Fig.
56.1
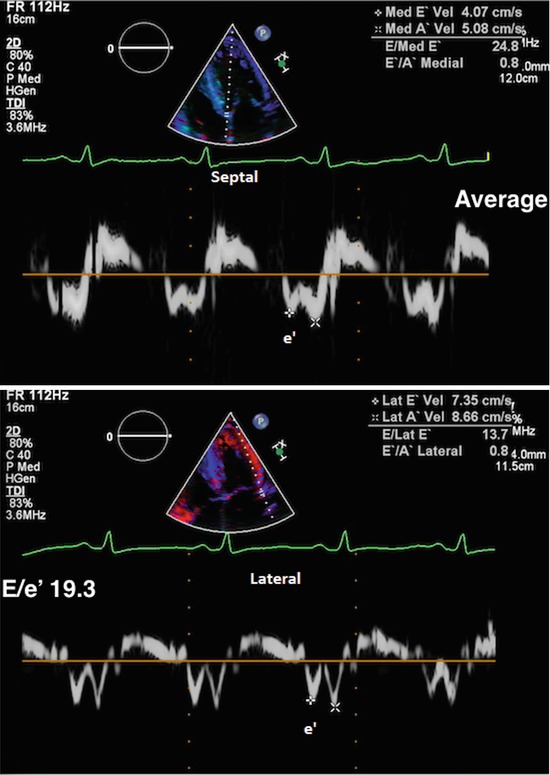
Fig.
56.2
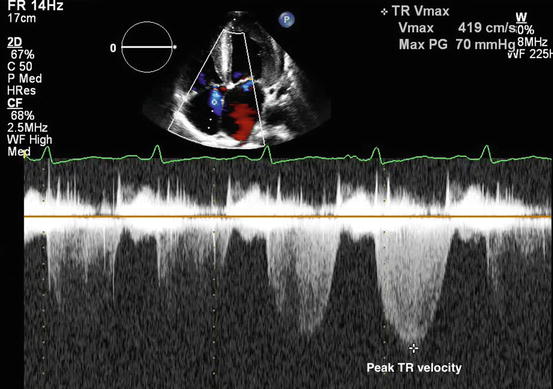
Fig.
56.3

Fig.
56.4
I. A 48-year-old male with history of uncontrolled hypertension and end-stage renal disease on hemodialysis presents for TTE as part of preoperative risk stratification prior to possible renal transplant. He has NYHA Class III symptoms at baseline. 2D images show moderately to markedly increased left ventricular wall thickness. LVEF calculated by the biplane Simpson’s method is 56%. The remainder of his diastolic parameters are as shown in Figs. 56.1, 56.2, 56.3, and 56.4.
Questions
- 1.
Describe what happens in normal diastole.
- 2.
What are the causes of diastolic dysfunction? What is the difference between diastolic dysfunction and heart failure with preserved ejection fraction (HF-pEF)?
- 3.
How do you use echocardiography to grade diastolic dysfunction?
- 4.
- 5.
Does this patient have normal or abnormal diastolic function? How would you grade it?
- 6.
What are the key considerations for managing diastolic dysfunction in the preoperative period?
Answers
- 1.
Diastole is defined as the portion of the cardiac cycle between aortic valve closure and mitral valve closure. It is normally divided into four phases: isovolumic relaxation, rapid early diastolic filling, diastasis, and atrial contraction. Isovolumic relaxation occurs between aortic valve closure and mitral valve opening. Through an active, calcium-dependent process, left ventricular pressure decreases, while volume remains the same [1]. When left ventricular end-diastolic pressure falls below left atrial pressure, the mitral valve opens and rapid early diastolic filling begins. This usually accounts for 70% of left ventricular filling [1, 2]. As pressures equalize between the left atrium and left ventricle, a small amount of filling continues via passive flow from the pulmonary veins; this is diastasis. Diastasis generally accounts for 5% of left ventricular filling and is only present at slower heart rates. If the patient is in sinus rhythm, atrial systole follows diastasis. Left atrial pressure again transiently increases, and there is further filling of the left ventricle. Atrial contraction generally accounts from 25% of left ventricular filling in the normal heart. Diastolic function is influenced by volume status, properties of the left ventricle (stiffness, recoil), atrial properties, and catecholamines.
- 2.
Aging, hypertension, diabetes, obesity, coronary artery disease, renal disease, valvular heart disease, and infiltrative processes all affect left ventricular mechanics/stiffening and thus diastolic function. In the presence of systolic dysfunction, diastolic function is always abnormal. HF-pEF is defined as the presence of diastolic dysfunction accompanied by signs/symptoms of clinical heart failure in patients with an ejection fraction of at least 50% [3].
- 3.
In the 2016 American Society of Echocardiography/European Association of Cardiovascular Imaging guidelines, there are four main echocardiographic parameters used to assess diastolic dysfunction: mitral inflow pulse wave (PW) Doppler, annular tissue Doppler imaging (TDI), peak tricuspid regurgitant (TR) velocity, and left atrial end-systolic volume index (LAESVi).
Mitral inflow PW Doppler is measured in the apical four chamber (A4C) view with the Doppler cursor placed at the mitral leaflet tips [2, 4]. The initial wave of early diastolic filling is labeled the E wave. The second wave represents filling due to atrial contraction and is labeled the A wave (Fig. 56.1). In normal hearts the E/A ratio is typically between 0.9 and 1.5 [2]. As relaxation becomes impaired, but before left atrial pressures (LAP) rise, there is an increased reliance on atrial contraction to maintain diastolic filling, and the E/A ratio is <0.9 [2]. As LAP continues to rise, there is again more filling happening in early diastole due to the increased pressure gradient between the left atrium (LA) and left ventricle (LV), and the E/A ratio becomes “pseudo normal.” As left ventricular compliance decreases and LAP rises further, there is initial brief filling in early diastole with relatively little filling happening during atrial contraction, and the E/A ratio increases to ≥2. Mitral inflow PW Doppler varies with volume status, mitral valve disease, and atrial arrhythmias.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree




