INTRODUCTION AND EPIDEMIOLOGY
Drowning is submersion in a liquid medium resulting in respiratory difficulty or arrest.1 As with other causes of accidental death, drowning injury typically involves otherwise healthy, young individuals, but can involve individuals of any age or background.
Worldwide, drowning accounts for >500,000 deaths annually and is the leading cause of injury death among children <15 years of age. In the United States, there are >500,000 drowning events each year and 1100 deaths, which makes drowning the second leading cause of unintentional death of individuals from birth to age 19 years old.2,3 However, the rate of drowning deaths has decreased over the past 40 years. In 1970, there were nearly 8000 deaths due to drowning in the United States,4 and education with public awareness has been the major contributor to the decreased incidence. The vast majority of victims survive submersion events, with effects ranging from minimal or transient injury to profound neurologic insult.
Drowning incidence peaks in three age groups: The highest is in children <5 years old, the second peak is in those aged 15 to 24 years, and the third peak is in the elderly. Toddlers drown primarily after falling into swimming pools or open water, but they also drown in bathtubs and buckets in the home. Physicians also need to evaluate for intentional drowning (child abuse) or factitious disorder by proxy (formerly Munchausen’s by proxy). In teenagers and adults, suicide, homicide, and domestic violence can be causes of drowning. The elderly also have an increased risk of bathtub drowning, often related to comorbid medical conditions or medications. Even in coastal areas, most drownings take place in warm, freshwater bodies of water (especially swimming pools).
Additional injuries or disorders that either precipitate or are associated with drowning events are shown in Table 215-1.
| Disorders Associated with Drowning |
Alcohol or other intoxicants Syncope (e.g., due to hyperventilation prior to underwater diving) Seizures Cardiac conditions (e.g., dysrhythmias including prolonged QT syndromes, Brugada’s syndrome, ischemic heart disease) Dementia Intentional (suicide, homicide, child abuse or neglect in young children) |
| Injuries Associated with Drowning |
Spinal cord injuries due to diving into shallow water, significant falls from heights, or boating/personal watercraft mishaps Hypothermia Aspiration Respiratory failure, insufficiency, or distress |
PATHOPHYSIOLOGY
After submersion, the degree of hypoxic insult to the central nervous system determines the ultimate outcome. It was previously thought that parasympathetic activation of the diving reflex (i.e., bradycardia, apnea, peripheral vasoconstriction, and central shunting of blood flow) provided transient protection during submersion. The diving reflex is strongest in infants <6 months of age, but the effects decrease with age.5 In adults, vertical immersion (head out) and vertical submersion (head under) activate both the sympathetic and parasympathetic systems, which blunts any effect of the diving reflex.6 Furthermore, physiologic stress associated with submersion also activates the sympathetic nervous system. Thus, the diving reflex is not protective. Cerebral protection in cold water submersions most likely results from rapid central nervous system cooling before significant hypoxic damage occurs.
Physiologic scoring systems7,8 to predict drowning outcome have been devised but are not clinically helpful. The vast majority of patients who arrive at the hospital with sTable cardiovascular signs and awake, alert neurologic function survive with minimal disability, whereas those who arrive with unsTable cardiovascular function and coma do poorly because of the hypoxic-ischemic insult. Predictors are not accurate for the 15% to 20% of drowning victims whose condition on arrival is between these two extremes.9
End organs can also be affected by hypoxemia and metabolic acidosis. Aspiration of substances such as contaminated foreign material, particulate matter, bacteria, vomitus, or chemical irritants can affect eventual pulmonary recovery. Electrolyte abnormalities are seldom significant and are usually transient unless there is significant hypoxia, central nervous system depression, renal injury from hemoglobinuria, or myoglobinuria.8,9 Hematologic values are usually normal unless there has been massive hemolysis. Disseminated intravascular coagulation can be a complicating factor in drowning outcome but usually occurs following severe hypoxic insult.
TREATMENT
Rapid resuscitation of a drowning victim (quickly restoring ventilation and oxygenation) optimizes outcome. After safe removal of the victim from the water, CPR should be initiated as quickly as possible. Trauma as a cause of drowning is uncommon, and most injured drowning patients have a history of trauma or signs of injury on examination.10 Cervical spine injury is rare (0.5%) in drowning unless there is a history of diving, falling from a significant height, or motorized vehicle crash.11 Use cervical spine precautions if the history warrants it.
Administer high-flow oxygen by facemask if the patient is breathing or by positive-pressure bag-valve mask ventilation if the patient is not breathing. For patients who do not recover spontaneous respiratory effort, endotracheal intubation and positive-pressure ventilation are necessary.
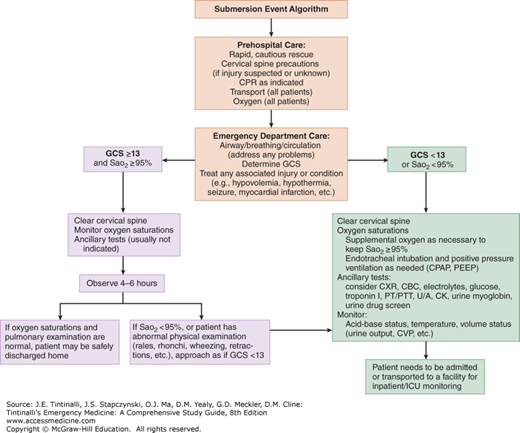
All patients with drowning amnesia for the event, loss of or depressed consciousness, or an observed period of apnea, as well as those who require a period of artificial ventilation, should be transported to an ED for evaluation, even if they are asymptomatic at the scene. The patient should be warmed and monitored, and IV access should be established (Figure 215-1).
FIGURE 215-1.
Drowning event algorithm. CBC = complete blood count; CK = creatine kinase; CPAP = continuous positive airway pressure; CVP = central venous pressure; CXR = chest radiograph; GCS = Glasgow Coma Scale score; ICU = intensive care unit; PEEP = positive end-expiratory pressure; PT = prothrombin time; PTT = partial thromboplastin time; SaO2 = oxygen saturation (via pulse oximetry); U/A = urinalysis.
Upon the patient’s arrival at the ED, assess and secure the airway, provide oxygen, determine core temperature, and assist ventilation as necessary. If the patient is hypothermic, administer warmed isotonic IV fluids and apply warming adjuncts (e.g., blankets, overhead warmers, warming devices). Address any associated injuries. Because cervical injury is rare without a history of diving or associated trauma, routine cervical immobilization and CT of the brain are not necessary.11
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree