INTRODUCTION AND EPIDEMIOLOGY
The thought of a woman presenting to the ED in active labor is justifiably a cause for anxiety—the emergency physician must contend not only with the often rusty recollection of the stages of normal delivery, but also with the knowledge that there are serious and even fatal complications associated with labor. Maternal and fetal survival may depend on the ability to successfully manage pre-eclampsia, eclampsia, hemorrhage, shoulder dystocia, malpresentation, cord prolapse, breech delivery, or fetal distress. Every ED should be prepared to take care of a woman in active labor. Tools include a basic delivery kit, an infant warmer or isolate, and medical supplies and equipment for neonatal resuscitation (see chapter 108, “Resuscitation of Neonates” and Tables 101-1 and 101-2).
Sterile gloves Sterile towels and drapes Povidone-iodine (Betadine) to cleanse the perineum Sterile lubricant gel Sterile scissors Kelly clamps Cord clamps Rubber suction bulb Towel or blanket for the infant Gauze sponges (4×4) Syringes (10 mL) and needles (22–24 gauge) Placenta basin Suture (3-0 chromic and 2-0 Vicryl) and needle driver |
| Classification | Medication | Dosage | Indication/Use | Contraindications |
|---|---|---|---|---|
| Uterotonic | Oxytocin | 10–40 units/1000 mL normal saline or 10 units IM | Stimulation of uterine contraction or as uterotonic for PPH | Hypersensitivity |
| Misoprostol | 1000 micrograms PR once | Unlabeled use for PPH | Hypersensitivity | |
| Methylergonovine | 0.2 milligram IM or IV or PO; may repeat at 2–4 h intervals | PPH | Hypersensitivity, hypertension | |
| Carboprost | 250 micrograms IM every 15–90 min (total dose 2 milligrams) | PPH | Asthma | |
| Antihypertensive | Hydralazine | 5 milligrams IV, followed by 5- to 10-milligram boluses every 20 min | Pre-eclampsia/eclampsia, hypertensive emergency | Hypersensitivity |
| Labetalol | 20 milligrams IV, followed by doubled doses up to 80 milligrams (20–40–80–80) every 10 min; maximum total dose, 220 milligrams | Pre-eclampsia/eclampsia, hypertensive emergency | Hypersensitivity, sinus bradycardia | |
| Anticonvulsant | Magnesium sulfate | Loading dose of 4–6 grams IV over 15 min, followed by 2 grams/h infusion; can also give 5 grams IM in each buttock | Seizure prophylaxis in pre-eclampsia/eclampsia | Myasthenia gravis |
| Electrolyte supplement toxicity | Calcium gluconate | 1 gram IV over 5–10 min | Magnesium toxicity | Hypersensitivity, cardiac arrhythmia |
| Analgesic | Lidocaine 1% | 1–10 mL injected locally | Local anesthetic | Hypersensitivity |
| Fentanyl, 50 micrograms/mL | 50 micrograms/mL | Short-acting opiate analgesic | Hypersensitivity | |
| Opiate antagonist | Naloxone | 0.4–2.0 milligrams IV every 2–3 min as need up to 10 milligrams cumulative dose | Narcotic overdose | Hypersensitivity |
| Antiemetic | Ondansetron | 4 milligrams IV | Nausea, vomiting | Hypersensitivity |
Out-of-hospital births occurred in 1.36% of births in 2012, and out-of-hospital births in the United States had a lower risk profile than in-hospital births, so that fewer teen, preterm, low-birth-weight, and multiple births occurred out of hospital.1 Occasionally, planned home deliveries experience medical complications and require rapid transport to the ED to assist with labor and delivery. In a prospective study of home births in the United States and Canada, nearly 12% of 5400 women who had planned a home delivery ultimately required urgent transfer to a hospital during the course of labor. The majority of intrapartum transfers were performed for failure to progress, need for pain management, and maternal exhaustion. Postpartum transfers encompassed a variety of obstetric and/or neonatal complications such as maternal hemorrhage, retained placenta, or newborn respiratory distress.2
Out-of-hospital deliveries may also occur due to inadequate or nonexistent prenatal care, transportation difficulties, remote setting, or the onset of premature labor. Occasionally, a woman may also attempt to avoid the hospital/physician fees associated with pregnancy until the delivery of her child, presenting to a hospital for the first time when in active labor.
The development of obstetric centers for high-risk pregnancy has led to a significant decline in neonatal mortality in the United States, and transports to specialized units have increased. The most common reasons for transport include preterm labor (41%), premature rupture of membranes (21%), hypertensive disease (16%), and antepartum hemorrhage (13%).3 Other indications for transport include eclampsia or pre-eclampsia, fetal distress, multiple gestation, fetal anomalies, and maternal health problems, including traumatic injuries. EMS units transporting an actively laboring patient should carry sterile delivery packs, relevant medical supplies (Table 101-1), and appropriate medications (Table 101-2). The transport team should be trained to assist in the precipitous delivery of an infant. Prehospital protocols regarding the complications of labor and delivery should be reviewed regularly to ensure that EMS personnel are adequately prepared for both normal delivery and potentially catastrophic pregnancy-related events.
For deliveries in an austere environment or in a disaster zone, the United Nations Population Fund provides a vaginal delivery kit for use during disaster relief, which includes a plastic sheet to lay on the ground, soap for washing hands and the perineum, string and a razor blade to tie and cut the umbilical cord, and a blanket to protect the newborn baby.4
PHYSIOLOGY
Determining rupture of membranes predicts not only the likelihood of imminent labor, but also the potential for complications, such as infection or cord prolapse. Spontaneous rupture of membranes occurs during the course of active labor in the majority of patients, although it also happens prior to onset of labor in approximately 8% of third-trimester patients.5 Fifty percent of women who experience premature rupture of membranes deliver within 5 hours, and 95% give birth within 28 hours of this event.6 The history of spontaneous rupture of membranes typically involves report of a gush of clear or blood-tinged fluid. Occasionally, patients recount continued leaking or dampening of their underwear on standing or with a Valsalva maneuver. Thick greenish brown fluid suggests the presence of meconium in amniotic fluid.
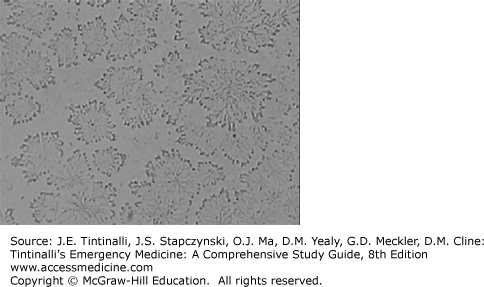
Rupture of membranes may be confirmed by using nitrazine paper to test residual fluid in the fornix or vaginal vault while performing a sterile speculum examination. Amniotic fluid has a pH of 7.0 to 7.4 and will turn nitrazine paper a dark blue. Vaginal fluid, on the other hand, typically has a pH of 4.5 to 5.5; the nitrazine strip, thus, remains yellow. False-positive results may occur, however, in the presence of blood, lubricant, Trichomonas vaginalis, semen, or even cervical mucus. Another test that confirms rupture of membranes is ferning, which is the observation of sodium chloride crystals on a microscope slide as amniotic fluid dries (Figure 101-1).
Rupture of the amnion and chorion prior to the onset of labor is called premature or prelabor rupture of membranes. If rupture of membranes occurs prior to 37 weeks of gestation, it is termed preterm premature rupture of membranes. Prolonged rupture of membranes transpires if delivery does not take place within 18 hours of rupture of membranes. It is important to understand the difference between and management of premature and preterm premature rupture of membrane as these patients may present to an ED for an initial evaluation.7 Risk factors related to both premature rupture of membranes and preterm premature rupture of membranes include infection, history of trauma, multiple gestation, fetal anomalies, abruptio placentae, and placenta previa. Obtain emergency obstetrics consultation for preterm premature rupture of membranes.
Cervical dilatation describes the diameter of the internal cervical os and indicates the progression of labor. The index and middle fingers of the examining hand are used to estimate the diameter, which is expressed in centimeters (from closed to 10 cm). Ten centimeters indicates full dilatation. As labor progresses, the cervix also undergoes thinning, known as effacement, which is described in terms of a percentage (%) of normal cervical length. Unfortunately, this estimate is poorly reproducible among examiners. Station indicates the level that the fetus occupies in the pelvis. The maternal ischial spines serve as the reference point and are palpable on either side of the vaginal canal (located at 4 and 8 o’clock). If the presenting fetal part remains above the ischial spines, the station is described as negative. Once the presenting fetal part has reached the level of the ischial spines, the station is 0, with further descent into the pelvis described as +1 or +2. Therefore, a +3 station corresponds to visible scalp at the introitus, indicating a fetal position consistent with impending delivery.
Distinguishing true from false labor is an important initial step in the management of the pregnant patient (Table 101-3). False labor is defined as uterine contractions that do not produce cervical changes and is characterized by irregular, brief contractions that are usually confined to the lower abdomen. Commonly known as Braxton Hicks contractions, they are irregular in both intensity and duration. False labor may persist for several days and is commonly treated with hydration and rest.
True labor, on the other hand, is characterized by painful, repetitive uterine contractions that increase steadily in both intensity and duration and result in cervical effacement and dilatation. Specifically, true labor pains typically commence in the fundal region and upper abdomen and radiate into the pelvis and lower back. True labor leads not only to cervical dilatation and effacement, but also to the progressive descent of the fetus into the pelvis, in preparation for delivery.
There are three stages of labor (Table 101-4). The first stage commences with the onset of regular uterine contractions and ends with full cervical dilatation. The first stage can be subdivided into two phases: latent and active. The latent phase is characterized by moderately uncomfortable uterine contractions that are infrequent and irregular, resulting in gradual cervical changes. In this preparatory phase the uterus orients to contractions and the cervix undergoes both effacement and softening. The active phase is typically noted to arise once the cervix has dilated to 3 to 4 cm, and results in cervical dilatation at an average rate of 1.2 cm/h in nulliparous and 1.5 cm/h in multiparous women. The second stage of labor commences at full dilatation and ends with the delivery of the infant.8 The mean length of the second stage of labor is 20 minutes for multiparous women and 54 minutes for nulliparous women.9 The third stage of labor starts after the delivery of the infant and ends with the delivery of the placenta. The third stage usually lasts less than 10 minutes, and active intervention is usually not required until after 30 minutes, unless hemorrhage occurs.
| Stage | Definition | Comments |
|---|---|---|
| First stage | From onset of regular uterine contractions to full cervical dilatation | — |
| Latent phase | Irregular, infrequent contractions | Preparatory phase, cervix softens and effaces |
| Active phase | Begins once cervix has dilated to 3–4 cm | Nulliparas: cervix dilates at 1.2 cm/h Multiparas: cervix dilates at 1.5 cm/h |
| Second stage | From full dilatation to delivery | Nulliparas: mean duration 54 min Multiparas: mean duration 20 min |
| Third stage | From delivery of infant to delivery of placenta | 10 min; intervention not needed until >30 min |
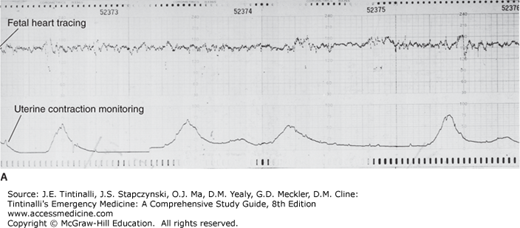
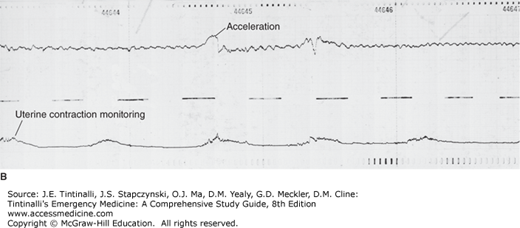
Fetal distress may occur during active labor. Thus, evaluate for signs of fetal status frequently. Indicators of fetal distress include fetal bradycardia or tachycardia, or late decelerations in fetal heart rate, which are defined as persistent drops in fetal heart rate both during and more than 30 seconds after a contraction. A physician or nurse trained in fetal monitoring can identify fetal distress (Figure 101-2). Doppler measurement of fetal heart tones is not reliable to detect decelerations. If decelerations are suspected, obtain emergency obstetrics consultation, and try to increase maternal blood flow by positioning the patient in the left lateral position, provide IV hydration, and administer oxygen. Further information is provided in the Advanced Life Support Course for Obstetrics (see later section “Useful Web Resources“).
FIGURE 101-2.
Fetal heart rate variability and uterine contraction patterns. A. Good variability. B. Good variability with brief accelerations. Fetal heart rises above baseline and quickly returns to normal. A reassuring pattern. C. Poor variability. May be due to fetal hypoxia. D. Variable decelerations. No relationship to uterine contractions. May represent cord compression. E. Late deceleration. Occurs at onset of contraction and slow return to baseline after contraction ends. Signifies uteroplacental insufficiency and fetal hypoxia. [Reproduced with permission from Pearlman MD, Tintinalli JE, Dyne PL (eds): Obstetric and Gynecologic Emergencies: Diagnosis and Management. McGraw-Hill, Inc., 2003. Figs. 10-9 and 10-10, pp. 131 and 132.]
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree