Chapter 5 Ethical Dilemmas in Emergency Nursing
Ethical Frameworks for Decision Making1,2
Ethical frameworks assist in clarifying values and beliefs. Table 5-1 lists some of the most common ethical frameworks used in decision making.
| FRAMEWORK | BASIC PREMISE | EXAMPLE |
|---|---|---|
| Utilitarian | Provide the greatest good for the greatest number of people | Disaster scenario |
| Rights-based | Individuals share basic inherent rights that should not be interfered with | Right to refuse |
| Duty-based | A duty to do something or to refrain from doing something | Nurse does not scream back when a patient is yelling at the nurse |
| Intuitionist | Each case weighted on a case-by-case basis to determine relative goals, duties, and rights | Should a patient with severe lung disease be put on a mechanical ventilator when there is little chance of successful weaning? |
Principles1–3
• Autonomy: self-determination or freedom of choice
• Utility: good of many outweighs the wants and needs of the individual
• Fidelity: keeping promises, loyalty, and accountability
Code of Ethics
Professional codes of ethics do not have the power of law; however, they do provide a guide for nursing practice, providing implicit standards and values for the profession. ANA’s Code of Ethics has existed since 1950. The current 2001 edition includes the following concepts6:
• Specifically indicating that the most fundamental accountability is to the patient
• Assuring that the workplace is safe
Table 5-2 lists the provision statements guiding the nursing practice in the ANA’s Code of Ethics.
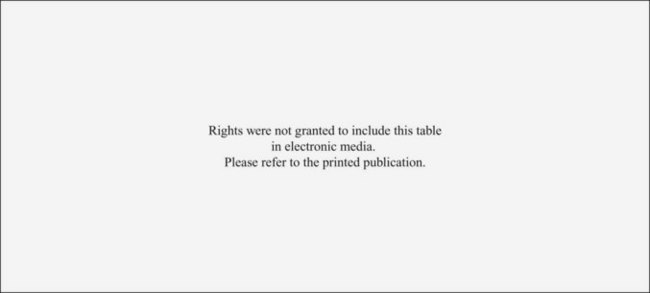
TABLE 5-2 ANA CODE OF ETHICS PROVISIONS
Rights were not granted to include this table in electronic media. Please refer to the printed book.
Reproduced with permission of the American Nurses Association.








