![]() To prevent severe spontaneous third- and fourth-degree perineal lacerations
To prevent severe spontaneous third- and fourth-degree perineal lacerations
![]() To increase the diameter of the soft-tissue pelvic outlet to relieve shoulder dystocia
To increase the diameter of the soft-tissue pelvic outlet to relieve shoulder dystocia
![]() To facilitate delivery of fetus having nonreassuring fetal heart-rate tracings
To facilitate delivery of fetus having nonreassuring fetal heart-rate tracings
![]() To facilitate delivery in malpresentations, including breech and occiput posterior presentations
To facilitate delivery in malpresentations, including breech and occiput posterior presentations
CONTRAINDICATIONS
![]() Not recommended for routine delivery, especially in the primiparous patient
Not recommended for routine delivery, especially in the primiparous patient
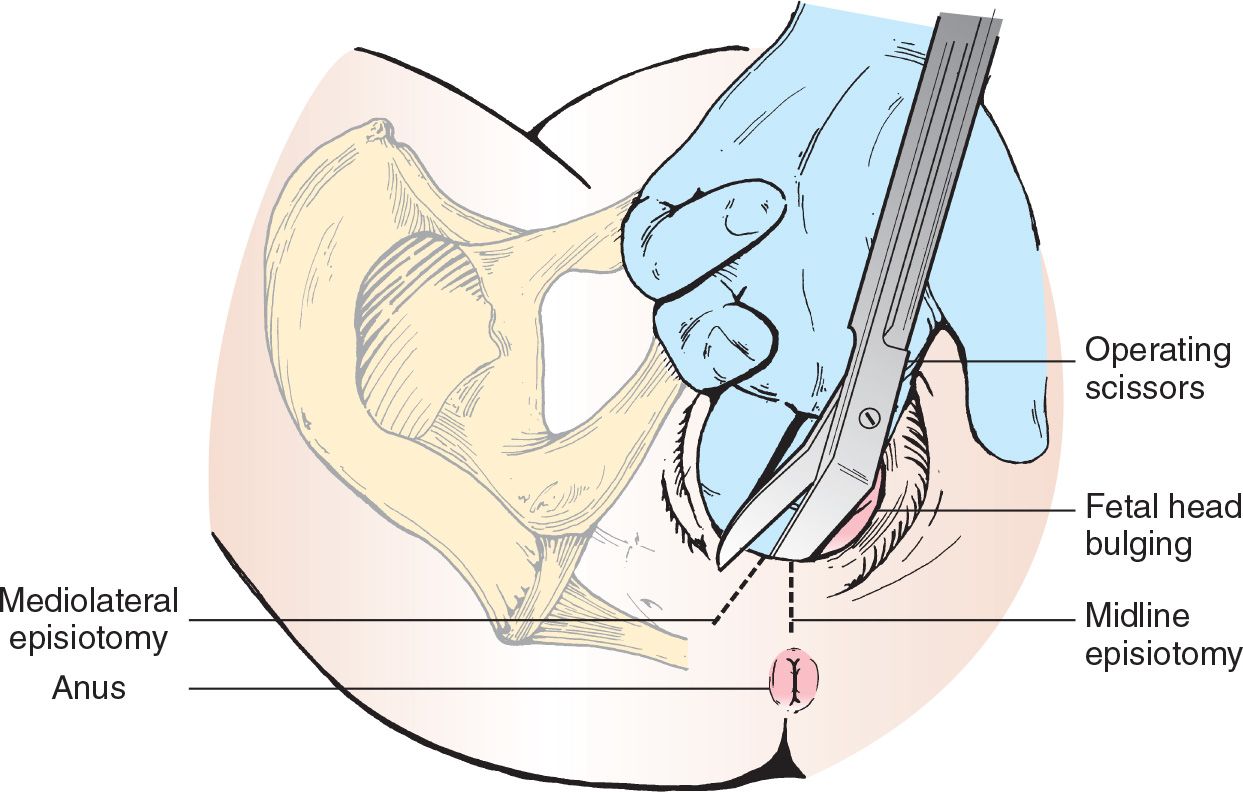
LANDMARKS (FIGURE 43.1)
![]() General Basic Steps
General Basic Steps
![]() Organize supplies
Organize supplies
![]() Local anesthesia
Local anesthesia
![]() Incision
Incision
![]() Closure
Closure
TECHNIQUE
![]() Supplies
Supplies
![]() A 3-0 or 2-0 absorbable suture (polyglactin preferred or chromic catgut) on atraumatic needle
A 3-0 or 2-0 absorbable suture (polyglactin preferred or chromic catgut) on atraumatic needle
![]() Needle holder
Needle holder
![]() Tissue scissors or scalpel
Tissue scissors or scalpel
![]() Suture scissors
Suture scissors
![]() Gauze
Gauze
![]() Local anesthesia and injection materials
Local anesthesia and injection materials
![]() Initiation of Procedure
Initiation of Procedure
![]() For vertex presentations, episiotomy is started when the fetal head begins to stretch the perineum and when 3 to 4 cm diameter of the caput is visible during a contraction (prior to crowning)
For vertex presentations, episiotomy is started when the fetal head begins to stretch the perineum and when 3 to 4 cm diameter of the caput is visible during a contraction (prior to crowning)
![]() For breech presentations, episiotomy is started just before extraction of the fetus
For breech presentations, episiotomy is started just before extraction of the fetus
![]() Inject 1% or 2% lidocaine locally in the perineum where episiotomy is planned (may also perform pudendal nerve block) (FIGURE 43.2)
Inject 1% or 2% lidocaine locally in the perineum where episiotomy is planned (may also perform pudendal nerve block) (FIGURE 43.2)
![]() Median or Midline Technique
Median or Midline Technique
![]() Most commonly performed
Most commonly performed
![]() Just prior to crowning, two fingers are placed inside the vaginal introitus to expose the mucosa, posterior fourchette, and the perineal body
Just prior to crowning, two fingers are placed inside the vaginal introitus to expose the mucosa, posterior fourchette, and the perineal body
![]() Tissue scissors are used to make a vertical incision beginning at the fourchette and extending caudally in the midline. The goal is to release the constriction caused by the perineal body.
Tissue scissors are used to make a vertical incision beginning at the fourchette and extending caudally in the midline. The goal is to release the constriction caused by the perineal body.
![]() Incision should be directed internally to minimize the amount of perineal skin incised
Incision should be directed internally to minimize the amount of perineal skin incised
![]() Incision includes the vaginal mucosa, perineal body, and the junction of the perineal body with the bulbocavernosus muscle in the perineum
Incision includes the vaginal mucosa, perineal body, and the junction of the perineal body with the bulbocavernosus muscle in the perineum
![]() Mediolateral Technique
Mediolateral Technique
![]() As the head crowns, two fingers are placed inside the vaginal introitus to expose the mucosa, posterior fourchette, and the perineal body
As the head crowns, two fingers are placed inside the vaginal introitus to expose the mucosa, posterior fourchette, and the perineal body
![]() Tissue scissors are used to make a 3- to 5-cm incision directed downward and outward toward the lateral margin of the anal sphincter in a 45-degree angle. This incision may be either to the left or the right.
Tissue scissors are used to make a 3- to 5-cm incision directed downward and outward toward the lateral margin of the anal sphincter in a 45-degree angle. This incision may be either to the left or the right.
![]() Incision includes the vaginal mucosa, transverse perineal and bulbocavernosus muscles, and the perineal skin
Incision includes the vaginal mucosa, transverse perineal and bulbocavernosus muscles, and the perineal skin
![]() Repair: Layer Closure
Repair: Layer Closure
![]() A 2-0 or 3-0 absorbable suture is used
A 2-0 or 3-0 absorbable suture is used
![]() Close the vaginal mucosa using a continuous suture from just above the apex of the incision to the mucocutaneous junction
Close the vaginal mucosa using a continuous suture from just above the apex of the incision to the mucocutaneous junction
![]() Burying the closing knot minimizes the amount of scar tissue and prevents pain and dyspareunia
Burying the closing knot minimizes the amount of scar tissue and prevents pain and dyspareunia
![]() Large actively bleeding vessels may require ligation with separate absorbable sutures
Large actively bleeding vessels may require ligation with separate absorbable sutures
![]() The perineal musculature is reapproximated using three to four interrupted sutures
The perineal musculature is reapproximated using three to four interrupted sutures
![]() Closure of the superficial layers is done with several interrupted sutures through the skin and subcutaneous fascia that are loosely tied. The skin can also be closed using a running subcuticular suture.
Closure of the superficial layers is done with several interrupted sutures through the skin and subcutaneous fascia that are loosely tied. The skin can also be closed using a running subcuticular suture.
![]() Finally, examine the rectum and anal sphincters with the index finger in the rectum and the thumb on the sphincter, using a pill-rolling motion to assess integrity (FIGURE 43.3)
Finally, examine the rectum and anal sphincters with the index finger in the rectum and the thumb on the sphincter, using a pill-rolling motion to assess integrity (FIGURE 43.3)
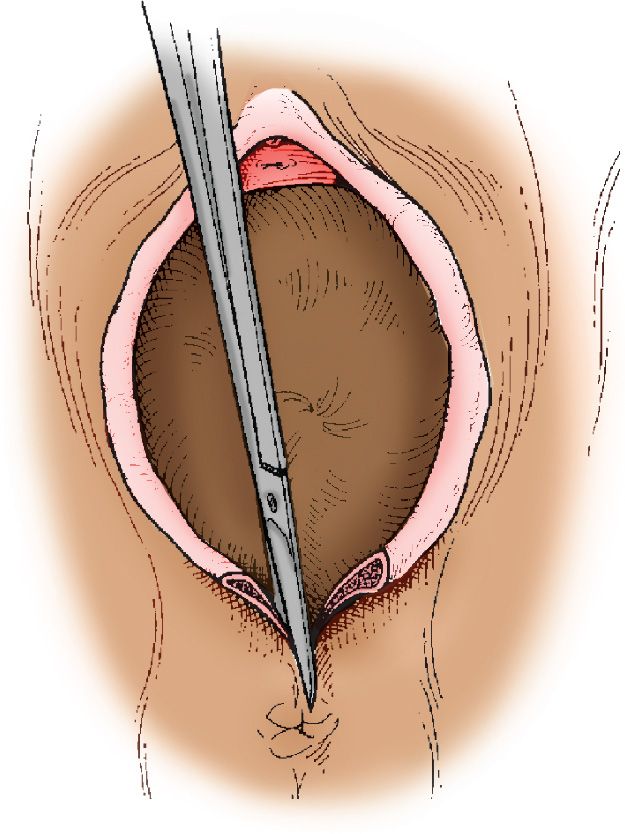
FIGURE 43.2 Midline episiotomy. As the fetal head distends, with the perineum under adequate anesthesia, a cut is made through the perineal body and the tissues of the vagina and the rectovaginal septum for the episiotomy. (From Rouse DJ, St John E. Normal labor, delivery, newborn care, and puerperium. In: Scott JR, Gibbs RS, Karlan BY, et al. eds. Danforth’s Obstetrics and Gynecology. 9th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2003:44, with permission.)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree