ANATOMY
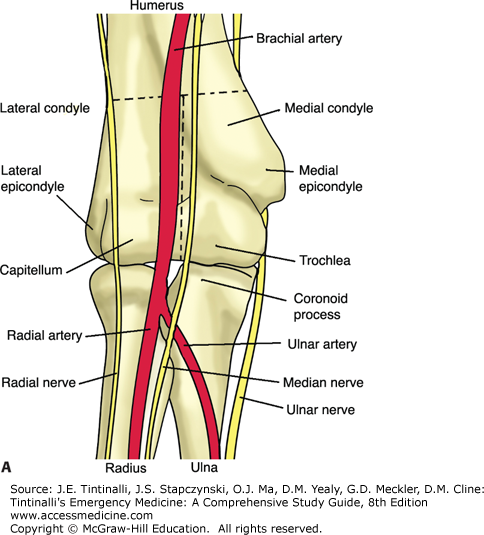
Articulations of the distal humerus and proximal ulna and radius form the elbow joint (Figure 270-1).
The epicondyles are nonarticulating surfaces that serve as sites of origin for forearm, wrist, and digit flexors and pronators (medial), and extensors and supinators (lateral). Medially, the trochlea articulates with the olecranon to form a uniaxial hinge joint. Laterally, the capitellum abuts the radial head to form a pivot joint. Between the condyles, the coronoid fossa is anterior, and the olecranon fossa is posterior. These allow for full flexion and extension of the ulna. The radial fossa lies proximal to the capitellum anteriorly and permits full flexion of the radius.
The radius and ulna are joined together along their entire length by a fibrous interosseous membrane, and articulate only at their ends to form the complex proximal and distal radioulnar joints. The ulna is a comparatively straight bone, whereas the radius has an important outward bowing. During the motions of supination and pronation, the radius rotates around the relatively fixed ulna. Because these bones have such a close relationship to one another, injury to one will have a direct impact on the other. A displaced or angulated fracture of one bone typically disrupts the other or causes a dislocation at the proximal or distal radioulnar joint.
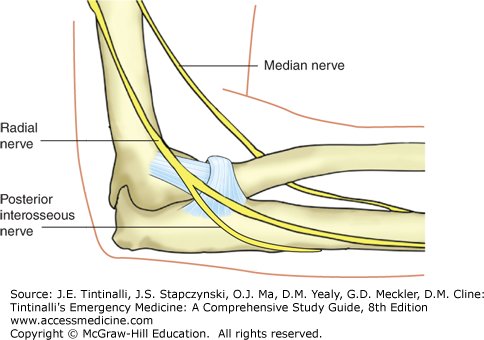
Several important neurovascular structures lie in close proximity to the distal humerus, and evaluation of their function is essential. These include the brachial artery, palpable just medial to the distal biceps tendon in the antecubital fossa, and the radial, median, and ulnar nerves (Table 270-1).
| Radial | Median | Ulnar | |
|---|---|---|---|
| Test for sensory function | Dorsum of the thumb index web space | Two-point discrimination over the tip of the index finger | Two-point discrimination over the little finger |
| Test for motor function | Extend both wrist and fingers against resistance | “OK” sign with thumb and index finger; abduction of the thumb (recurrent branch) | Abduct index finger against resistance |
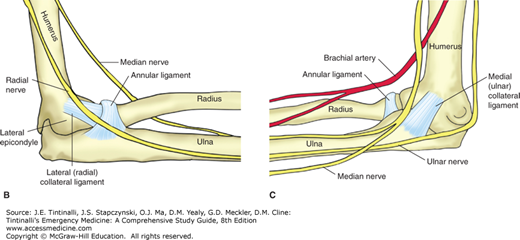
The neuroanatomy is best understood by appreciating the neural control of basic wrist and finger movement (Figure 270-2). The radial nerve travels over the lateral epicondyle and supplies the muscles of wrist extension before it branches off into the posterior interosseous nerve. This deep branch travels around the proximal radius and through the supinator muscle and controls the muscles of finger and thumb extension. The remainder of the radial nerve lies adjacent to the radial artery. This superficial branch is purely sensory and innervates the dorsal aspect of the hand from the thumb to the radial half of the ring finger. Thus, the proximal portion of the radial nerve controls the more proximal function of wrist extension, the deep branch (posterior interosseous nerve) controls the more distal function of finger extension, and the superficial branch is purely sensory. Therefore, an isolated injury to the posterior interosseous branch affects finger extension but spares wrist extension and sensation to the dorsum of the hand.
The median nerve supplies the muscles of wrist and finger flexion and sensation over the volar surface of the hand from the thumb to the radial half of the ring finger, including the dorsal tips of the thumb and index and middle fingers. The proximal portion of the median nerve innervates the muscles that control wrist flexion and the flexor digitorum superficialis before it gives off the anterior interosseous nerve. This branch controls portions of the remaining deep finger flexors. The remaining portion of the median nerve provides sensation to most of the volar surface of the hand in addition to controlling the thenar muscles of the thumb via a separate motor branch (recurrent branch of the median nerve).
The ulnar nerve provides innervation to forearm muscles and controls the intrinsic muscles of the hand while providing sensation to the little finger and the ulnar half of the ring finger. Proximal to the elbow, the ulnar nerve courses under a ligamentous band called the arcade of Struthers prior to entering the cubital tunnel posterior to the medial epicondyle. These are two sites where the nerve can become entrapped, leading to ulnar neuropathy syndromes. The ulnar nerve is palpable as a cord in the cubital tunnel and is vulnerable to injury with trauma over this area.
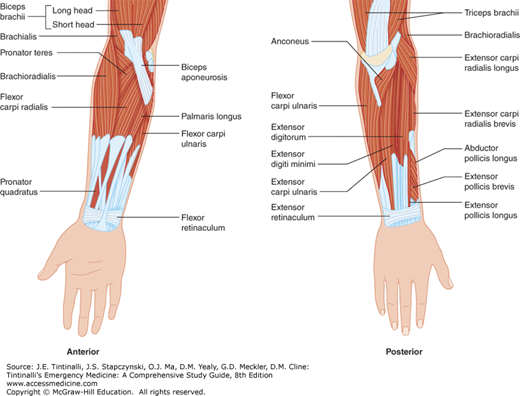
The biceps muscle has two proximal heads (Figure 270-3). The long head originates at both the supraglenoid tubercle of the scapula and the superior labrum of the glenohumeral joint, and then travels through the capsule of the shoulder and along the intertubercular (bicipital) groove of the humerus. The short head originates at the coracoid process of the scapula. The distal attachments are to the radial tuberosity by the distal biceps tendon and the forearm by the bicipital aponeurosis. A bicipitoradial bursa lies adjacent to the radial tuberosity. The biceps muscle is innervated by the musculocutaneous nerve (C5 and C6) and functions to flex the supinated forearm and supinate the flexed forearm.
The brachialis muscle lies deep to the biceps muscle. It originates on the distal anterior humerus and inserts on the ulnar tuberosity of the proximal ulna. The brachialis muscle is innervated by both the musculocutaneous and radial nerves (C5, C6, C7, and C8) and is the primary flexor of the forearm.
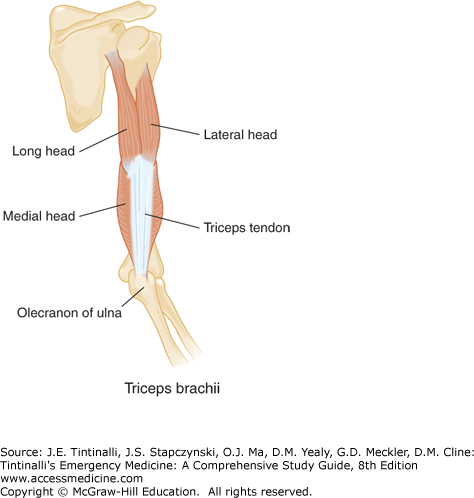
The triceps muscle has three proximal heads (Figure 270-4): a long head originating from the infraglenoid tubercle of the scapula; a lateral head on the posterior surface of the humerus superior to the radial (spiral) groove; and a medial head inferior to the radial groove. The triceps inserts at the olecranon. A subtendinous bursa separates the triceps from the olecranon, and a subcutaneous bursa lies just distal to the tendinous insertion. The latter frequently becomes inflamed. The triceps muscle is innervated by the radial nerve (C6, C7, and C8) and is the sole extensor of the forearm. Additionally, the triceps aids extension and adduction of the arm, and the long head stabilizes the head of the humerus in abduction.
The intrinsic forearm muscles include the brachioradialis, pronator teres, pronator quadratus, anconeus, and supinator (Figure 270-5). The brachioradialis muscle originates at the lateral condyle and assists with forearm flexion. The pronator teres muscle has two proximal heads that originate from the medial epicondyle and the proximal ulna; it pronates and flexes the forearm. The pronator quadratus muscle originates from the distal ulna and is the primary pronator of the forearm. The anconeus muscle originates from the posterior lateral epicondyle and has trivial function in extending the forearm. Lastly, the supinator muscle originates from the posterior medial ulna and supinates the forearm with the biceps muscle. The deep branch of the radial nerve (posterior interosseous nerve) pierces the supinator muscle after branching off of the proximal segment of the radial nerve. Thus, a compression neuropathy to the posterior interosseous nerve can occur at this level (Figure 270-6).
CLINICAL FEATURES
A thorough history is essential for determining the correct diagnosis in a patient with elbow or forearm pain. Onset of symptoms, mechanism of injury, exact location of pain, and associated symptoms such as numbness, weakness, or distal wrist and hand complaints are important elements to obtain. Most acute traumatic injuries to the elbow and forearm occur due to a fall onto an outstretched hand or a direct blow. Chronic overuse injuries should correlate with preceding activity involving a repetitive motion. A history of arthritides may point to a systemic disorder such as lupus, rheumatoid arthritis, or gout.
General examination of the elbow and forearm should include inspection for gross deformity, soft tissue swelling such as bursitis, or open wounds. Assess range of motion of the elbow in flexion, extension, pronation, and supination. Inability to fully extend the elbow is correlated with the presence of a fracture.1 Strength testing against resistance should also include wrist flexion and extension. Carefully assess radial, median, and ulnar nerve function. The single best test of radial nerve motor function is to have the patient extend both the wrist and fingers against resistance (Table 270-1). Test sensation with two-point discrimination over the dorsum of the thumb index web space. Evaluate the median nerve by assessing its distal branches. A simple test of anterior interosseous nerve function is the ability to make a circle, or “OK” sign, with the thumb and index finger. Abduction of the thumb against resistance (recurrent branch of the median nerve) and sensory testing over the tip of the index finger complete the evaluation of the median nerve. The easiest way to test ulnar nerve function is to have the patient spread the fingers apart against resistance. Sensation is tested over the tip of the fifth digit.
DIAGNOSIS
Initial imaging studies should include anteroposterior and lateral views of the elbow, and anteroposterior, lateral, and oblique views of the humerus and forearm. If a distal forearm injury is present, anteroposterior, lateral, and oblique views of the wrist instead of the humerus should be obtained. Attempts to derive a clinical decision rule to guide imaging decisions for the elbow, similar to published ankle and knee imaging rules, have so far produced conflicting data.1,2,3
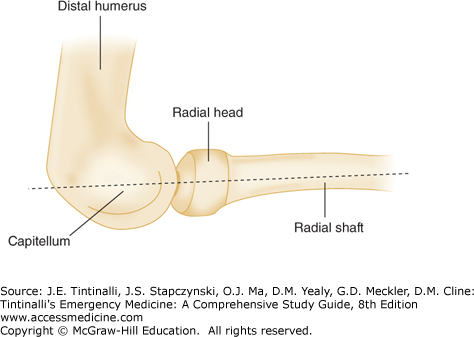
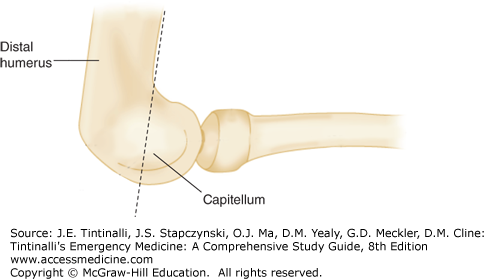
On lateral films of the elbow, a line drawn straight through the center of the radial shaft should bisect the radial head and capitellum (radiocapitellar line) (Figure 270-7). Loss of this relationship should raise suspicion for an occult radius fracture or dislocation. A line drawn straight along the anterior border of the humerus should transect the posterior two thirds of the capitellum (anterior humeral line) (Figure 270-8). Abnormal extension of the line through the anterior one third of the capitellum suggests a distal humerus (in adults) or supracondylar fracture (in children). A small anterior fat pad may be a normal finding. Large anterior and any posterior fat pads are always abnormal and indicate the presence of a joint effusion (Figure 270-9).
CT imaging provides greater radiographic detail when evaluating certain elbow fractures, particularly coronoid and comminuted intra-articular fractures. MRI is useful in the evaluation of soft tissue injuries such as ligament or tendon ruptures but has limited value in the acute setting. Bedside US can demonstrate effusions and tendon injury but requires operator skill.4,5
TREATMENT
Consult an orthopedic surgeon immediately for open fractures, irreducible dislocations, injuries resulting in a grossly unsTable elbow joint, or vascular injury with signs of ischemia or uncontrolled hemorrhage. All other injuries may be referred for follow-up within 1 to 2 days for operative planning or up to a week for nonoperative treatment. Table 270-2 outlines guidelines for ED immobilization and appropriate orthopedic consult time frames for the conditions discussed in this chapter.
| Injury | Splint | Referral |
|---|---|---|
Soft tissue injuries Biceps tendon rupture Triceps tendon rupture Lateral/medial epicondylitis | Sling immobilization Sling immobilization Forearm counterforce brace | 1 wk 1 wk 2–4 wk PRN |
Elbow dislocation Stable/postreduction Unstable/postreduction Irreducible | Long arm posterior splint, forearm in pronation Long arm posterior splint (presurgical stabilization) Long arm posterior splint (presurgical stabilization) | 1 d Immediate Immediate |
Elbow fractures Distal humerus nondisplaced Supracondylar Intercondylar Lateral condyle/epicondyle Nondisplaced Displaced Medial condyle/epicondyle Nondisplaced Displaced Articular surface Coronoid Nondisplaced or minimally displaced Markedly displaced or unstable Olecranon Radial head Nondisplaced Displaced or range of motion block | Long arm posterior splint, forearm neutral Long arm posterior splint (presurgical stabilization) Long arm posterior splint, forearm neutral Long arm posterior splint, forearm in supination, wrist extended Long arm posterior splint (presurgical stabilization) Long arm posterior splint, forearm in pronation, wrist flexed Long arm posterior splint (presurgical stabilization) Long arm posterior splint, forearm neutral Long arm posterior splint, elbow past 90 degrees, forearm in supination Long arm posterior splint (presurgical stabilization) Long arm posterior splint, forearm neutral Sling immobilization with early range of motion Long arm posterior splint, forearm neutral | 1 wk Immediate 1–2 d 1–2 d Immediate 1-2 d Immediate 1–2 d 1–2 d Immediate <24 h 1 wk <24 h |
Forearm fractures Both bones Pediatric Greenstick Displaced Adult Nondisplaced Displaced Isolated ulna shaft Proximal two thirds of radius Monteggia’s Galeazzi’s | Long arm posterior splint Long arm posterior splint (prereduction stabilization) Anteroposterior long arm splint Long arm posterior splint (presurgical stabilization) Long arm posterior splint, forearm neutral or sugar tong splint if stable and nondisplaced Long arm posterior splint, forearm neutral Long arm posterior splint (presurgical stabilization) Long arm posterior splint (presurgical stabilization) | 1 wk Immediate 1 wk <24 h 1 wk 1 wk Immediate Immediate |
SOFT TISSUE INJURIES
Of all injuries to the biceps, the vast majority are proximal, and nearly all involve the proximal long head. Injuries are usually the result of repetitive microtrauma and overuse. Steroids, whether injected locally or used systemically, can accelerate the breakdown of tendons. Biceps tendon rupture usually occurs when there is sudden or prolonged contraction against resistance in middle-aged and older individuals with a history of chronic bicipital tenosynovitis. A snap or pop is usually described, and pain is present in the anterior shoulder. Examination of the anterior shoulder will reveal swelling, tenderness, and often crepitus over the bicipital groove. Ecchymosis may extend the entire length of the biceps. Flexion of the elbow will elicit pain and may produce a midarm “ball,” which represents the distally retracted biceps muscle. Comparing arms for symmetry helps. Loss of strength is minimal due to the function of the brachialis and supinator. Avulsion fractures occasionally occur, so radiographs of the shoulder should be obtained.
ED treatment includes sling, ice, analgesics, and referral to an orthopedic surgeon for definitive care. Surgical repair is usually recommended for young, active patients. A conservative approach with immobilization may be adequate for elderly patients whose activities of daily living are not significantly compromised by the injury.
Distal biceps injuries are less common than proximal injuries.6,7 Complete ruptures of the tendon are most common in middle-aged men and usually involve the dominant extremity. Partial tears are seen in men and women. Mechanism of injury is typically a sudden eccentric (extension) load applied to a flexed elbow. In ruptures of the distal biceps, pain is felt in the antecubital fossa, with swelling, ecchymosis, and tenderness to palpation noted on examination. A distal rupture is indicated by a palpable defect in the antecubital fossa and a midarm “ball.” Strength loss, especially supination, is usually greater than with proximal ruptures. The biceps squeeze test, similar to the Thompson test for assessing Achilles tendon rupture, can detect biceps rupture.8 With the patient seated and the forearm at 60 to 80 degrees of flexion, place one hand on the muscle belly of the biceps brachii and the other hand on the myotendinous junction, and squeeze with both hands. The squeeze should result in forearm supination, indicating an intact biceps. Lack of supination is considered a positive test, indicating rupture of the distal biceps brachii. To perform the hook test,9 flex the patient’s elbow to 90 degrees, and during active supination, if the biceps tendon is intact, the examiner can “hook” the index finger under the distal biceps tendon in the antecubital fossa. Obtain elbow radiographs to search for an associated avulsion fracture. Although most complete distal ruptures are diagnosed clinically, MRI and US can aid in confirming the diagnosis of partial tears.10,11
ED treatment includes sling, ice, analgesics, and referral to an orthopedic surgeon for definitive care. Without surgical repair of complete ruptures, supination strength is decreased by approximately 50% and flexion strength by almost 30%.12,13
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree