![]() Clinical suspicion of acute anterior, posterior, lateral, medial, or divergent dislocation with or without neurovascular compromise
Clinical suspicion of acute anterior, posterior, lateral, medial, or divergent dislocation with or without neurovascular compromise
![]() The clinical presentation depends on the type of dislocation
The clinical presentation depends on the type of dislocation
![]() Suspected dislocation is clinically confirmed by disruption of the relationship between the tip of the olecranon and the distal epicondyles of the humerus in comparison with the unaffected elbow
Suspected dislocation is clinically confirmed by disruption of the relationship between the tip of the olecranon and the distal epicondyles of the humerus in comparison with the unaffected elbow
![]() Radiographic evidence of anterior, posterior, lateral, medial, or divergent dislocation (FIGURE 65.1)
Radiographic evidence of anterior, posterior, lateral, medial, or divergent dislocation (FIGURE 65.1)
CONTRAINDICATIONS
![]() Open dislocations require emergent consultations with an orthopedic surgeon
Open dislocations require emergent consultations with an orthopedic surgeon
![]() Multiple failed reduction attempts with adequate sedation should prompt consultation with an orthopedic surgeon
Multiple failed reduction attempts with adequate sedation should prompt consultation with an orthopedic surgeon
![]() Irreducible elbow dislocations may require operative management
Irreducible elbow dislocations may require operative management
![]() An elbow that has been unreduced for 7 or more days will likely require open reduction with an orthopedic surgeon
An elbow that has been unreduced for 7 or more days will likely require open reduction with an orthopedic surgeon
RISKS/CONSENT ISSUES
![]() Procedural sedation may be associated with loss of airway reflexes and respiratory arrest (these risks are extremely rare)
Procedural sedation may be associated with loss of airway reflexes and respiratory arrest (these risks are extremely rare)
![]() Soft-tissue injury may occur with reduction attempts
Soft-tissue injury may occur with reduction attempts
![]() Fractures and neurovascular injury may occur with reduction attempts
Fractures and neurovascular injury may occur with reduction attempts
![]() General Basic Steps
General Basic Steps
![]() Obtain necessary x-rays
Obtain necessary x-rays
![]() Sedation/Analgesia
Sedation/Analgesia
![]() Position patient
Position patient
![]() Reduction
Reduction
![]() Postprocedure exam/x-rays
Postprocedure exam/x-rays

FIGURE 65.1 Posterior dislocation of the olecranon. (From Campbell C. Elbow dislocation. In: Greenberg MI, ed. Greenberg’s Text-Atlas of Emergency Medicine. Philadelphia, PA: Lippincott Williams & Wilkins; 2005:492, with permission.)
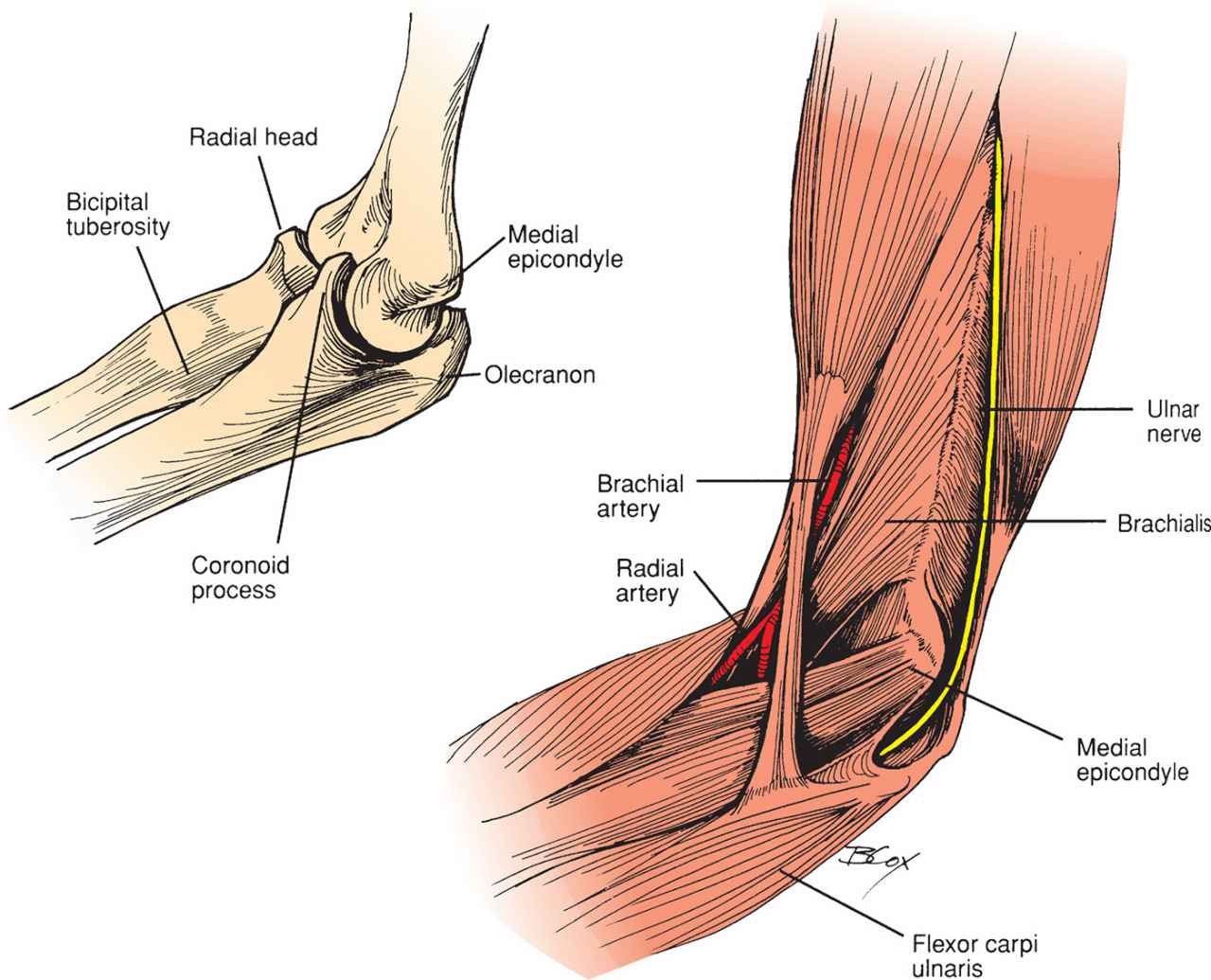
FIGURE 65.2 Elbow anatomy. (From McCue FC III, Sweeney T, Urch S. The elbow, wrist, and hand. In: Perrin DH, ed. The Injured Athlete. 3rd ed. Philadelphia, PA: Lippincott Williams & Wilkins; 1999, with permission.)
TECHNIQUE
![]() Perform a complete neurovascular check before any reduction attempt
Perform a complete neurovascular check before any reduction attempt
![]() Obtain radiographs of the affected joint and consider radiographs of one joint above and below the injury (shoulder and wrist)
Obtain radiographs of the affected joint and consider radiographs of one joint above and below the injury (shoulder and wrist)
![]() Complex dislocations (those with associated fractures) may require consultation with orthopedic surgery
Complex dislocations (those with associated fractures) may require consultation with orthopedic surgery
![]() Dislocations with neurovascular compromise should be reduced without prior imaging
Dislocations with neurovascular compromise should be reduced without prior imaging
![]() Anesthesia/analgesia: Consider parenteral analgesics. Reduction may also be attempted with injection of local anesthetic alone into the elbow joint or an ultrasound-guided brachial plexus block
Anesthesia/analgesia: Consider parenteral analgesics. Reduction may also be attempted with injection of local anesthetic alone into the elbow joint or an ultrasound-guided brachial plexus block
![]() Reduction technique is determined by the type of dislocation
Reduction technique is determined by the type of dislocation
TECHNIQUE: POSTERIOR DISLOCATION
![]() 80% to 90% of all elbow dislocations
80% to 90% of all elbow dislocations
![]() Mechanism of injury: Most commonly caused by a fall on an outstretched hand with the arm in extension
Mechanism of injury: Most commonly caused by a fall on an outstretched hand with the arm in extension
![]() Clinical presentation: Shortened forearm that is held in flexion with a prominent olecranon posteriorly. In addition, a defect may be palpable above the olecranon (FIGURE 65.2).
Clinical presentation: Shortened forearm that is held in flexion with a prominent olecranon posteriorly. In addition, a defect may be palpable above the olecranon (FIGURE 65.2).
![]() Associated injuries:
Associated injuries:
![]() Fractures including radial head and coronoid process are common
Fractures including radial head and coronoid process are common
![]() Small fractures of the coronoid process may be treated as simple posterior dislocations
Small fractures of the coronoid process may be treated as simple posterior dislocations
![]() Neurologic symptoms accompany 15% to 22% of dislocations
Neurologic symptoms accompany 15% to 22% of dislocations
![]() Ulnar nerve injury is most common followed by median nerve injury
Ulnar nerve injury is most common followed by median nerve injury
![]() Radial nerve injury commonly occurs when the dislocation is complicated by radial head fracture
Radial nerve injury commonly occurs when the dislocation is complicated by radial head fracture
![]() Traction leading to stretch injury, local swelling, and entrapment during reduction are common causes of nerve injury
Traction leading to stretch injury, local swelling, and entrapment during reduction are common causes of nerve injury
![]() Brachial artery injury occurs in 5% to 13% of posterior dislocations
Brachial artery injury occurs in 5% to 13% of posterior dislocations
![]() Reduction Techniques
Reduction Techniques
![]() Supine Technique
Supine Technique
![]() Place patient in supine position
Place patient in supine position
![]() An assistant stabilizes the humerus by wrapping both hands around arm just distal to axilla
An assistant stabilizes the humerus by wrapping both hands around arm just distal to axilla
![]() The physician grasps the wrist with one hand and places the other hand just above the antecubital fossa with the thumb on the olecranon (FIGURE 65.3)
The physician grasps the wrist with one hand and places the other hand just above the antecubital fossa with the thumb on the olecranon (FIGURE 65.3)
![]() The physician applies slow, steady in-line traction while the assistant applies steady countertraction
The physician applies slow, steady in-line traction while the assistant applies steady countertraction
![]() To minimize additional trauma to the coronoid process, the elbow is held in slight flexion and the wrist is held in supination as traction is applied
To minimize additional trauma to the coronoid process, the elbow is held in slight flexion and the wrist is held in supination as traction is applied
![]() Avoid hyperextension as this may cause injury to the median nerve or brachial artery
Avoid hyperextension as this may cause injury to the median nerve or brachial artery
![]() Reduction is accompanied by a “clunk” that is heard or felt
Reduction is accompanied by a “clunk” that is heard or felt
![]() Alternatively, the forearm may be gently flexed in an effort to reduce the joint
Alternatively, the forearm may be gently flexed in an effort to reduce the joint
![]() Seated Technique
Seated Technique
![]() Patient is seated in a high backed chair with arm hanging over the back of the chair in a flexed position
Patient is seated in a high backed chair with arm hanging over the back of the chair in a flexed position
![]() The physician applies traction by gently pulling down on the patient’s hand while guiding the olecranon into place using the other hand
The physician applies traction by gently pulling down on the patient’s hand while guiding the olecranon into place using the other hand
![]() The physician may also elect to simply apply downward pressure onto the olecranon to reduce the elbow
The physician may also elect to simply apply downward pressure onto the olecranon to reduce the elbow
![]() Reduction is once again signaled by a “clunk”
Reduction is once again signaled by a “clunk”
![]() This method has the advantage of requiring only a single physician
This method has the advantage of requiring only a single physician
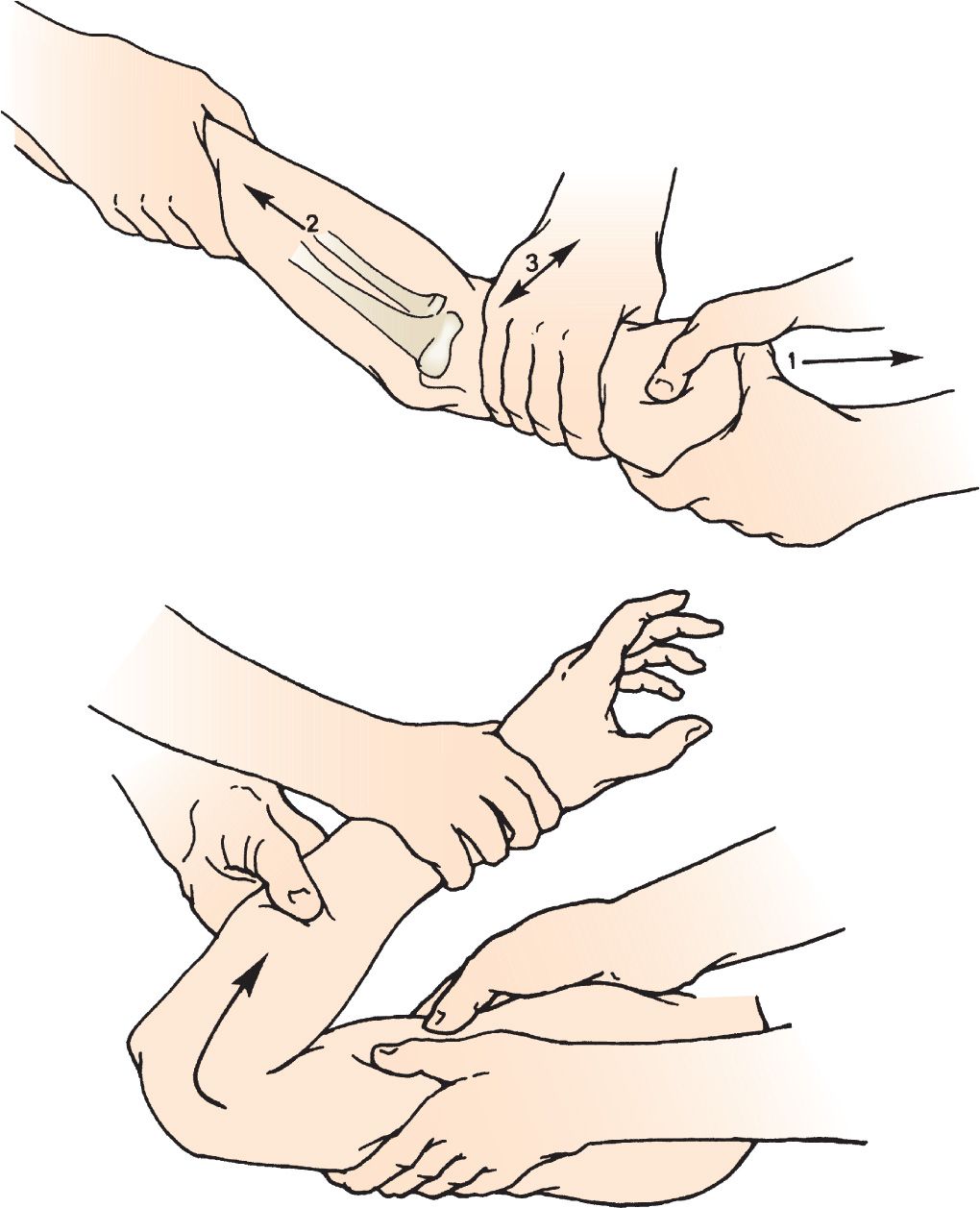
FIGURE 65.3 Technique for reduction of posterior dislocation of the elbow. (From Perron AD, Germann CA. Elbow injuries. In: Wolfson AB. Harwood-Nuss’ Clinical Practice of Emergency Medicine. 6th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2015:260, with permission.)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


