
Elbow Injuries
Andrew D. Perron and Carl A. Germann
The elbow is a complex synovial hinge joint consisting of three articulations between the distal humerus, radius, and ulna. Because of the need for a wide variety of articular motions (flexion–extension and pronation–supination), the joint is at risk for instability with injury. The humerus widens distally to form the lateral and medial condyles. The capitellum is a spheroidal cartilaginous structure of the lateral condyle that articulates with the radial head, permitting pronation and supination. The trochlea is a spoon-shaped cartilaginous projection of the medial condyle that articulates with the deep trochlear notch of the ulna, permitting flexion and extension at the elbow. The articulating surfaces of the head of the radius and ulna are held together by the annular ligament. The associated musculature and the anterior capsule combined with the radial and ulnar collateral ligaments provide stability at the elbow joint.
A number of important structures traverse or are located within the elbow. The wrist flexor and pronator muscle groups originate from the medial epicondyle. The wrist extensor and supinator muscles attach to the lateral epicondyle. The brachial artery traverses the elbow and is palpable medial to the biceps tendon in the antecubital space. The median nerve traverses deep in the antecubital fossa medial to the brachial artery. The ulnar nerve courses posteriorly in the cubital tunnel between the medial epicondyle and olecranon process. The radial nerve passes between the heads of the triceps in the posterior humerus and is at risk for injury in humeral shaft fractures.
There are several bursal structures in and around the elbow that help facilitate the wide range of motion possible in the joint. The superficial olecranon bursa lies beneath the skin over the olecranon process and is particularly vulnerable to traumatic and infectious processes. Figure 39.1 illustrates the anatomy of the elbow.
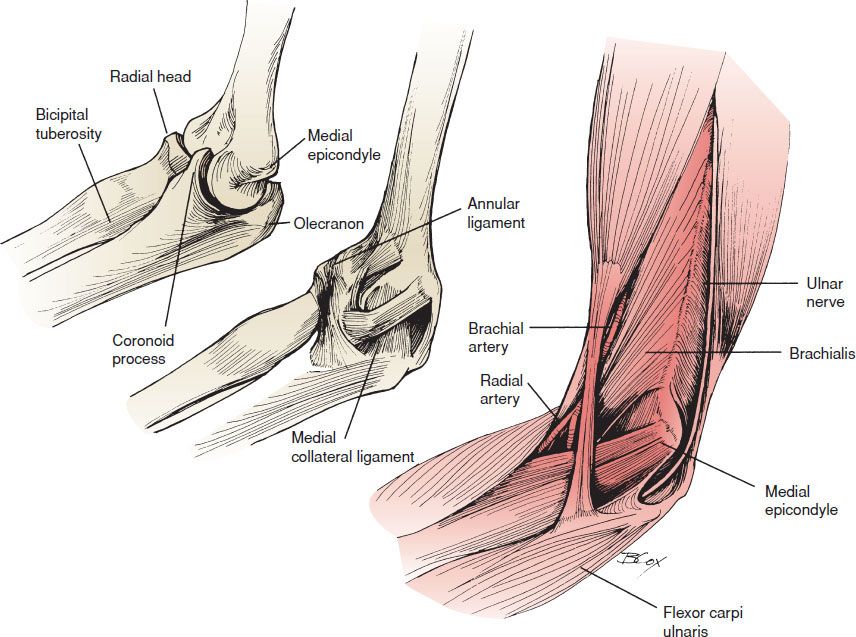
FIGURE 39.1 Elbow anatomy. (From McCue FC III, Sweeney T, Urch S. The elbow, wrist, and hand. In: Perrin DH, ed. The Injured Athlete. 3rd ed. Philadelphia, PA: Lippincott-Raven; 1999, with permission.)
ED EVALUATION
The emergency department (ED) assessment of elbow injuries should include a focused history of the mechanism of injury. The most common complaints are pain, restriction of movement, and swelling. A description of the location and duration of pain, aggravating factors, and presence of paresthesias or loss of movement is important. Elbow pain may also be referred from injuries to the shoulder, forearm, or wrist. Conversely, injuries to the elbow may refer pain to the wrist. Identification of one injury should not preclude the search for other injuries. An occupational history may provide a clue to the diagnosis in patients presenting with chronic pain.
Inspection of the involved extremity for swelling, open wounds, deformities, effusions, and discoloration is the first step in the physical examination of the patient with elbow pain. In most cases, the involved joint should not be extensively manipulated until radiographs have been obtained to exclude fracture and dislocation. The shoulder, forearm, wrist, and hand should also be carefully examined to look for associated injuries. Laceration over the medial epicondyle should raise suspicion of an ulnar nerve injury, whereas laceration over the antecubital fossa should raise suspicion for injury to the brachial artery or median nerve. Any abnormality noted in the involved extremity should be compared with the contralateral extremity.
An effusion is best palpated over the soft tissue area lateral to the radial head. The bony prominences of the medial and lateral condyles, olecranon, and radial head should be palpated for tenderness. The radial head is best palpated with the thumb of one hand while pronating and supinating the forearm with the examiner’s other hand. Limitation of motion, crepitance, or pain should all be noted. With the elbow flexed to 90 degrees, the medial and lateral condyles and the olecranon should form a triangle. In an elbow dislocation, this triangle is disrupted with displacement of the olecranon. A posterior dislocation or extension-type fracture is suggested by a prominent olecranon. Loss of the olecranon prominence suggests an anterior dislocation or supracondylar fracture. The triangular relationship is maintained in supracondylar fracture. Each of the muscle groups should be tested against resistance and the muscle belly palpated during contraction.
Careful neurovascular examination of the structures distal to the elbow is of critical importance. Brachial, radial, and ulnar pulses should be palpated and capillary refill assessed. The brachioradialis, biceps, and triceps reflexes should be elicited. The radial nerve is best tested by evaluating wrist and finger extension. Wrist drop results from radial nerve injury. Flexion of the wrist and digits and pronation of the forearm are the functions of the median nerve. Inability to flex and abduct the thumb is diagnostic of median nerve injury. Loss of strength of the interossei muscles and adduction of the thumb suggests ulnar nerve injury. The sensory component of the radial nerve innervates the dorsum of the hand and is best tested in the web space between the thumb and index finger. Median nerve sensation is tested over the palmar aspect of the thumb and the digits to the radial one-half of the ring finger; at the volar tip of the index finger, there is no overlap from the radial or median nerves. The ulnar nerve is tested at the volar tip of the small finger. The neurovascular examination of the extremity should be repeated after manipulation and at regular intervals as edema from a fracture may result in neurovascular compromise.
The radiographic examination of the elbow should consist of a minimum of two views at right angles to each other (anteroposterior [AP] and true lateral). Radiographs are most commonly misread because a true lateral view of the elbow is not obtained. In one university ED setting, the incidence of missed elbow fractures was 12% (1). Oblique views may be obtained to provide additional information. Specialized views, such as the radial head–capitellum view, are indicated when a suspicion for particular injury exists.
On the lateral radiograph, a line parallel to the anterior border of the humerus should intersect the anterior portion of the middle third of the capitellum (Fig. 39.2) (2). If this intersection is displaced, usually anterior to the capitellum, a supracondylar fracture should be suspected.

FIGURE 39.2 Anterior humeral line. The anterior humeral line is drawn on the lateral radiograph along the anterior surface of the humerus through the elbow. Normally this line transects the middle of the capitellum (left). With an extension fracture of the supracondylar region, this line will either transect the anterior third of the capitellum or pass entirely anterior to it (right). (Adapted from Simon RR, Koenigsknecht SJ. Emergency Orthopaedics: The Extremities. 2nd ed. Norwalk, CT: Appleton & Lange; 1987, with permission.)
The radiocapitellar line extends from the center of the radius and should intersect the middle third of the capitellum on the lateral view (2). Disruption of this line suggests radial head dislocation or fracture and is most useful in evaluating subtle fractures in children.
Fat pad signs are helpful in diagnosing occult fractures within the joint capsule. The anterior fat pad consists of fat in the coronoid and radial fossa. This radiolucent fat overlaps and normally appears as a triangular area anteriorly over the distal humerus on a lateral radiograph of the elbow. The posterior fat pad is located in the olecranon fossa and is normally hidden by the overlying humeral condyles on a lateral radiograph.
When an effusion is present, it distends the joint capsule and displaces the fat pads (Fig. 39.3). The anterior fat pad displaces anteriorly and superiorly and appears bowed out as a “ship’s sail.” The posterior fat pad becomes visible on radiography with elbow injury and is highly indicative of intra-articular disease. In the setting of elbow trauma, a visible posterior fat pad or a prominent anterior fat pad in the absence of visible fracture should prompt consideration of occult fracture, most commonly of the radial head.

FIGURE 39.3 Anterior and posterior fat pad signs are indicated by the large white arrows. Small black arrows indicate the radial head fracture that produced the effusion displacing the fat pads.
Positive fat pad signs can also be present with any intra-articular disease process and thus are not strictly pathognomonic for fracture. Fat pad signs may be seen with arthritis, gout, pseudogout, infection, neoplasia, or other disease process causing an intra-articular fluid collection (3). A fat pad sign may not be present with severe injury causing disruption of the joint capsule.
Though usually not necessary in the ED evaluation of these patients, computed tomography (CT) scanning may be useful in delineating complex fractures in adults. Magnetic resonance imaging (MRI) has become the procedure of choice for evaluating soft tissues, cartilaginous surfaces, joint space, and trabecular bone (4).
KEY TESTING
Plain radiographs for skeletal injuries must:
• Include the appropriate bone/joint injured
• Have at least two views at right angles to each other
• Be adequate for diagnosing most elbow fracture and dislocation injuries
CT Imaging:
• Particularly useful to better characterize elbow injury and assist in preoperative planning
• Consider when the relationship of fracture fragments is complex or will impact downstream care (e.g., multifragment radial head fractures, fracture/dislocation injuries)
• Can be combined with angiographic contrast (CT-A) to identify injuries to major blood vessels)
MR Imaging:
• Provides greatest soft tissue detail (tendons, ligaments, disc)
• Can also provide imaging in multiple planes (axial, coronal)
• Consider when there is a potential soft tissue injury that will impact care (e.g., degree of tendon injury)
Ultrasound:
• An imaging modality being used by some practitioners in the bedside diagnosis of musculoskeletal injuries
• Trained hands can identify fractures, dislocations, and some soft tissue injuries (e.g., tendon tears)
ED MANAGEMENT
Supracondylar Fractures
Supracondylar fractures occur in the distal humerus proximal to the epicondyles and are most commonly seen in children. In adults, because of their stronger bones, elbow dislocations from ligamentous disruption are more common. These fractures most commonly result from a fall on the outstretched hand with the elbow in extension.
Twenty-five percent of supracondylar fractures are nondisplaced. Treatment of a nondisplaced fracture is a posterior splint from axilla to palm, with the elbow flexed to 90 degrees. These patients should be urgently referred to an orthopedic surgeon for follow-up within 24 to 48 hours. The patient and parents should be carefully counseled regarding warning signs of compartment syndrome. A child with elbow tenderness and swelling should be splinted, even without a demonstrable radiographic fracture, because of the possibility of occult fracture (5).
In displaced fractures, the distal fragment is usually displaced posteriorly (extension injury), and an abnormal anterior humeral line will be visualized on the lateral radiograph. Anterior displacement of the distal fragment (flexion injury) occurs less frequently and is caused by a direct blow to the posterior aspect of the flexed elbow.
Assessment of neurovascular function is essential, especially with extension injuries, because occult injury to the brachial artery may occur. A strong pulse does not completely rule out arterial injury, and a vascular study should be performed if injury is clinically suspected. The reported rate of nerve injury in displaced supracondylar fractures is up to 20% (6). Injury to the median and radial nerve can occur from stretching or entrapment on the proximal humeral fragment. The ulnar nerve may also be disrupted and is more frequently damaged in a flexion-type fracture (6). Closed reduction of displaced fractures should be attempted as soon as possible if neurovascular compromise is present.
Displaced fractures require internal fixation or percutaneous pinning if good alignment is not maintained with closed reduction. Patients with displaced fractures should be admitted because of the risk of delayed swelling and neurovascular compromise, including compartment syndrome, and the potential for Volkmann ischemic contracture. Flexion fractures may also require internal fixation and should be splinted in extension.
A common complication of supracondylar fracture is an abnormal carrying angle. The normal carrying angle is 10 to 15 degrees of valgus. Measurement of Baumann’s angle, formed by a line perpendicular to the humeral shaft and a line through the lateral humeral condyle, is predictive of an acceptable carrying angle (7). This angle normally measures about 75 degrees. A discrepancy of >5 to 10 degrees, compared with the uninjured extremity, is an unacceptable reduction, as it may impair useful function of the arm (Fig. 39.4).
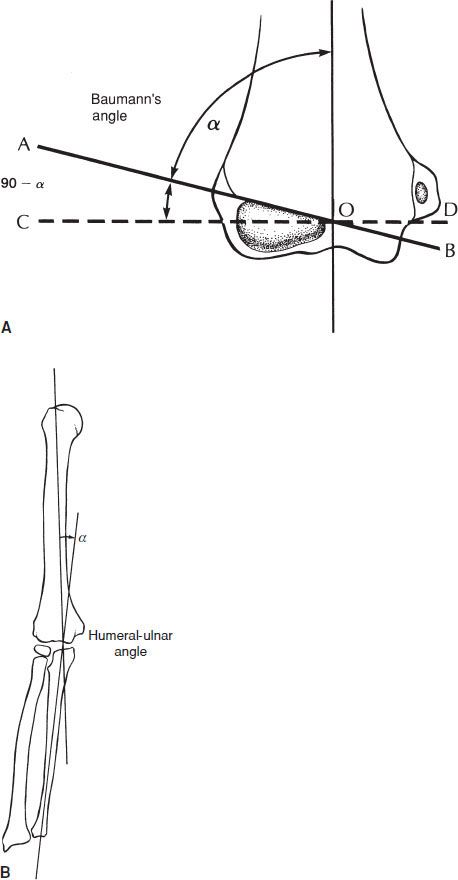
FIGURE 39.4 A: Baumann’s angle. B: Humeral–ulnar angle. (From O’Brien WR, Eilert RE, Chang FM, et al. The metaphyseal-diaphyseal angle as a guide to treating supracondylar fractures of the humerus in children. Unpublished data, with permission.)
Intercondylar Fractures
Intercondylar fractures usually occur in older patients as a result of direct trauma to the flexed elbow. They usually occur in “T” and “Y” configurations, and treatment is based on the amount of displacement of the humeral condyles from each other and from the proximal humerus. Neurovascular complications are uncommon, and these fractures rarely require manipulation by the emergency physician.
Nondisplaced fractures are treated in a posterior splint for 3 weeks, and then active range of motion is begun. Displaced fractures are treated with internal fixation and early range of motion beginning after 1 week. Severely comminuted fractures may be treated with olecranon traction for 3 to 4 weeks if operative repair is not possible.
Humeral Condyle Fractures
Isolated humeral condyle fractures are caused by a fall on the outstretched hand, by direct trauma, or by avulsion of bone from the pull of the flexor or extensor muscles from the medial and lateral condyles, respectively. Lateral condyle fractures are more common than medial condyle fractures and frequently involve the joint surface.
Nondisplaced lateral condyle fractures are immobilized in a posterior splint, with the elbow flexed to 90 degrees and the forearm in supination with the wrist extended. The forearm should be in pronation and the wrist flexed for medial condyle fractures. Active range of motion is begun as early as 2 to 3 weeks after injury. Operative fixation is required for displaced fractures, owing to instability caused by the pull of the forearm muscles. All of these patients should be treated in consultation with an orthopedic surgeon.
Epicondyle Fractures
Epicondyle fractures in adults are usually caused by a direct blow. The medial epicondyle is involved more commonly than the lateral epicondyle, and ulnar nerve function should be evaluated, as it is in close proximity to the medial epicondyle at the elbow (Fig. 39.5). There is up to a 50% incidence of associated elbow dislocation with medial epicondyle fracture (8).

FIGURE 39.5 Avulsion fracture of the medial epicondyle. (From Yochum TR, Rowe LJ. Yochum and Rowe’s Essentials of Skeletal Radiology. 3rd ed. Philadephia, PA: Lippincott Williams & Wilkins; 2004.)









