Chapter 13
Exercise therapy
At the end of this chapter readers will be able to:
1 Understand the key principles of exercise.
2 Understand the prevalence and impact of three of the most common musculoskeletal pain problems.
3 Describe the key findings from best available evidence about the role of exercise as a core treatment for persistent musculoskeletal pain.
4 Understand the importance of the key characteristics of exercise programmes that help deliver better outcomes for patients.
OVERVIEW
Chronic or persistent musculoskeletal pain is a major health problem (White & Harth 1999) treated by many different healthcare providers. The most common types of chronic musculoskeletal pain are low back pain and joint pain related to osteoarthritis (Breivik et al 2006), including knee pain and hand pain. The primary prevention of these conditions has not proved feasible and modern management approaches, following biopsychosocial principles, are thus not orientated around a cure but rather around prevention of unnecessary disability and minimizing morbidity (Jordan et al 2010). It is clear that exercise, encompassing a wide range of interventions, such as general (aerobic) exercise, specific body-region exercises for strengthening, flexibility, control and balance, continuing normal physical activities and increasing general physical activity levels, is a core treatment option for those with musculoskeletal pain. Therapeutic exercise is one of the core skills upon which the physiotherapy profession is based, although many other health professionals are involved in advising and supporting patients in exercise and physical activity. This chapter focuses on the role of exercise in the management of persistent pain and provides a summary of the physiological and psychological principles for exercise before highlighting three specific examples of low back pain, knee pain and hand pain. The chapter then considers the particular importance of exercise adherence in realizing the potential of exercise therapy for improving the longer term outcomes of those with persistent pain before concluding with key implications for both clinical practice and future research.
KEY DEFINITIONS AND PRINCIPLES
Physical activity is any bodily movement produced by the skeletal muscles that results in energy expenditure (www.cdc.gov/nccdphp/dnpa/physical/terms). In contrast, exercise is planned, structured and repetitive movement to maintain or improve physical fitness (e.g. cardiovascular fitness, muscle strength, endurance, flexibility and body composition) and psychological well-being (ACSM 2006). Therapeutic exercise is the systematic implementation of planned physical movements, postures or activities to remediate or prevent impairments, and enhance function, fitness and well-being (APTA 2001). Whilst the focus of this chapter is therapeutic exercise for persistent musculoskeletal pain, where evidence is available to suggest that general physical activity and lifestyle changes have merit in achieving beneficial outcomes for patients these are also included.
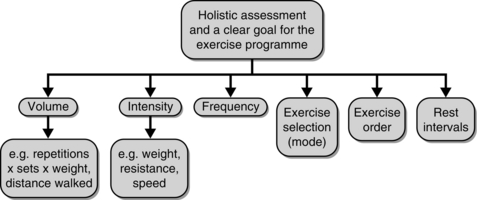
A therapeutic exercise programme for someone with persistent musculoskeletal pain may have several different goals, for example to improve function or reduce pain, to increase muscle strength, endurance or motor control, to improve range of movement or flexibility, or to help with coordination and balance. All goals should be mutually agreed between the patient and healthcare professional, and the selection of an appropriate exercise programme is informed by a holistic assessment of the patient, not only considering relevant subjective and objective clinical findings about the present condition but also about how the problem is affecting the individual, their general health (including other co-morbidities and other musculoskeletal pain), previous exercise experience and their attitude towards exercise. A number of design variables for the exercise programme must then be considered (Fig. 13.1), including the type of exercise prescribed, the volume of exercise (e.g. number of repetitions and sets of a strength exercise or walking distance), the intensity of exercise (e.g. weight for a resistance exercise or speed of a walking programme), and the frequency and duration of exercise (i.e. number of times the programme is completed per week over a specific period of time).
These design variables should be based on key physiological principles, provided in detail elsewhere (Glynn & Fiddler 2009, Hurley & Bearne 2009, McArdle et al 1996), but summarized below.
• Specificity: Any exercise will train a system for the particular task being carried out as the training stimulus. Hence, for example, it is important that an exercise aimed at muscle strengthening targets the correct muscle, in the range and using the type of muscle work specific to the task required.
• Overload: A system must be exercised at a level beyond that to which it is normally accustomed in order to achieve a training effect. Achieving the appropriate overload for an individual requires manipulation of the exercise programme design variables such as through increasing frequency, intensity, duration and mode of exercise. The choice of whether or not to use apply the overload principle must be based on an assessment of psychological variables (Chapters 4 and 7) and evidence of sensitization (Chapter 6). Patients with persistent pain may have to exercise little and often, in a time contingent manner.
• Adaptation: The system being exercised will gradually adapt to the overload or training stimulus, and this will continue as long as the training stimulus continues to be increased until the tissue or system can no longer adapt further.
• Individuality: Different individuals will respond to a given exercise training stimulus in different ways, and many factors contribute to individual variation in this training response. Training benefits are improved if the exercise programme is designed to meet the individual’s needs and capabilities.
• Reversibility: The beneficial effects of exercise are transient and reversible. They begin to be lost as soon as the exercise stimulus stops and this happens in a similar timeframe as it takes to train the system.
In addition, there are key psychological factors to take into consideration when prescribing an exercise programme for musculoskeletal pain patients, and whilst these tend to receive less attention than the physiological principles of exercise, they are important in determining whether an individual initially engages in, and continues with, exercise over time. In order to realize the benefits of exercise, effort and determination on the part of the individual is needed. Key psychological factors include motivation, self-efficacy to exercise (or confidence in their ability to perform tasks like exercise) and personal or internal control (Bandura 1977, 6, 7, 8). Thus, patient education alongside the therapeutic exercise programme is important to increase their understanding of the problem, challenge unhelpful beliefs about the problem and enhance the patient’s individual motivation and confidence to exercise. These aspects can be enhanced by designing exercise programmes in ways that take into consideration personal preferences (for example for individual or group-based exercise, or for the type of exercise), the potential benefits of peer support and social interaction, the importance of tailoring exercise for individual patients so that they can appreciate its relevance to their individual problem, agreeing specific and meaningful personal goals for the short and long term, and the role of supervision, review and positive reinforcement.
EXAMPLE 1: EXERCISE FOR PERSISTENT NON-SPECIFIC LOW BACK PAIN
The problem
Low back pain (LBP) is a very common condition, with lifetime prevalence rates as high as 84% (Walker 2000). In the UK, LBP is the fourth most common reason for consulting a GP after depression, hypertension and upper respiratory tract infection, and is the most common musculoskeletal reason for consultation. Estimates suggest that between 6 and 9% of people registered with a GP consult annually with LBP (Croft et al 1998, Dunn & Croft 2005), which equates to approximately five million people each year in the UK (Maniadakis & Gray 2000). In addition, many people seek care from musculoskeletal therapists, including physiotherapists, osteopaths and chiropractors. Even though it is a non-life threatening and largely self-limiting condition, LBP is responsible for large personal, societal and financial burdens as many patients with LBP develop persistent pain with a relapsing and recurrent pattern to their symptoms. The proportion of patients who continue to experience back pain 12 months after onset is reported to be in the region of 42–75% (Hestbaek et al 2003). It is now recognized that only a small proportion of persistent back pain can be attributed to a specific underlying disease or pathology. For patients with LBP presenting in primary care approximately 1% will have serious spinal pathology such as a systemic inflammatory condition or cancer, and around a further 5% will have nerve root pain/radicular pain (Waddell 2004). These patients often require specific diagnoses and management frequently involves onward referral to secondary care clinicians such as rheumatologists and orthopaedic surgeons. The remainder can be categorized as having non-specific LBP and most will be managed within primary care settings. The evidence synthesis presented below focuses on exercise for adults with persistent non-specific low back pain.
Clinical guidelines
Many clinical guidelines for the management of LBP have been developed in a number of different countries. The quality of clinical guidelines for the management of LBP is improving as time goes by (Bouwmeester et al 2009) and a synthesis of recent guidelines found that exercise is recommended in all the guidelines for persistent LBP (Dagenais et al 2010). The most recently published UK guidelines are the National Institute for Health and Clinical Excellence (NICE) guidance for the early management of persistent non-specific low back pain (NICE 2009). The guidelines recommend advising all patients presenting with persistent non-specific LBP to exercise, be physically active and to carry on with normal activities as much as possible. In addition, one of the three core treatments that the guidelines recommend is the provision of a structured exercise programme (a maximum of eight sessions over a period of up to 12 weeks). Exercise programmes may include aerobic activity, movement instruction, muscle strengthening and postural control, and the programme should be delivered in a group setting unless group exercise is considered inappropriate for a particular person.
Exercise for persistent non-specific LBP: the evidence
For example, the systematic review by Hayden et al (2005a) included 43 RCTs (3907 individuals) that investigated the effectiveness of exercise in people with persistent non-specific LBP. Strong evidence (consistent findings in multiple high-quality trials) was found that exercise therapy is as effective as other conservative interventions, although there was conflicting evidence (inconsistent findings in multiple trials) that exercise therapy is superior to other interventions. The meta-analyses showed pooled mean improvements in pain of 10.2 points (95% CI: 1.31 to 19.09) compared to no treatment and 5.93 points (95% CI: 2.21 to 9.65) compared to other conservative interventions. Pooled mean improvements in function were 3.00 points (95% CI: 0.53 to 6.48) compared to no treatment and 2.37 points (95% CI: 0.74 to 4.0) compared to other conservative interventions. The exercise interventions that showed better outcomes than comparison interventions were generally based in healthcare rather than general population settings, were designed and delivered with individual patients, and commonly included strengthening and trunk stability exercises.
In a later systematic review, only higher quality studies of exercise therapy were included to overcome some of the difficulties resulting from including studies with methodological limitations (Hettinga et al 2007). The results indicated that inclusion of smaller RCTs in systematic reviews leads to overestimation of effectiveness. The higher quality studies support the use of exercise, particularly strengthening exercises, aerobic exercises, general exercises, hydrotherapy and McKenzie exercises for individuals with persistent pain. Further support that exercise is beneficial for LBP is provided by the systematic review by Macedo et al (2009), who also highlighted that no one type of exercise appears superior. Motor control exercise for LBP was superior to minimal intervention, with mean differences in pain scores at short term, medium term and long term of − 14.3 (95% CI: − 20.4 to − 8.1), − 13.6 (95% CI: − 22.4 to − 4.1) and − 14.4 (95% CI: − 23.1 to − 5.7), respectively. Improvements in function were also seen but at long-term follow-up only, with a difference to the comparison groups of − 10.8 (95% CI: − 18.7 to − 2.8). However, motor control exercise was not more effective than other forms of exercise for LBP.
A further comprehensive review of RCTs for persistent non-specific LBP included 37 RCTs (3957 individuals) (van Middelkoop et al 2010). Compared to usual care, exercise therapy improved post-treatment pain intensity and disability, and long-term function. The review concluded that evidence from RCTs demonstrates that exercise is effective for persistent LBP, that the effects tend to be small, that there is no evidence that one particular type of exercise is clearly more effective than others and that it is still unclear which patients benefit most from which type of exercise. Of 11 studies that compared different exercise interventions, only two studies found statistically significant differences in pain and disability outcomes. Aerobic exercise was found to be better than a flexion exercise regime in one low-quality study and motor control exercise was shown to be slightly better than general exercises in one high-quality study. Pooling of data was not undertaken due to the heterogeneity of the interventions in these studies.
In addition to specific exercise regimes, graded activity and graded exposure have been shown to be superior to minimal intervention in both the short and medium term on improving pain (pooled mean change at short term − 6.2 95% CI: − 9.4 to − 3.0, medium term − 5.5 95% CI: − 9.9 to − 1.0) and disability (pooled mean change at short term − 6.5 95% CI: − 10.1 to − 3.0, medium term − 3.9 95% CI: − 7.4 to − 0.4) in individuals with persistent non-specific LBP. However, graded activity and exposure were not better when compared to other forms of exercise (Macedo et al 2010).
Effect of exercise on work disability
Intensive exercise interventions that include aerobic capacity, muscle strength, endurance and coordination training, and have some relation to the work environment have been shown, in a systematic review, to reduce the number of sick days in employed individuals with persistent LBP (Schonstein et al 2003). However, the interventions included in this review also incorporated cognitive–behavioural approaches. More recently, a systematic review and meta-analysis of 23 RCTs showed a statistically significant effect of exercise on work disability in the long term (odds ratio 0.66 95%CI: 0.48 to 0.92), but not short or medium term, compared to usual care or other exercise interventions (Oesch et al 2010). Again there was no evidence of the superiority of any particular type of exercise. In addition, a small effect on sickness absence was found in pooled results (mean difference of − 0.18 95%CI: − 0.37 to 0.0) of five studies of physical conditioning in workers with persistent non-specific LBP, although conflicting results were found when compared to other exercise interventions (Schaafsma et al 2010).
Factors improving outcomes with exercise
Exercise therapy incorporates a wide range of heterogeneous interventions which in addition to the type of exercise can vary in terms of duration, frequency, setting, dosage and supervised or home-based programmes. A Bayesian meta-regression of 43 trials, where the characteristics of exercise interventions providing the best outcomes were examined, concluded that exercise interventions are more effective when individually designed rather than standardized, when exercise programmes were supervised and when programmes were carried out over longer time periods (Hayden et al 2005b). A separate examination of the impact of a variety of study characteristics on the small but significant improvements of pain and disability seen in included trials showed that only exercise dosage was significantly associated with effect sizes (Ferreira et al 2010).
EXAMPLE 2: EXERCISE FOR KNEE PAIN IN OLDER ADULTS
The problem
Knee pain is a common musculoskeletal complaint caused by both acute injuries such as meniscal tears and ligament ruptures, and chronic conditions such as patellofemoral pain syndrome, rheumatoid arthritis and osteoarthritis. Knee problems in older adults are particularly common, with estimates suggesting that approximately 25% of adults aged 55 years and over suffer with knee pain (Peat et al 2001a). This prevalence is likely to continue to rise as the population ages (Wilmoth 2000) and as levels of obesity, a risk factor, continue to grow (James 2008). Most knee pain in older adults is likely to be attributable to osteoarthritis (OA). Traditionally, OA was believed to be a progressive, degenerative disease, but it is now viewed as a dynamic repair process involving all joint tissues, including cartilage, bone, ligament and muscle (NICE 2008; Peat et al 2001b). There is some discordance between the extent of X-ray changes and clinical symptoms of OA, which can make the diagnosis of ‘OA’ difficult (Peat et al 2006). Recent UK national guidelines (NICE 2008) propose the following working clinical diagnosis of peripheral joint OA: patients aged 45 and over, with persistent joint pain that is worse with use, and morning stiffness lasting no more than half an hour (NICE 2008). Therefore, this evidence synthesis focuses on exercise for ‘knee pain’, with the assumption that most older adults with this condition will have a clinical problem of OA, and some will have radiographic changes in the relevant joints.
Persistent knee pain can have a considerable impact at an individual level. Pain, joint stiffness, instability, swelling and muscle weakness can contribute to functional limitations, psychological distress and reduced quality of life (Bennell & Hinman 2011; Hurley 2003; Jordan et al 2003; Neame & Doherty 2005). It can also have wider societal implications. For example, within the UK between 1999 and 2000, £43 million was spent on community services for OA, including patients with knee pain (NICE 2008), and each year 2 million adults visit their GP because of OA (Arthritis Research UK 2002).
Clinical guidelines
Many guidelines now exist to try and optimize health care for patients with knee pain, all of which recommend exercise as a frontline treatment (Zhang et al 2007b). The most recent UK guidelines are the NICE Osteoarthritis Guidelines (NICE 2008). They state that three core treatments should be considered first for every patient with OA: advice and education to enhance understanding of the condition, interventions to achieve weight loss if the person is overweight or obese, and activity and exercise, including local muscle strengthening and general aerobic fitness (NICE 2008). A multidisciplinary group have also developed a set of recommendations that address specific questions about the role of exercise in knee and hip OA, summarized in Table 13.1 (Roddy et al 2005a). These incorporate research-based evidence and expert opinion to evaluate ten propositions about the role of exercise, such as the benefit of specific types of exercises and predictors of response.
Table 13.1
Summary of the 10 propositions included in the exercise recommendations for hip and knee OA
| Proposition | Category of evidence (1–41) | Strength of recommendation (A–D2) |
| Both strengthening and aerobic exercise can reduce pain and improve function and health status in patients with hip and knee OA | Knee 1B Hip 4 | A C (extrapolated from knee OA) |
| There are few contraindications to the prescription of strengthening or aerobic exercise in patients with hip or knee OA | 4 | C (extrapolated from adverse event data) |
| Prescription of both general (aerobic fitness training) and local (strengthening) exercises is an essential, core aspect of management for every patient with hip or knee OA | 4 | D |
| Exercise therapy for OA of the hip or knee should be individualized and patient-centred, taking into account factors such as age, co-morbidity and overall mobility | 4 | D |
| To be effective, exercise programmes should include advice and education to promote a positive lifestyle change with an increase in physical activity | 4* 1B | D A |
| Group exercise and home exercise are equally effective and patient preference should be considered | 1A** 4 | A D |
| Adherence is the principal predictor of long-term outcome from exercise in patients with hip or knee OA | 4 | D |
| Strategies to improve and maintain adherence should be adopted, e.g. long-term monitoring/review and inclusion of spouse/family in exercise | 1B | A |
| The effectiveness of exercise is independent of the presence or severity of radiographic findings | 4 | Not recommended |
| Improvements in muscle strength and proprioception (balance) gained from exercise programmes may reduce the progression of hip and knee OA | 4 | D |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree