Lisa M. O’Neal
Epiglottitis
![]() Immediate emergency department referral or physician consultation is indicated for patients with suspected epiglottitis.
Immediate emergency department referral or physician consultation is indicated for patients with suspected epiglottitis.
Definition and Epidemiology
Epiglottitis (supraglottitis) is an acute inflammation of the supraglottic region of the oropharynx. Epiglottitis is characterized by inflammation and edema of the epiglottis, vallecular, arytenoids, and aryepiglottic folds.1 Owing to the high vascularity and loose mucosa of the epiglottic region, sudden airway obstruction and possible death can result.1 Epiglottitis is typically caused by a bacterial infection and less commonly results from a viral illness or caustic and thermal injury to the epiglottis. Thermal epiglottitis is a rare and potentially life-threatening disease caused by direct thermal injury or inhalation of steam or aspiration of heated liquids.2,3 Crack cocaine use has been associated with thermal injury to the hypopharynx in teens and young adults.4
Epiglottitis is a rare but serious life-threatening condition because of the potential for laryngospasm and irrevocable loss of the airway.5 From the 1950s to the early 1990s, epiglottitis typically occurred more often in children than in adults. The most common bacterial pathogen responsible for epiglottitis in children was Haemophilus influenzae type B (Hib). More recently, however, the incidence of epiglottitis in adults has shown a steady increase and is approximately 2.5 times greater than that in children.5 In the United States, epiglottitis in adults is estimated to be 1.9 in 100,000 per year.5 The dramatic decline in childhood epiglottitis is due to the advent of the vaccination for Haemophilus organisms. Overall, the incidence is now decreasing in all age groups, possibly as a result of a general decrease of Hib disease in the general population. It should be noted however, that a recent case report found H. influenzae type A as the responsible pathogen for severe invasive disease in countries with an Hib vaccination program.6 Other pathogens associated with epiglottitis include groups A, B, and C streptococci; Streptococcus pneumoniae; Klebsiella pneumoniae; Candida albicans; Staphylococcus aureus; Haemophilus parainfluenzae; Neisseria meningitidis; varicella-zoster virus; and various other viral pathogens.7
Male predominance is reported with epiglottitis; however, male/female ratios have varied. The mean age of adults with epiglottitis is 44.94 years.8 There is no seasonal predilection for epiglottitis; however, two studies have shown an increase in cases during the summer months.5
Epiglottitis among adults may follow an unpredictable clinical course, ranging from relatively benign disease to rapidly progressive disease with acute airway obstruction and possibly death. The mortality rate for children is less than 1%, but the mortality rate for the adult population is in the range of 6% to 7%.9
Pathophysiology
Epiglottitis can be caused by a variety of microorganisms. In the postvaccine era, for children younger than age 5, Hib continues to be an important cause of epiglottitis.6 In patients with underlying disease, Aspergillus, Klebsiella, and Candida organisms have been identified. A viral cause has been postulated for some cases of adult epiglottitis, especially the milder cases, although it is traditionally associated with infectious organisms. Investigators have identified noninfectious causes of epiglottitis, which can include inflammation in association with thermal injury (crack cocaine and marijuana smoking), ingestion of caustic substances (automatic dishwashing detergent), systemic disease (diabetes mellitus, hypertension, obstructive pulmonary disease, seizure disorder, alcohol and drug abuse, tobacco smoking), chemotherapy for head and neck cancer, trauma by foreign objects, and burns associated with bottle-fed infant formula.5,8,10
Clinical Presentation
Patients with epiglottitis are initially seen with an acute occurrence of severe odynophagia, dysphagia, fever, and shortness of breath with sitting up and leaning forward in an effort to enhance air flow.10 Other complaints include the inability to swallow their own secretions, neck tenderness, lymphadenopathy, cough, drooling, stridor, respiratory distress, and hoarseness. The patient may adopt the tripod position (leaning forward with hands braced on the knees), using accessory muscles for respiration.5 Dyspnea and stridor are common signs of epiglottitis in children, whereas odynophagia, dysphagia, and voice change are common presenting symptoms in adults.10 The onset and duration of symptoms before the patient’s initial contact with the health care provider vary. Depending on the severity of symptoms, patients may seek treatment after having symptoms for less than 8 hours, or they may have had them for more than 4 days.
Physical Examination
Patients with epiglottitis may or may not have fever and a toxic appearance, depending on the severity of the infection or the cause of the inflammation. Generalized toxemia is a result of acute epiglottitis.10 If assessment of the adult patient reveals the presence of anterior neck tenderness with severe sore throat, epiglottitis should be suspected.5 Patients experiencing respiratory distress, posturing in the upright “sniff” or tripod position, dysphagia, and refusal to swallow are all reliable signs of epiglottitis.5 Indirect laryngoscopy may reveal an erythematous, edematous epiglottis with a narrow glottic opening. Substernal and supraclavicular retractions, tachycardia, tachypnea, and inspiratory stridor are common. With severe respiratory distress, changes in mental status, anxiety, pallor, cyanosis, and other signs of hypoxia may be present.
Precautions during the physical examination are required. If epiglottitis is suspected, the pharynx should not be examined with a tongue depressor, because this may precipitate an airway emergency. Any inspection of the oral cavity requires that emergency airway management equipment be immediately available in case of laryngospasm; laryngospasm can cause sudden airway occlusion.
Diagnostics
The gold standard for a definitive diagnosis of epiglottitis is made by direct visualization via laryngoscopy with a flexible fiberoptic scope or a laryngeal mirror.11 It provides accurate visualization of the epiglottis and it shows the extent of epiglottic swelling.5 Indirect laryngoscopy is considered a safe diagnostic tool in the adult population but not in children.12 A recent study showed that sonography is an accurate, noninvasive, and rapid diagnostic tool for epiglottitis in the emergency setting.9 A positive diagnosis of epiglottitis is achieved by evaluating the diameter of the anteroposterior diameter of the epiglottis.9
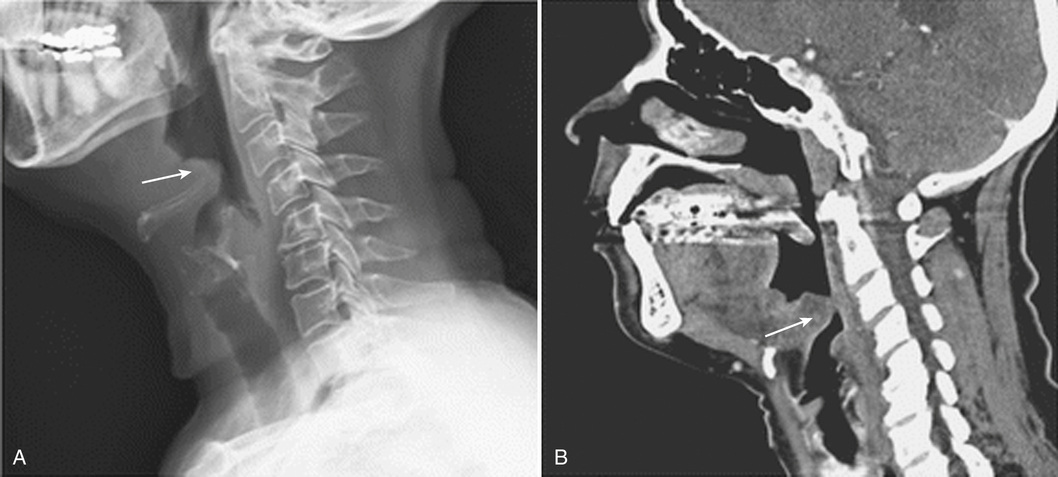
A lateral neck film can be useful but is not always diagnostic in the adult population.11 Findings on the lateral neck film suggestive of epiglottitis include a swollen epiglottis manifesting as a “thumbprint” sign (Fig. 97-1).13 Because they have a low sensitivity rate (true positives), lateral neck films are not a true diagnostic tool and are being replaced with direct visualization of the epiglottis with fiberoptic nasopharyngoscopy.11 It should be noted that if the thumbprint sign is present, it is a significant predictor for imminent airway compromise and rapid clinical deterioration.10 Prophylactic airway management is not indicated for an adult with epiglottitis; however, securing the airway should take precedence over the performance of laboratory examinations or radiologic studies.3 Computed tomography (CT) and magnetic resonance imaging (MRI) are not commonly used for the diagnosis of epiglottitis; however, they are useful in the evaluation of complications (infection and abscess formation) of epiglottitis.5