INTRODUCTION
This chapter discusses common nontraumatic conditions affecting the external, middle, and inner ear. Selected traumatic conditions include auricular hematoma, burns, and frostbite. Lacerations to the ear are discussed in the chapter 40, “Face and Scalp Lacerations.” Ear disorders in children are discussed in chapter 115, “Ear and Mastoid Disorders in Infants and Children.”
ANATOMY
The auricle, or pinna, is the visible external portion of the ear, whose trumpet shape enables it to collect air vibrations. It consists of a thin plate of elastic cartilage with a tightly adherent covering of skin. The external auditory canal is an S-shaped skin-lined tube that extends from the auricle to the tympanic membrane (TM). The outer one third of the external auditory canal is composed of an incomplete cartilaginous tube. Its thick skin supports hair follicles plus apocrine and sebaceous glands. The inner two thirds of the canal is composed of bone covered by a thin layer of tightly adherent skin, which is easily torn by minimal trauma.
The blood supply to the external ear is derived from the posterior auricular, superficial temporal, and deep auricular arteries. Venous drainage of the external ear is into the superficial temporal and posterior auricular veins, which then drain into the external jugular vein. The posterior auricular vein frequently connects to the sigmoid sinus, providing a route for extension of infected material into the intracranial cavity.
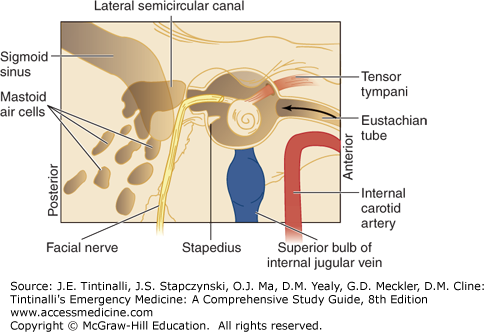
The middle ear is an air-containing cavity in the petrous temporal bone. It contains the auditory ossicles, which transmit vibrations of the TM to the perilymph of the internal ear. It communicates with the nasopharynx anteriorly via the eustachian tube and with the mastoid air spaces posteriorly via the aditus ad antrum (Figure 242-1).
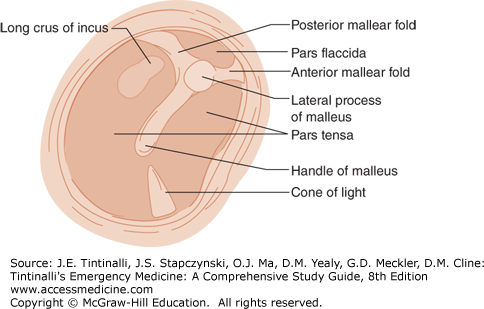
The TM is a thin, pearly gray, fibrous membrane that produces a cone-shaped light reflex anteroinferiorly when illuminated. Superiorly, the pars flaccida is the relatively slack portion of the membrane between the malleolar folds; the remainder of the membrane is tense and is called the pars tensa. The auditory ossicles are the malleus, incus, and stapes. Both the incus and the handle and lateral processes of the malleus are typically visible through the TM (Figure 242-2). Figure 242-1 shows the relationships of the facial nerve, sigmoid sinus, and internal carotid artery to the middle ear.
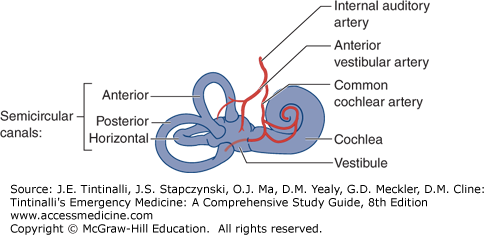
The inner ear consists of the cochlea, which contains the auditory sensory receptors, and the vestibular labyrinth, which contains balance receptors. Cristae in the semicircular canals detect angular acceleration, and macules detect linear acceleration. Afferent nerves from the vestibular labyrinth connect to brainstem nuclei to maintain smooth movement of the eyes during head movement and to the cerebellum to control oculomotor and postural functions. Blood supply is from the vertebrobasilar system (Figure 242-3). The otolithic organs (utricle and saccule) lie in the vestibule. The internal auditory artery divides into the common cochlear artery and the anterior vestibular artery. The anterior vestibular artery provides the blood supply to the anterior and horizontal semicircular canals but not to the cochlea. Isolated occlusion of the anterior vestibular artery may therefore cause acute vestibular syndrome without hearing loss.
OTALGIA
Primary otalgia is caused by auricular and periauricular disease, whereas referred otalgia is caused by disease originating from remote structures.1 Referred otalgia is common because the ear and several structures of the head and neck share sensory innervation from the fifth, seventh, ninth, and tenth cranial nerves, as well as by the cervical plexus. Table 242-1 lists common causes of primary and referred otalgia, including related neuralgias.1
| Primary | Referred |
|---|---|
| Trauma | Temporomandibular dysfunction syndrome |
| Infection | Dental |
| Otitis externa | Abscessed teeth/dental carries |
| Otitis media | Malocclusion |
| Mastoiditis | Bruxism |
| Bullous myringitis | Eustachian tube dysfunction |
| Pinna cellulitis | Retro- and oropharyngeal |
| Cerumen impaction | Tonsillitis |
| Cholesteatoma | Abscess |
| Neoplasms | Neoplasm |
| Foreign bodies | Nasal cavity |
| Sinusitis | |
| Facial Neuralgias with Periauricular Pain | Deviated septum |
| Trigeminal neuralgia | Throat and neck |
| Ramsay Hunt syndrome | Foreign body |
| Great auricular neuralgia | Thyroid disease |
| Neoplasm |
TINNITUS
Tinnitus is the perception of sound without external stimulation. It may be constant, pulsatile, high- or low-pitched, hissing, clicking, or ringing. It is most prevalent between the ages of 40 and 70 years old.2
Tinnitus is divided into two types: objective and subjective. Objective tinnitus may be heard by the examiner. Subjective tinnitus is more common. Its exact origin is unknown, although it is believed to result from damage to cochlear hair cells. Table 242-2 outlines causes of tinnitus.2
| Objective | Subjective |
|---|---|
| Vascular | Sensorineural hearing loss |
| Arteriovenous malformations | Hypertension |
| Arterial bruits | Conductive hearing loss |
| Mechanical | Head trauma |
| Enlarged eustachian tube | Medication side effects |
| Palatal myoclonus | Temporomandibular joint disorders |
| Stapedial muscle spasm | Anxiety, depression, |
| Neurologic | |
| Acoustic neuroma | |
| Multiple sclerosis | |
| Benign intracranial hypertension | |
| Ménière’s disease | |
| Cogan’s syndrome |
A number of drugs are associated with tinnitus, and some also cause hearing loss2 (Table 242-3).
| Loop diuretics | Chemotherapeutic agents |
| Ethacrynic acid | Cisplatin |
| Furosemide | Carboplatin |
| Bumetanide | Vinblastine |
| Salicylates and salicylate-containing compounds* | Vincristine |
| Nonsteroidal anti-inflammatory drugs* | Topical agents |
| Quinine | Solvents |
| Antibiotics | Propylene glycol |
| Aminoglycosides* | Antiseptics |
| Erythromycin | Ethanol |
| Vancomycin | Polymyxin B |
| Neomycin |
Accurate diagnosis usually requires referral to an otolaryngologist. Many medications have been suggested as therapies; antidepressants may help patients tolerate their tinnitus but do not change the course.
SUDDEN HEARING LOSS
Sudden hearing loss occurs over 3 days or less and is divided into sensorineural (cochlea, auditory nerve, or central auditory processing) and conductive (external ear, TM, and ossicles). Conductive hearing loss is more likely due to a reversible cause, such as otitis media, serous otitis, or a cerumen impaction. Indicators of poor prognosis include more severe hearing loss on presentation and the presence of vertigo. Table 242-43 lists causes of sensorineural hearing loss.
| Idiopathic (71.0%) | Trauma (4.2%) |
|---|---|
| Infectious disease (12.8%) | Head injury |
| Unspecified respiratory infection (viral) | Acoustic trauma |
| Meningitis* | Barotrauma |
| Group A Streptococcus | Vascular or hematologic (2.8%) |
| Epstein-Barr virus | Cardiovascular disease |
| Toxoplasma gondii | Neurovascular disease |
| Syphilis | Hemorrhage (brain) |
| Herpes simplex virus | Neoplastic (2.3%) |
| Otologic disease (4.7%) | Vestibular schwannoma |
| Meniere’s disease | Cerebellar angioma |
| Skull base or otologic surgery | Other causes (2.2%) |
| Autoimmune inner ear disease | Pregnancy related |
| Drug toxicity† | Nonotologic surgery |
Viral infections, most typically mumps, have long been associated with sudden hearing loss.4 Because of the terminal branches and interosseous location of the blood supply to the inner ear, the ear is uniquely vulnerable to a variety of vascular and hematologic diseases. Cogan’s syndrome is an autoimmune disorder that presents with a bilateral hearing loss classically associated with tinnitus and vertigo.5 Sudden hearing loss may also be caused by rupture of the TMs. Many common medications are implicated (Table 242-3).3,5
The evaluation begins with a complete history and physical examination. Differentiate conductive hearing loss from sensorineural hearing loss with a tuning fork. To perform the Weber test, place a vibrating tuning fork on the forehead and ask the patient where it is heard: it is normal to hear it equally in both ears; if the sound lateralizes to one ear, there is conductive hearing loss in that ear, or there is sensorineural loss in the opposite ear. To perform a Rinne test, place the vibrating tuning fork on skin over the mastoid bone of one ear, and then move the tuning fork to the entrance of the ear canal on the same side; the sound is normally heard better through air conduction at the entrance of the ear. If the sound is heard better over the mastoid bone, there is conductive hearing loss in that ear. Sudden conductive hearing loss may result from obstruction of the external auditory canal or from disturbances (or infection) of the TM or ossicles. Evaluate all current medications for possible ototoxic agents. A history of trauma or recollection of a “popping” noise preceding the hearing loss may indicate perforation of the TM or ossicle dislocation. Coexistent tinnitus or vertigo may point to Ménière’s disease. Also consider systemic illness.
The differential diagnosis includes both potentially reversible and potentially ominous causes (Table 242-4). If the physical examination does not identify the cause, consult otolaryngology. Treatment of idiopathic sudden sensorineural hearing loss is 60 milligrams of prednisone daily for 7 to 14 days or until follow-up, which is usually arranged within 2 weeks.5,6,7
ACUTE DIFFUSE OTITIS EXTERNA
Otitis externa includes infections and inflammation of the external auditory canal and auricle. It is divided into acute diffuse and malignant types. Acute diffuse disease is simply called otitis externa or swimmer’s ear.
Predisposing factors for the development of otitis externa are trauma to the skin of the external auditory canal and elevation of the local pH. Factors include frequent contact with water from swimming or bathing in hot tubs, pools, or freshwater lakes, and living in a humid environment. Trauma is most commonly due to scratching or overzealous disimpaction of cerumen. Cerumen is an acidic mixture of sebaceous and apocrine gland secretions and desquamated epithelial cells. It forms a physical barrier that protects the skin of the external auditory canal, whereas the acidic pH has antimicrobial properties.
The most common organisms are Pseudomonas aeruginosa, Staphylococcus aureus, Enterobacteriaceae, and Proteus species.8
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree