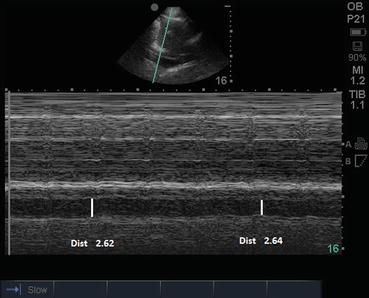
Fig. 57.1 TTE image
A 70-year-old male presents to the ED after an industrial accident causing a traumatic below-knee amputation on the right side. The patient has been obtunded and dyspneic since arrival. A total of six pRBC units and 5 L of crystalloids have been given in the last hour. You have been asked to evaluate this patient prior to operative BKA. HR, 120; BP, 90/60; RR, 35; SpO2, 84%.
Questions
- 1.
What is the view shown in the picture and how do you obtain it (See Fig. 57.1)?
- 2.
Is it accurate to measure fluid status and fluid responsiveness with TTE?
- 3.
How do you interpret the following images?
- 4.
Would you change this patient’s management, based on the ultrasound findings, and how?
- 5.
How would you confirm your suspicion?
Fig. 57.1A Probe placement
Answers
- 1.
This is a longitudinal view of the subcostal inferior vena cava.
In the supine position, if possible with the knees bent, (relaxes abdominal wall) the probe is placed in the midline 2 or 3 cm below the xyphoid perpendicular to the abdominal wall with the orientation marker pointing toward the 3 o’clock position (See Fig. 57.1A). Focusing on the right atrium the probe is turned counterclockwise until the orientation marker is pointing toward the patient’s head or until the IVC is seen merging into the RA. The IVC diameter is best-measured 2–3 cm before the IVC-RA junction, where the IVC walls are parallel [1].
- 2.
IVC diameter and dynamic measurements of the IVC diameter have been used as surrogates for CVP, fluid status, and responsiveness to fluid therapy. Several difficulties may be encountered when using this technique. It maybe difficult to obtain the appropriate image; the liver or diaphragm may tend to splint open the IVC in the most proximal portions. Tricuspid valve dysfunction, right heart structural abnormalities, and variation in the diameter of the IVC among normal patients may also confound the matter [2].
As recommended by the American society of echocardiography, in the context of focused cardiac ultrasound, IVC diameter and plethora are useful as surrogates of fluid status, when formal transthoracic echocardiography is not practical or readily available [3].
The IVC diameter and respiratory variation should be used along with other indicators of volume status for clinical correlation. The interpretation of this image alone should not be used for clinical decision-making.
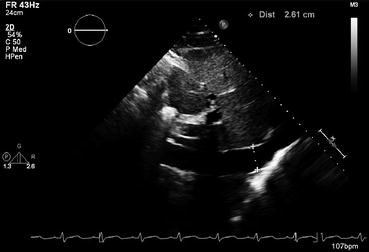
Fig. 57.2
Subcostal TTE longitudinal view of the subcostal inferior vena cava