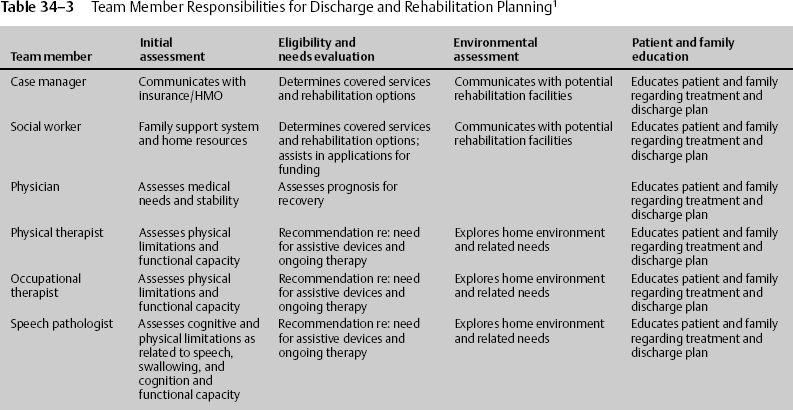
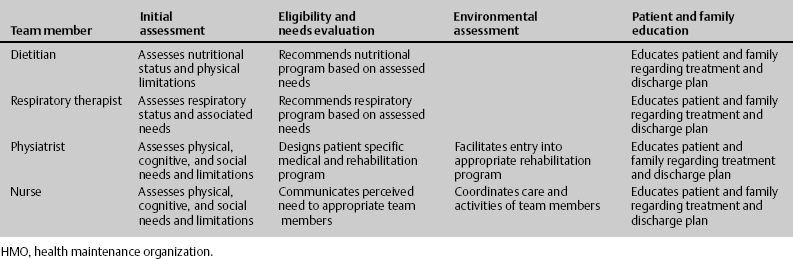
34 Paula Snyder Discharge planning in the neurosurgical intensive care unit (NICU) should begin upon admission. Neurologic patients often have increased needs for discharge. Their functional capacity may be significantly decreased because of cognitive and/or physical impairments. These patients may have tracheostomy or gastrostomy tubes, and limited or no bowel and/or bladder control. They may be at increased risk for injury due to cognitive impairment, recent memory deficits, and judgment and impulse control issues and may require constant supervision. Most inpatient rehabilitation programs require that the patient be able to participate in at least 3 hours of therapy each day. Some patients with complex medical problems may not be able to tolerate intensive rehabilitation; others may be medically stable but may not be able to participate in intensive rehabilitation due to the severity of their neurologic injury. Many of these patients may need subacute rehabilitation or skilled nursing with less intensive physical therapy. Generally, the more severe the injury or the longer the NICU/hospital stay, the longer the recovery period and the greater the need for more intensive rehabilitation or long-term care. Patients with only cognitive impairments may not qualify for inpatient rehabilitation. Early identification of the patient’s resources, community resources and outpatient rehabilitation programs, home situation and adaptability, and family support system is imperative for patients not meeting inpatient rehabilitation criteria. Patients rehabilitated on an outpatient basis will need careful evaluation and planning by the multidisciplinary team. Identification of caregivers among a patient’s family and friends is essential to a smooth discharge plan. Other areas to be assessed include (1) where outpatient therapies will be received; (2) transportation availability to and from therapies and physician visits; (3) whether home therapy is needed and, if so, whether it is covered by insurance; (4) evaluation of the home environment to identify needs for assistive devices, such as a hospital bed, commode, and a shower chair, as well as supplies (for tracheotomy care, feedings, etc.). The nurse/case manager, in concert with the multidisciplinary team, assesses the anticipated needs of the patient for discharge. The team usually consists of the nurse, physician, physiatrist, physical therapist, occupational therapist, speech pathologist, dietitian, respiratory therapist, and social worker, along with the patient and his or her family. Each team member has a specific area of responsibility related to discharge planning. Areas of particular concern when evaluating a patient for potential rehabilitation needs include motor dysfunction, alteration in sensory perception, altered communication patterns, behavioral issues, altered respiratory function, cranial nerve impairment, and cognitive impairment (Tables 34–1, 34–2, and 34–3).1
Discharge Planning in the Neurosurgical Intensive Care Unit Patient
| Alteration | Associated with/demonstrated by |
| Alteration in motor function | Associated with spinal cord injury, traumatic brain injury, and stroke resulting in paresis, paralysis, incoordination, apraxia, spasticity, and abnormal reflexes |
| Alteration in sensory perception | Blindness and visual disturbances and defects, loss or disturbance in pain, temperature, and pressure perception, position sense, agnosia |
| Altered communication patterns | Receptive, expressive, and global dysphasias, aphasia, motor dysphasia |
| Alteration in behavior | Demonstrated by mood disturbances, depression, poor impulse control, dysinhibition, anger, aggressive behavior |
| Alteration in cranial nerve function | Swallowing and speech defects, ptosis, diplopia, disruption of taste, smell, hearing, cranial nerve (CN) VII palsy |
| Alteration in cognitive function | Confusion, altered level of consciousness, impaired memory, judgment, concentration, problem solving, higher thought processes |
| Condition/situation | Discharge destination |
| Spinal cord injury (SCI) | Acute rehabilitation |
| Stroke with hemiplegia | Acute rehabilitation |
| Brain injury with paresis, paralysis, apraxia, ataxia, inability to ambulate | Acute rehabilitation vs skilled nursing facility with physical therapy vs home with outpatient therapy |
| Ventilator dependent (excluding SCI) | Subacute placement with rehabilitation/physical therapy |
| Persistent vegetative state | Skilled nursing facility vs subacute facility |
| Mild cognitive impairment | Home with outpatient therapy |
| Moderate cognitive impairment | Acute rehabilitation vs home with outpatient therapy |
| Severe cognitive impairment | Acute rehabiltiation vs skilled nursing facility |
| Sensory impairment: Blindness | Acute rehabilitation |
| Communication deficits: aphasia, dysphasia | Home with outpatient therapy |
| Behavioral issues | Home with outpatient therapy and supervision vs skilled nursing facility |
 Implications
Implications
Determining discharge destination early in the acute hospital phase can facilitate treatment decisions, resource allocation, family education, and counseling. It enables families and discharge planners to choose appropriate posthospital facilities or prepare the home environment. Case management increases patient and family understanding of posthospital needs and promotes the family’s ability to meet those needs confidently. It also decreases the length of hospital stay and costs.
Reference
< div class='tao-gold-member'>