CHAPTER 12
EMG and Nerve Conduction Studies
OVERVIEW
In the practice of pain medicine, nerve conduction studies and electromyography provide useful information through the diagnosis of peripheral neurologic injury. By precisely identifying and localizing spinal root and peripheral nerve injury, these studies provide an important role in confirming the anatomical site active in pain generation. This knowledge increases the success of focal procedural and other interventions. It should be noted that these tools should be used to optimize patient care or help guide surgical and interventional practice.
DEFINITIONS
Electromyography (EMG) and nerve conduction studies (NCS) are electrodiagnostic tests performed to evaluate the function of the peripheral nervous system. These tests are usually but not invariably performed together and interpreted in conjunction. Often the single term “EMG” is used to mean an examination comprising both NCS and EMG studies, though this is technically an imprecise usage. Both examinations evaluate and measure aspects of the electrophysiological properties inherent in peripheral nerve and muscle tissue. Through assessment of these neurophysiological parameters, these studies provide accurate diagnostic information to the clinician regarding the integrity and function of the spinal nerve roots, nerve plexi, peripheral nerves, neuromuscular junction, and muscle.
INDICATIONS
EMG/NCS are performed in patients for the following reasons:
• To evaluate if a symptom is due to injury within the peripheral nervous system (PNS)
• To localize the site of nerve injury within the PNS (ie, to spinal root, nerve plexus, peripheral nerve, neuromuscular junction, and/or muscle)
• To assess the nature of the injury, including severity, chronicity, and at times pathophysiology
Symptoms consistent with possible peripheral nerve injury, either in isolation or combination, include the following:
• Pain in limb
• Neck pain
• Back pain
• Numbness in feet
• Numbness or tingling of limbs
• Weakness of arms or legs
• Clumsiness in hands
• Gait impairment
CONTRAINDICATIONS
NCS and EMG are relatively safe tests, with few potential associated complications or side effects. Some patients find the study uncomfortable; however, when performed correctly, both NCS and needle EMG examination are well tolerated by most patients.
There are no absolute contraindications to NCS/EMG; however, the following relative contraindications are considered:
• Needle electromyography is performed with caution in patients on anticoagulation and/or on antiplatelet therapy.
![]() The examination is generally modified to exclude muscles at noncompressible sites to eliminate the risk of hematoma.
The examination is generally modified to exclude muscles at noncompressible sites to eliminate the risk of hematoma.
![]() Although not absolutely contraindicated, examination of the paraspinal musculature is generally avoided in patients on anticoagulation due to potential adverse effects of possible hematoma formation adjacent to spinal structures.
Although not absolutely contraindicated, examination of the paraspinal musculature is generally avoided in patients on anticoagulation due to potential adverse effects of possible hematoma formation adjacent to spinal structures.
• Needle electromyography is not performed in muscles where overlying skin infection or other tissue pathology is seen or suspected.
• Needle electromyography is avoided in affected limbs of patients with lymphedema.
• Nerve conduction studies requiring proximal stimulation at Erb point or the neck are not performed in patients with permanent pacemakers, internal defibrillators, or other implanted electrical devices.
RELEVANT ANATOMY
• Spinal nerve roots from C1-C4 form the cervical plexus, and supply sensory function to the back of the head and neck, and motor innervation to cervical musculature.
• Roots from C5-T1 supply neurologic function to the upper extremities. The nerve roots from these levels combine fibers and ramify in the anterior neck forming the brachial plexus, off of which branch the peripheral nerves supplying sensory and motor function to the shoulders, arms, and hands.
• Roots from the thoracic vertebrae innervate the dermatomes and myotomes of the anterior and posterior trunk.
• Roots from L1-S2 supply neurologic function to the lower extremities, via the lumbosacral plexus, from which arise the peripheral nerves subserving sensory and motor function of the legs and feet. (Figures 12-1 to 12-3).
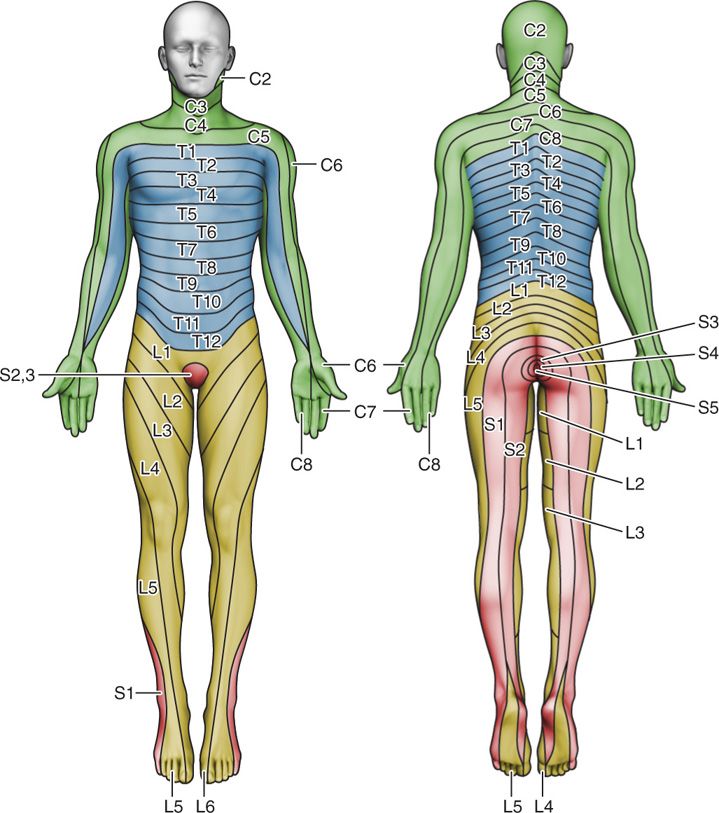
Figure 12-1. Dermatome map.
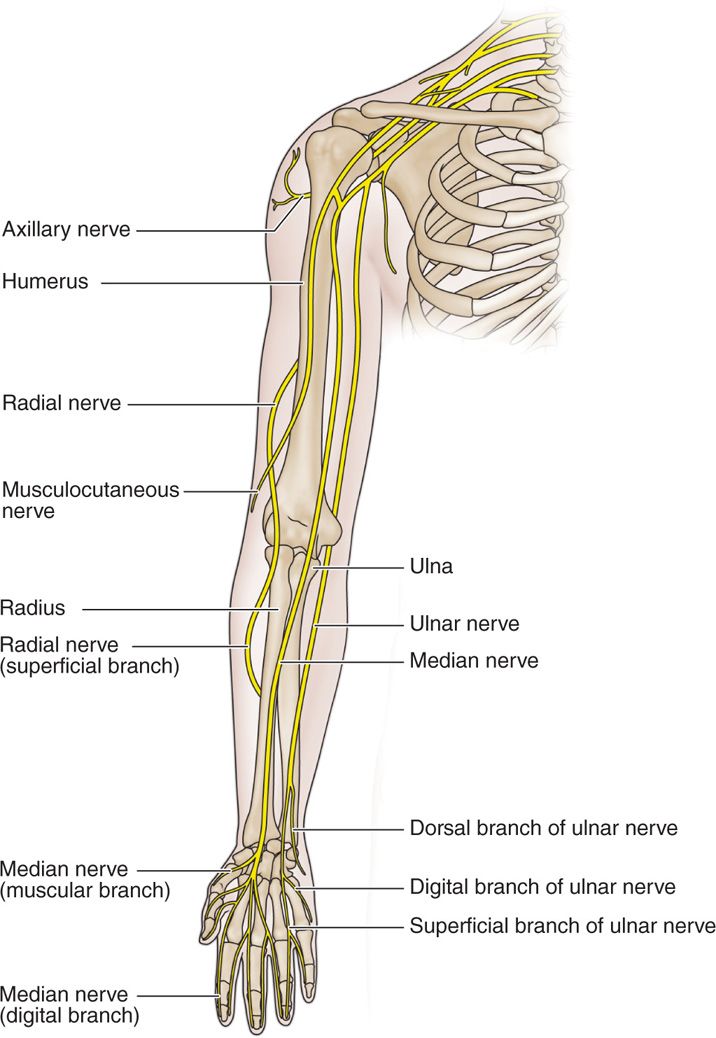
Figure 12-2. UE nerve schematic drawing.
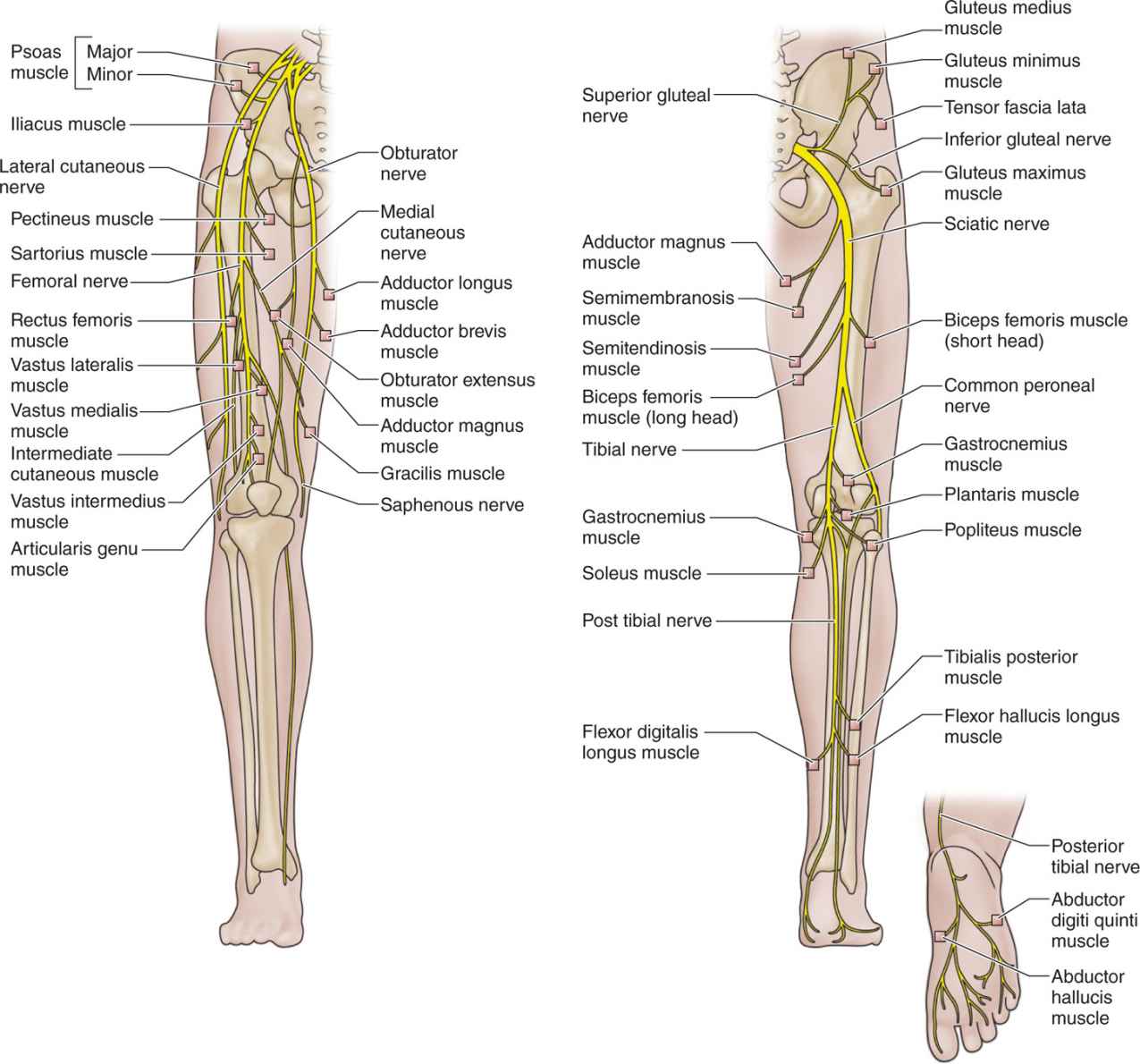
Figure 12-3. LE nerve schematic drawing.
TECHNICAL ASPECTS AND CONSIDERATIONS
NCS/EMGs are most frequently performed in the outpatient office setting. NCS may be performed by a trained technician or physician; however, the EMG portion is always performed by a physician. Both examinations are performed in “real time,” with findings elicited during the examination influencing the extent and specific subsequent course of the study. Study design and the interpretation of all information derived from these tests must be performed by a physician with training in electrodiagnostic medicine and a solid understanding of clinical neurophysiology (Figure 12-4).

Figure 12-4. EMG/NCS machine. A typical EMG/NCS system which has settings for both nerve conduction studies and electromyography.
NERVE CONDUCTION STUDIES
Nerve conduction studies (NCS) involve the delivery of an electrical stimulus externally over the skin along the course of a peripheral nerve. This stimulus activates the selected underlying nerve; that is, it depolarizes the nerve causing an action potential. The response evoked by stimulation of the nerve is then measured at a site distant to the stimulation by a recording electrode placed on the surface of the skin. Motor nerves, sensory nerves, and reflex pathways involving both can be studied in this method, with slight variations in technique (Figures 12-5 and 12-6).

Figure 12-5. NCS stimulator. The bipolar prongs are held against the skin overlying the nerve to provide an electrical potential that induces depolarization over the stimulated nerve segment.
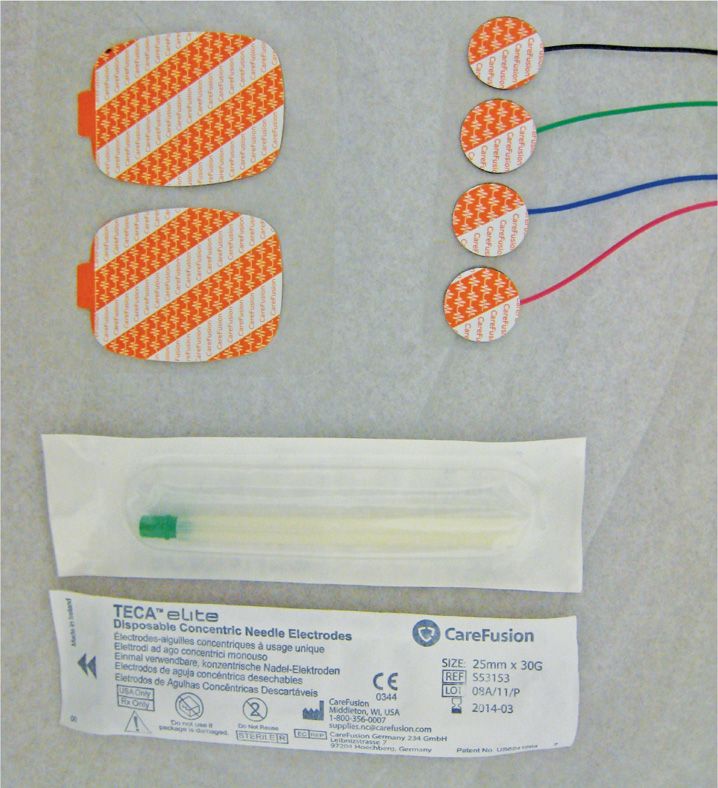
Figure 12-6. Surface and needle electrodes. Recording and ground electrodes for NCS, and single-use disposable needle electrodes for EMG.
Motor NCS are performed by stimulating over the selected nerve, and recording the compound muscle action potential (CMAP) with a surface electrode placed over a muscle that the selected nerve is known to innervate. Standard procedures have been established for the commonly (and less commonly) studied nerves that identify specific sites for stimulation and recording.
In general for all motor NCS:
• Stimulation is performed at least 2 sites, a distal site and a proximal site/sites.
• A single recording site is used to measure the responses from all stimulation sites.
For example, a recording electrode for the median nerve is placed over the abductor pollicis brevis (APB) muscle over the thenar eminence, and the nerve is first stimulated at the wrist (distal site) and then at the antecubital fossa (proximal site) (Figures 12-7 and 12-8).
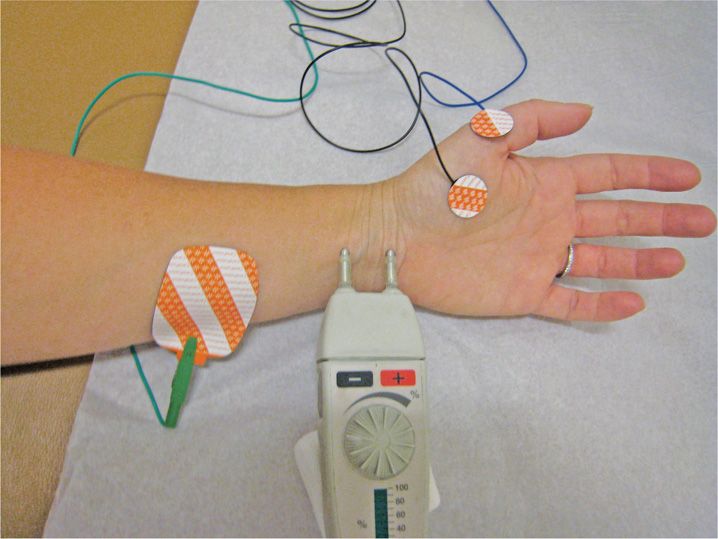
Figure 12-7. Median nerve conduction studies, distal stimulation. Recording electrodes are placed over the abductor pollicis brevis muscle, and the nerve is stimulated at the wrist (distal stimulation site).
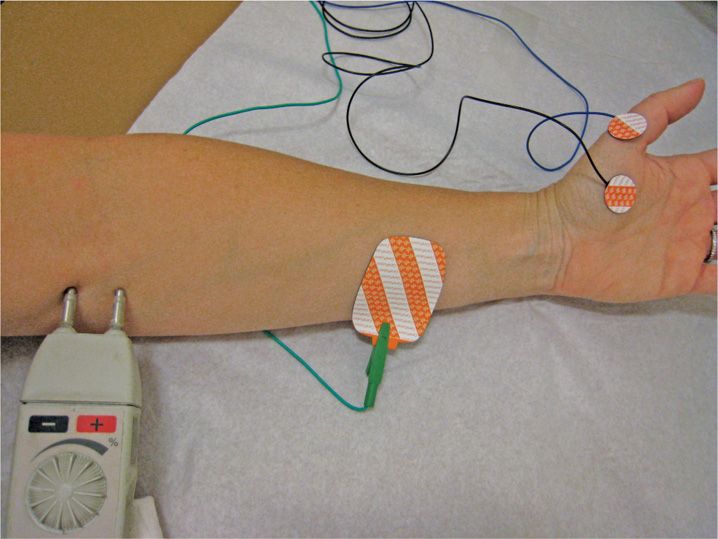
Figure 12-8. Median motor nerve conduction studies, proximal stimulation. Recording electrodes are placed over the abductor pollicis brevis muscle, and the nerve is stimulated at the antecubital fossa (proximal stimulation site).
For the peroneal nerve, a recording electrode is placed over the extensor digitorum brevis (EDB) muscle in the foot. The nerve is first stimulated at the ankle (distal site), then below the neck of the fibula, then again above the neck of the fibula (Figure 12-9).

Figure 12-9. Peroneal motor nerve conduction studies, distal stimulation. Recording electrodes are placed over the extensor digitorum brevis muscle, and the nerve is stimulated at the anterior ankle (distal stimulation site).
Several electrophysiological parameters are recorded, measured, and analyzed, including:
• Distal motor latency
• Compound muscle action potential (CMAP) amplitude
• Motor nerve conduction velocity
Results are then analyzed in comparison with normative data for the specific nerve and electrophysiological parameter studied (Figure 12-10 and Table 12-1).
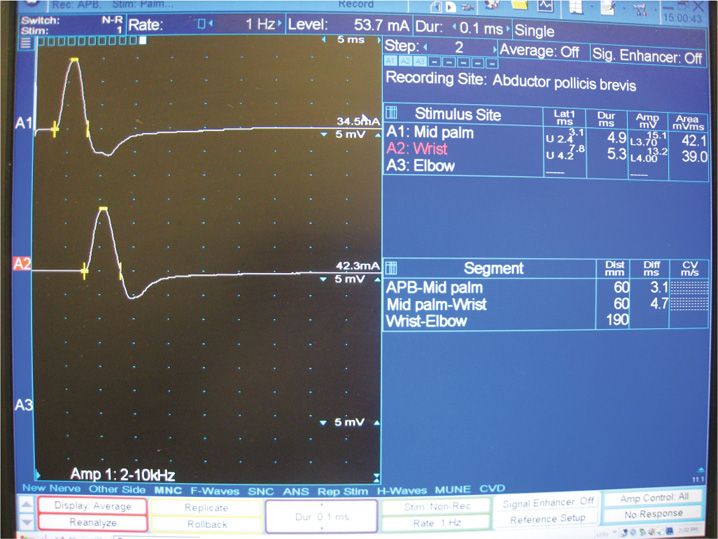
Figure 12-10. Median motor tracing. Motor nerve conduction study of the median nerve. The top line displays the compound muscle action potential (CMAP) obtained by distal stimulation, and the bottom line displays the CMAP obtained by proximal stimulation. Numerical data pertaining to the CMAP responses is displayed on the right of the screen.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






