![]() Used to decompress accumulated edema under tight, unyielding eschar following full-thickness burn (classic and modern classifications of burns are given in TABLE 74.1)
Used to decompress accumulated edema under tight, unyielding eschar following full-thickness burn (classic and modern classifications of burns are given in TABLE 74.1)
![]() Circumferential extremity burn with evidence of neurovascular compromise:
Circumferential extremity burn with evidence of neurovascular compromise:
![]() Cyanosis
Cyanosis
![]() Deep tissue pain
Deep tissue pain
![]() Progressive paresthesia
Progressive paresthesia
![]() Decreased or absent pulses
Decreased or absent pulses
![]() Elevated compartment pressure
Elevated compartment pressure
![]() Decreased arterial flow on Doppler ultrasonography
Decreased arterial flow on Doppler ultrasonography
![]() Pulse oximetry <95% of affected extremity (without systemic hypoxia)
Pulse oximetry <95% of affected extremity (without systemic hypoxia)
![]() Thoracic burn with evidence of respiratory compromise due to eschar
Thoracic burn with evidence of respiratory compromise due to eschar
![]() Circumferential neck burn
Circumferential neck burn
![]() Abdominal burn with evidence of increased intra-abdominal pressure (usually estimated by bladder pressure)
Abdominal burn with evidence of increased intra-abdominal pressure (usually estimated by bladder pressure)
![]() Circumferential penile burn
Circumferential penile burn
CONTRAINDICATIONS
![]() No evidence of tissue hypoperfusion on physical examination
No evidence of tissue hypoperfusion on physical examination
![]() Normal findings on arterial Doppler ultrasonography
Normal findings on arterial Doppler ultrasonography
![]() Adequate respiration despite eschar
Adequate respiration despite eschar
![]() No evidence of increased intra-abdominal pressure
No evidence of increased intra-abdominal pressure
RISK/CONSENT ISSUES
![]() Often difficult to obtain consent from major burn victims; escharotomy is a life-saving procedure and should be performed even if informed consent from the patient cannot be obtained
Often difficult to obtain consent from major burn victims; escharotomy is a life-saving procedure and should be performed even if informed consent from the patient cannot be obtained
![]() Procedure can cause pain (local and systemic analgesia will be provided)
Procedure can cause pain (local and systemic analgesia will be provided)
![]() Risk of bleeding (minimized with proper technique)
Risk of bleeding (minimized with proper technique)
![]() Whenever the skin is broken, there is potential for introducing infection (sterile technique will be utilized)
Whenever the skin is broken, there is potential for introducing infection (sterile technique will be utilized)
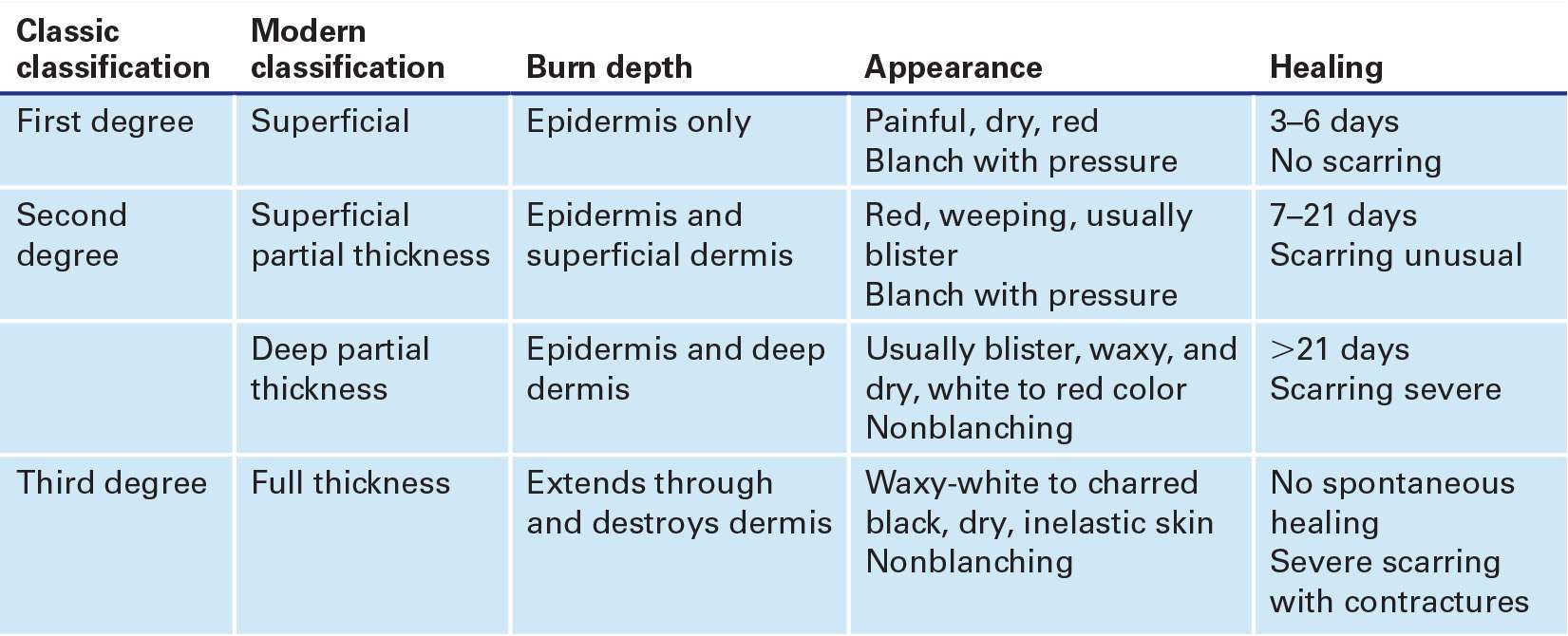
BURN DEPTH CLASSIFICATION |
LANDMARKS
Escharotomy sites are depicted in FIGURE 74.1.
TECHNIQUE
![]() General Basic Steps
General Basic Steps
![]() Airway, breathing, and circulation (ABC)
Airway, breathing, and circulation (ABC)
![]() Consider early intubation
Consider early intubation
![]() Fluid resuscitation
Fluid resuscitation
![]() Analgesia
Analgesia
![]() Tetanus prophylaxis
Tetanus prophylaxis
![]() Wound care
Wound care
![]() Escharotomy
Escharotomy
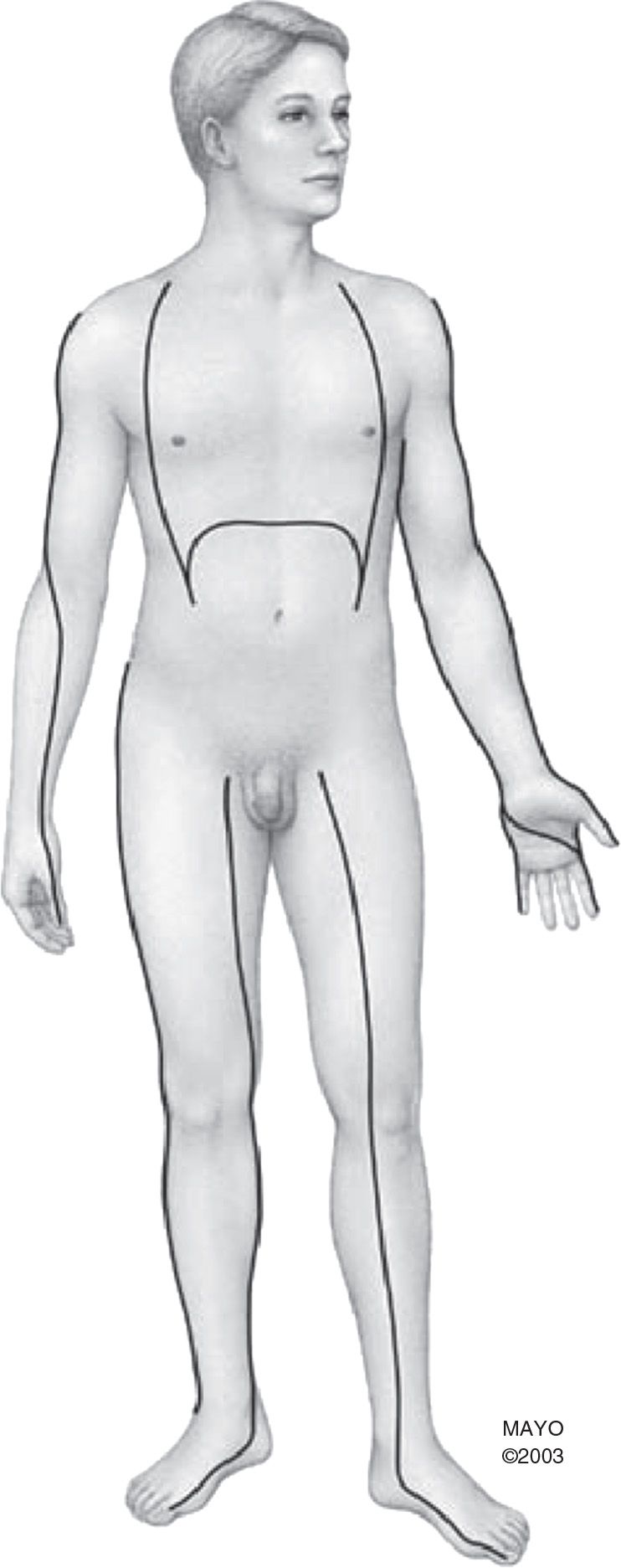
FIGURE 74.1 Escharotomy sites. (From Haro LH, Miller S, Decker WW. Burns. In: Wolfson AB, ed. Harwood-Nuss’ Clinical Practice of Emergency Medicine. 6th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2014:315, with permission.)
BURN MANAGEMENT
![]() First ensure ABC and administer supplemental oxygen
First ensure ABC and administer supplemental oxygen
![]() Strongly consider endotracheal intubation if:
Strongly consider endotracheal intubation if:
![]() Burns to the face and neck are present
Burns to the face and neck are present
![]() Soot in and around the mouth and nose
Soot in and around the mouth and nose
![]() Hoarseness, stridor, wheezing, or development of acute coughing
Hoarseness, stridor, wheezing, or development of acute coughing
![]() Carbonaceous sputum
Carbonaceous sputum
![]() Give intravenous fluids for resuscitation (for moderate to major burns)
Give intravenous fluids for resuscitation (for moderate to major burns)
![]() Use Parkland formula: Ringer lactate 4 mL × weight (kg) × % of total body surface area (TBSA) burned (excluding superficial burns)
Use Parkland formula: Ringer lactate 4 mL × weight (kg) × % of total body surface area (TBSA) burned (excluding superficial burns)
![]() Give ½ of total volume over the first 8 hours from time of burn injury
Give ½ of total volume over the first 8 hours from time of burn injury
![]() Give second ½ of total volume over the following 16 hours
Give second ½ of total volume over the following 16 hours
![]() Titrate to maintain blood pressure and urine output of at least 1 mL/kg/hour
Titrate to maintain blood pressure and urine output of at least 1 mL/kg/hour
![]() Continue maintenance fluids in addition
Continue maintenance fluids in addition
![]() Place urinary catheter to monitor adequate resuscitation (FIGURE 74.2)
Place urinary catheter to monitor adequate resuscitation (FIGURE 74.2)
![]() Provide pain management with frequent pain assessment
Provide pain management with frequent pain assessment
![]() Acetaminophen and nonsteroidal anti-inflammatory drugs (NSAIDS) with or without opioids for superficial burns
Acetaminophen and nonsteroidal anti-inflammatory drugs (NSAIDS) with or without opioids for superficial burns
![]() Opioids are necessary for partial-to-full thickness burns
Opioids are necessary for partial-to-full thickness burns
![]() Administer tetanus prophylaxis
Administer tetanus prophylaxis
![]() Wound care, if not delaying transfer to burn unit:
Wound care, if not delaying transfer to burn unit:
![]() Use sterile technique
Use sterile technique
![]() Clean with mild soap and tap water
Clean with mild soap and tap water
![]() Debride sloughed or necrotic skin; avoid extensive debridement
Debride sloughed or necrotic skin; avoid extensive debridement
![]() Remove ruptured blisters
Remove ruptured blisters
![]() Intact blister management is controversial; it is recommended to unroof cloudy blisters or those where rupture is imminent (e.g., over joints)
Intact blister management is controversial; it is recommended to unroof cloudy blisters or those where rupture is imminent (e.g., over joints)
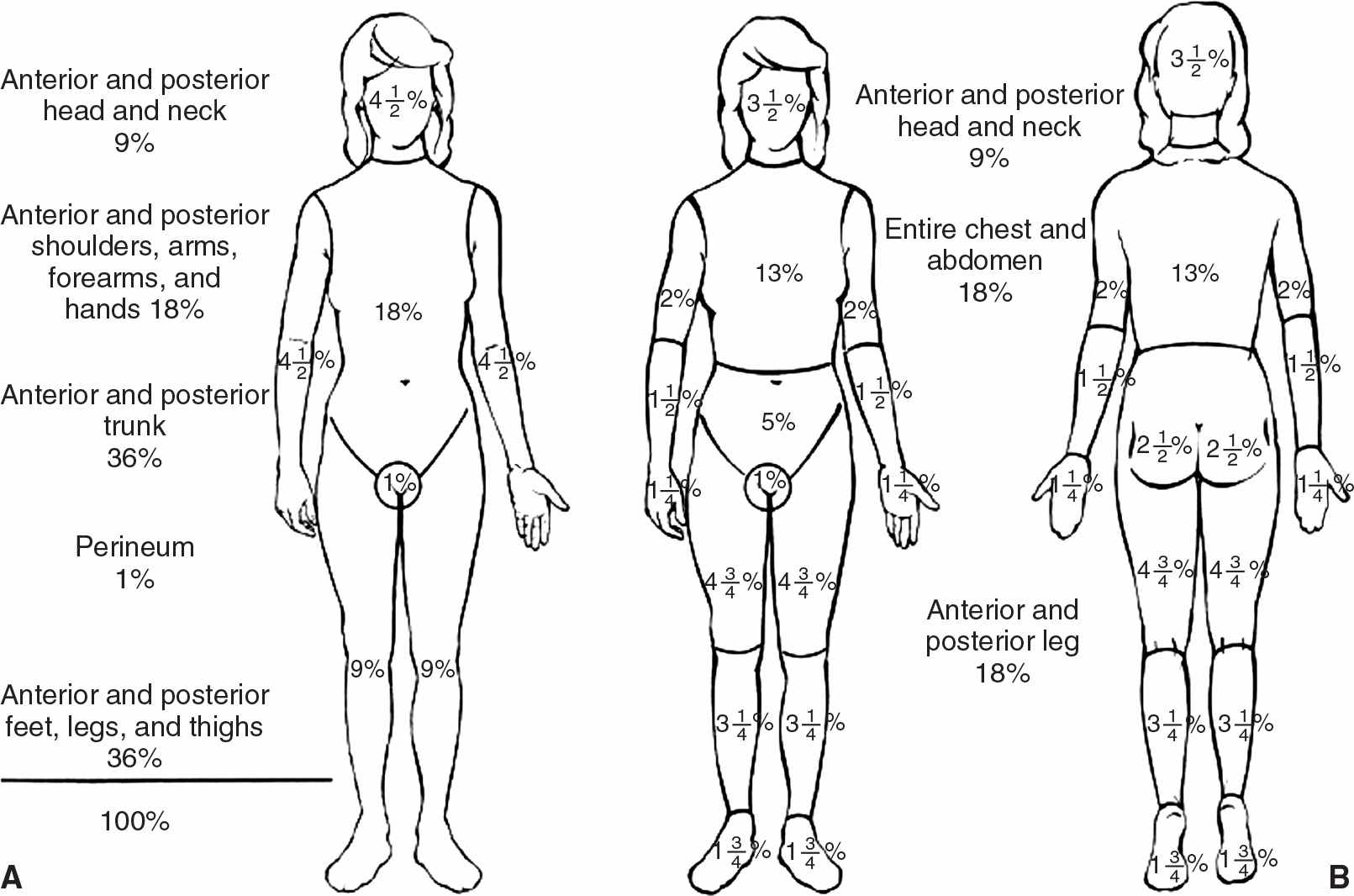
FIGURE 74.2 Methods to evaluate percentage of body surface area burned. A: Rule of Nines. B: Lund and Browder chart. (From Haro LH, Miller S, Decker WW. Burns. In: Wolfson AB, ed. Harwood-Nuss’ Clinical Practice of Emergency Medicine. 6th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2014:1103, with permission.)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


