1 Epidemiology of Spinal Injuries Darric E. Baty, Howard B. Levene, Stephen V. Nalbach, Eli M. Baron, and Devanand A. Dominique Spinal cord injury (SCI) encompasses more than just the direct injury to the tissues of the spinal cord itself. The injury creates a range of disabilities and hurdles, encompassing everything from physical limitations to social embarrassment. In the United States, there are more than 200,000 people living with chronic SCI.1 People with SCI suffer losses, physical and mental, with far-reaching impact on their ability to work and socialize. The effects of SCI involve families that now must care for a loved one with a potentially disabling neurologic condition; they most readily feel the costs, financial and personal, associated with SCI. Although not every injury is severe enough to make the injured person appear abnormal, the effects of SCI are felt by nearly all these families in the form of elevated health care costs, rising insurance premiums, and safety laws.1 It was not so long ago when SCI was considered a death sentence and a condition not worthy of treatment. Sir Ludwig Guttmann and Sir George Bedbrook were responsible for dramatically changing the way SCI was perceived by the medical community.2 Guttmann was a German who left his country for England in the 1930s when National Socialism gained favor in Germany. He was trained as a neurosurgeon and worked in basic science research at the beginning of World War II. He was therefore assigned the “hopeless” SCI cases in Stoke-Mandeville Hospital, because it was felt he could do “little harm.” The hospital was actually separate from the other military hospitals, a place where SCI patients could “go to die.” Guttmann used his neurologic and surgical knowledge to establish many of the principles of rehabilitative care; he is in fact considered one of the fathers of modern rehabilitation.2 Guttmann learned through experience and observation that laminectomies in the acute phase of SCI were indeed harmful, and thus he became a strong advocate of conservative management of SCI. He was referred patients from other hospitals and saw many complications, such as bed sores and infections; therefore, he insisted on direct admission of all SCI patients to his unit. With a team approach and insistence on 24-hour care, Guttmann emphasized avoidance of complications and therefore achieved astonishing results. Many of his patients returned to their homes and a productive life, taking up jobs that were suitable for their neurologic conditions.2 A short time later, Bedbrook, an orthopedist from Australia, also obtained excellent results from aggressive conservative care by utilizing a host of therapists and medical specialists devoted to complete care of the SCI patient. He, too, gained recognition as one of the fathers of modern rehabilitation and helped to further the emphasis on focused, quality care for those suffering with SCI.2,3 Much work has been done in recent years to understand and treat patients with SCI. The United States government has established model SCI care systems across the country to collect data, treat patients, and perform research; 25 such systems have been supported by federal funding since the inception of the National Spinal Cord Injury Database in 1973. Despite this emphasis, however, experts estimate that the database captures only 13% of patients with SCI. In addition, there have been no overall incidence studies of SCI in the United States since the 1970s.4 These facts point to the inadequacy of current epidemiologic data and to the desperate need for expansion of ongoing research in the area. Aside from the National Spinal Cord Injury Database, there is primarily one other large collection of data, located in Olmsted County, Minnesota, that provides historical clues to the trends of SCI epidemiology in the United States.5,6 Several other, smaller studies from various parts of the country as well as from developing countries have also been published and provide some insight into the worldwide epidemiology of SCI. The incidence of SCI is the frequency with which new SCIs occur over a specified period of time (usually 1 year) in a designated population. In developed countries, the annual incidence of SCI varies from 11.5 to 53.4 cases per million population.7,8 The National Spinal Cord Injury Statistical Center estimates the annual incidence of SCI in the United States to be 40 per million; this translates into approximately 11,000 cases per year.4 A recent Canadian study showed the annual age-adjusted incidence in a tertiary referral center to be 42.4 per million for those 15 to 64 years old, and 51.4 per million for those 65 and older.9 These numbers do not reflect patients who die at the scene of the accident or prior to arrival at the hospital. Data collected from Olmsted County, Minnesota, between 1975 and 1981 established an age- and sex-adjusted incidence of 71 injuries per million; death prior to an SCI-injured patient’s reaching the hospital was counted. The same study showed an incidence of 50 injuries per million for patients reaching the hospital alive.5,6 These data demonstrate the importance of including those patients who do not make it to the hospital alive, as the mortality of SCI prior to arrival at a hospital ranges from 48.3 to 79%.10 The rate of death after admission to a hospital ranges from 4.4 to 16.7%,11 significantly less than the on-site and prior-to-hospital-arrival mortalities. In the Olmsted County data, 11% of SCI patients died during the first hospitalization.10 As mentioned previously, the overall incidence of SCI in the United States has not been studied since the 1970s; therefore, we cannot establish any recent trends. Again, the Olmsted County data give us earlier time points to analyze. The average annual age- and sex-adjusted SCI incidence rates rose steadily from 22 per million in 1935–1944, to 67 per million in 1965–1974, to 71 per million in 1975–1981, whereas the age-adjusted mortality declined slightly from 36 per million in 1965–1974 to 32 per million in 1975–1981 (Fig. 1.1). The incidence of those reaching the hospital alive increased from 17 (1935–1944) to 50 (1975–1981).5,6 Data from New York provided an unadjusted incidence of SCI of 43 per million in 1982–1988.8 The prevalence of SCI is the percentage of a population that is directly affected by an SCI at one particular point in time. Various studies have given prevalence rates between 130 and 1124 per million.12–15 Part of the difficulty in ascertaining prevalence is the lack of standardization of the definition of a prevalent case; lifelong SCI patients are generally counted, but those with mild injuries who improve significantly may not be.8 The Olmsted County data provided a prevalence of 583 per million in 1980,5 which means that approximately 132,000 persons were living with SCI at that time. The National Spinal Cord Injury Statistical Center estimated the June 2006 United States prevalence to be 253,000 persons (Table 1.1).4 Table 1.1 United States Prevalence of Spinal Cord Injury (SCI)
 Historical Overview
Historical Overview
 Data Sources and Adequacy
Data Sources and Adequacy
 Incidence
Incidence
 Prevalence
Prevalence
| Year | Prevalence (Number of People) |
|---|---|
| 1980 | 132,000 |
| 2006 | 253,000 |
 Etiology
Etiology
The causes of SCI are variable. In some cases, traumatic injury directly transmits kinetic or shear energy to the substance of the spinal cord, causing damage to the sensitive tissues. Other causes of SCI come from gradual compression with vascular ischemia, such as seen with growing tumors and arthritis. Still other causes of SCI arise from systemic diseases such as multiple sclerosis, amyotrophic lateral sclerosis, infection, and thromboembolism.16
Industrial countries’ etiologies of injury are naturally different from more agrarian or impoverished countries. Even within a country, however, there is variability from region to region and between primarily rural versus more urban populations. Nevertheless, on a global scale, about one half of all SCI cases can be attributed to accidents involving motor vehicles, bicycles, or pedestrians.8
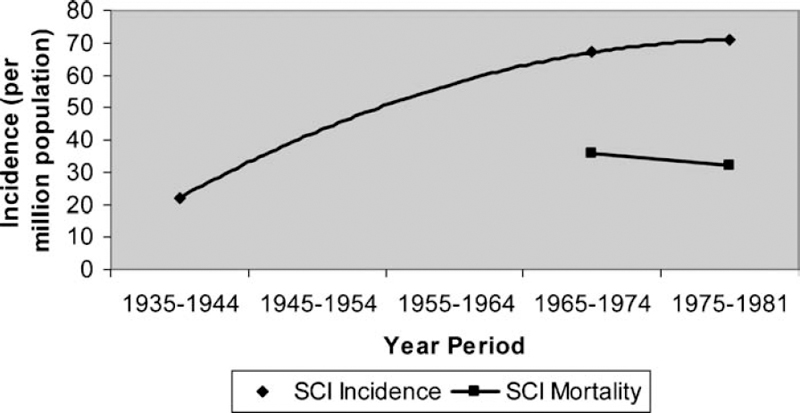
Fig. 1.1 Average annual age- and sex-adjusted spinal cord injury (SCI) incidence and mortality rates.
The etiology of a country’s SCI cases also changes with time.8 In some developing countries where communal violence is becoming increasingly rampant, the number of SCIs secondary to penetrating injuries of an inflicted nature is on the rise.17–19 On the other hand, in countries where there has been a focus on safe work practices, the number of SCIs taking place on the job is declining. Some countries’ sports- and recreational-activity-related injuries are on the rise.8
Table 1.2 Etiology of SCI since 2000
| Injury Cause | Incidence |
|---|---|
| Motor vehicle accidents | 46.9% |
| Falls | 23.7% |
| Violence | 13.7% |
| Sports | 8.7% |
| Other/unknown | 7.0% |
Recent data from the United States indicate that motor vehicle accidents account for 46.9% of reported SCIs since 2000 (Table 1.2). The proportion of injuries caused by falls has increased, whereas the proportion of those attributed to sports has diminished. Acts of violence as a proportion of etiology for SCI peaked from 1990 to 1999 at 24.8% and declined to only 13.7% since 2000 (Table 1.3).4
Substance Abuse and Alcohol Use: Do They Play a Role?
Overall, evidence for substance abuse, apart from alcohol use, is found in only a small percentage of SCI patients. On the other hand, alcohol use is implicated as a causative or contributing factor to the incident, causing the SCI in approximately 25% of patients.20
Associated, Preinjury Conditions
In patients with SCI, the most common abnormality of the spine seen prior to the SCI is cervical spondylosis, with a prevalence as high as 10% in some studies.8 Other acquired disorders such as rheumatoid arthritis, spinal arthropathy, and metastatic disease are also seen in patients with SCI. Congenital abnormalities like tethered cord, atlantoaxial instability, and congenital fusion may also be seen, and in some cases may exacerbate the injury.17
 Neurologic Level
Neurologic Level
The neurologic level of injury as defined by the American Spinal Injury Association (ASIA) is the most caudal segment of the spinal cord with normal function on both sides of the body.21 The need for precisely defining neurologic levels and the extent of incomplete SCIs led ASIA to publish Standards for Neurological Classification of Spinal Injured Patients22 for the first time in 1982; subsequent revisions have been made, producing further refinements in the definition of neurologic level, key muscle and sensory points, the Frankel scale (since modified to create the ASIA Impairment Scale), and the zone of partial preservation. The 1992 revision established sacral sparing as the basis for the definition of incomplete injuries and included recommendations for using an assessment of disability.23 The international community endorsed these standards,23 and they are now referred to as International Standards for Neurological Classification of Spinal Cord Injury.21 The ASIA standards continue to serve as an important clinical and research tool and can aid in determining the prognosis of SCI patients.24
Table 1.3 Violent Acts as an Etiology for SCI
| Year Period | Proportion of Total SCI Cases |
|---|---|
| 1990–1999 | 24.8% |
| 2000–2006 | 13.7% |
In general, the higher the neurologic level, the more devastating the injury. Therefore, the spine can be divided into three primary regions-cervical, thoracic, and lumbosacral-and two junctional zones-cervicothoracic and thoracolumbosacral.8 Each region carries its own subset of clinical manifestations. For example, high cervical injuries may result in respiratory failure, along with tetraplegia, neurogenic bladder, and other symptoms, whereas lumbar injuries can present as bladder and rectal abnormalities, with or without lower extremity weakness. The degree of devastation for a particular injury also depends on its severity and the patient’s clinical course, as a self-resolving cervical-level lesion would be less disabling than a permanent sacral-level injury.
The architecture of the cervical spine (C1 to C7-T1), including smaller vertebral bodies and greater relative mobility, makes it the most common location for SCI; indeed, cervical-level injuries account for approximately 55% of all injuries. The other regions of the spine, namely the thoracic (T1-T11), thoracolumbar (T11-T12 to L1-L2), and lumbosacral (L2-S5) levels, each account for approximately 15% of all SCI cases (Table 1.4).8
Table 1.4 Percentage of SCI by Level
| Neurologic Level | Percentage of SCI Cases |
|---|---|
| Cervical | 55 |
| Thoracic | 15 |
| Thoracolumbar | 15 |
| Lumbosacral | 15 |
Injuries encountered during a specific activity sometimes have a predilection for a certain region of the spine, corresponding to a particular neurologic level of injury. For example, diving injuries have a propensity for the cervical spine, whereas injuries encountered in mining, logging, and some recreational activities tend to involve the thoracolumbar spine. It is interesting to note that the high lethality associated with cervical spine trauma is reflected in the striking difference between the incidence (52%) and prevalence (40%) of cervical-level injuries.8
Table 1.5 Percentage of SCI Classified as Complete
| Year/Period | Proportion of Total SCI Cases Considered Complete |
|---|---|
| 1961 | 66% |
| 2000–2006 | 52.4% |
 Deficit Severity
Deficit Severity
Use of the terms complete and incomplete can be confusing, and, in fact, the definitions vary among individual physicians and specialist groups. In general, a complete injury is one in which there is no motor or sensory function below a specified level, whereas an incomplete injury describes abnormal, but present, function caudal to the area of discussion. The terms can give a sense of the severity of the injury, and have implications for recovery, but even the term complete injury should not be construed as meaning that improvement in neurologic function cannot occur. As discussed previously, the ASIA standards define the terms with a slightly different emphasis, in which a complete injury is any injury without sacral sparing.21
Since 2000, slightly more than half (52.4%) of all SCIs reported to the National Spinal Cord Injury Statistical Center have been complete.4 This contrasts with 1961, when two thirds of injuries were reported as complete (Table 1.5).20 The reasons for this are numerous (Table 1.6), including improved motor vehicle safety, increased awareness of the need for strict immobilization following injury, better initial care and retrieval systems, and implementation of the avoidance of hypotension and hypoxia. In addition, strategies for transporting patients and nursing care in general have improved greatly.25 Over time, incomplete tetraplegia has increased slightly as a percentage of cases, whereas both complete paraplegia and complete tetraplegia have shown a slight diminution.4
Table 1.6 Reasons for Reduction in Number of Complete SCI Cases
| Improved motor vehicle safety |
| Adherence to strict immobilization following injury |
| Better initial care |
| More sophisticated retrieval systems |
| Superior strategies for transporting patients |
| Advances in nursing care |
| Prevention/treatment of hypotension |
| Avoidance of hypoxia |
When the level of neurologic injury is correlated with the severity of the injury, thoracic injuries more commonly produce complete SCIs. The greatest neurologic recovery of complete injuries occurs in those with cervical-level injuries, followed by those with thoracic, and then those with lumbar injuries. For incomplete injuries, recovery is related to the severity of the neurologic deficit, regardless of level, with more severe initial injuries being associated with poorer neurologic recovery.25 Overall, less than 1% of SCI patients experience complete recovery by hospital discharge.4
 Vertebral Column Injuries
Vertebral Column Injuries
Bearing in mind the close proximity of the spinal cord and nerve roots to the bony elements of the spine, it is no wonder that SCI is often associated with some vertebral column abnormality. In fact, it is rather expected that there be radiographic evidence of injury or trauma. This is not always the case, as evidenced by the classification of some SCIs as spinal cord injury without obvious radiologic abnormality (SCIWORA) or spinal cord injury without obvious radiologic evidence of trauma (SCIWORET). The widespread availability of high-resolution computed tomography (CT) and magnetic resonance imaging (MRI) scanners has reduced the number of injuries that are classified in this manner, however. Underlying congenital abnormalities or spondylosis can often be identified when evidence of direct spinal cord trauma is lacking.26
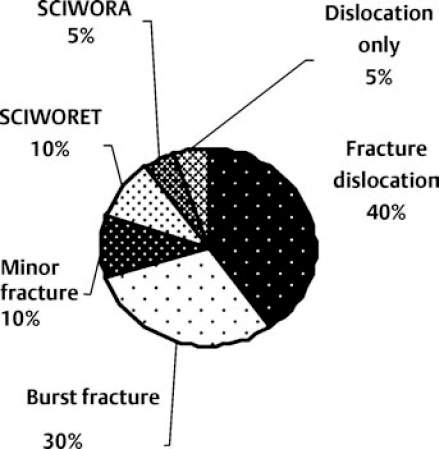
The incidence for each type of vertebral column injury in adults is illustrated in Fig. 1.2.27 Correlation of neurologic injury severity and vertebral column injury reveals that complete SCI is more likely to result from anterior dislocations and fracture dislocations compared with burst fractures and compression fractures.8 Different types of vertebral column injury may be associated with similar neurologic-level injuries.
 Systemic Injuries
Systemic Injuries
Spinal cord injury occurs as the sole injury to a patient in approximately 20% of cases.28–31 Other significant injuries occur 20 to 57% of the time.17 Motor vehicle collisions are responsible for many of these multisystem traumas.8 Traumatic brain injury patients have an associated SCI 5 to 10% of the time. Conversely, 25 to 50% of patients with acute SCI have a traumatic brain injury (Fig. 1.3).30
Some data suggest that the multiplicity of injuries in SCI patients reduces the potential for neurologic recovery and increases mortality.8 There are more than likely several reasons for this (Table 1.7). First, hypoxia and hypotension may be caused, or worsened, by other injuries. These two physiologic aberrations have been implicated in secondary injury to the spinal cord. Second, multiple injuries may be associated with a more severe initial SCI. Third, treatment of the other injuries in an SCI patient becomes more challenging. For example, neurogenic shock may make hypotension difficult to treat. Furthermore, cervical injuries, especially higher injuries, can make the establishment of an airway more complicated and are associated with respiratory failure. In addition, SCI can disguise intra-abdominal pathology when a clinical assessment is being made.32