B. Factors contributing to the difficult airway. Difficult mask ventilation, difficult laryngoscopy, and difficult intubation are factors that contribute to a difficult airway.
1. Difficult mask ventilation and difficult laryngoscopy occurs in 5% and 5.8% of patients undergoing GA for surgical procedures, respectively.5
2. A combination of difficulty mask ventilation and difficult laryngoscopy increases the risk for hypoxemia.
a. A recent trial determined the incidence of difficult mask ventilation combined with difficult laryngoscopy to be 0.4% and identified 12 independent predictors: (1) age >46 years, (2) body mass index (BMI) >30 kg per m2, (3) male sex, (4) Mallampati class III or IV, (5) neck mass or prior neck radiation therapy, (6) limited thyromental distance, (7) sleep apnea, (8) prominent teeth, (9) beard, (10) thick neck, (11) limited cervical spine mobility, and (12) limited jaw protrusion.5
b. The incidence of simultaneous difficult mask ventilation and difficult intubation in obstetrical population is unknown. Two studies show that failure of mask ventilation or SGA devices to rescue the airway in obstetrical patients can result in a high incidence of cannot intubate, cannot ventilate situations with an estimated incidence ranging from 1:95 to 1:500.6 In one recent review of GA for CD, there was one encounter of a cannot intubate, cannot ventilate situation following failed attempts at intubation and placement of an SGA, which required emergent cricothyroidotomy resulting in good outcomes in both mother and baby.6
CLINICAL PEARLRates of difficult mask ventilation and difficult tracheal intubation are increased in obstetric patients.
V.Anesthesia-related morbidity and mortality
Recent reviews of anesthesia-related maternal mortality have improved anesthesiologists’ awareness of potential airway problems in obstetric patients. The increased use of neuraxial anesthesia and advances in airway management have resulted in a decrease in the incidence of maternal brain death and mortality.2 However, cases of difficult or failed intubation are still reported, some in association with the administration of neuraxial anesthesia. An anesthesia provider must provide effective airway management when using either neuraxial or general anesthesia for CD.
A. Experience in the United States
1. In the last three decades, GA-related complications related to airway management resulting in maternal mortality have declined in the United States. Declines in anesthesia-related maternal mortality7 in the United States and the United Kingdom are similar.
a. Hawkins et al. published the first national study of anesthesia-related maternal mortality in the United States in 1997 and reported a 16.7 relative risk increase in mortality in mothers who received GA as compared with those who received neuraxial anesthesia.8 Eighty-two percent of the deaths took place during CD and most often resulted from difficult or failed intubation, inability to ventilate and oxygenate, pulmonary aspiration, and respiratory complications. The death rates during GA for CD increased from 20 per million during the interval 1979 to 1984 to 32.3 per million for the interval 1985 to 1990. The relative risk ratio of GA associated mortality was 2.3 times higher as compared to neuraxial anesthesia-related deaths. The evidence-based data hastened the change in anesthesia for pregnant patients away from GA to predominantly neuraxial anesthesia for CDs.
b. In a follow-up report, Hawkins et. al.9 reexamined and estimated trends of anesthesia-related maternal deaths in the 12 years from 1991 to 2002 and compared it to the anesthesia-related deaths from 1979 to 1990. The case fatality for GA declined from 16.8 in 1991 to 1996 to 6.5 per million in 1997 to 2002. Although the data was encouraging, 56 maternal deaths occurred during CD. Anesthesia-related mortality was most associated with complications during anesthetic induction, failure of tracheal intubation, respiratory failure, or high spinal or epidural block followed by respiratory failure.
c. Currently, anesthetic-related deaths occur in 1 of 1 million live births.9 Although the reasons for the reductions in anesthesia-related deaths are not fully understood, the improved patterns of anesthesia practice, enhanced awareness, use of protocols and difficult airway algorithms during management, and utilization of alternate airway technologies are likely responsible for the noted improvement in outcomes.
2. According to a recent ASA closed claims analysis, pulmonary aspiration in association with difficult intubation in obstetric patients may occur more often than in nonobstetric patients. The greater proportion of obstetric claims in which pulmonary aspiration was identified as the primary damaging event is noteworthy because it occurred in 15 out of the 17 patients who received GA. A strong association with difficult intubation or the sequelae of esophageal intubation was noted.10
B. Experience in the United Kingdom
1. The Confidential Enquiries into Maternal Deaths is published every 3 years in the United Kingdom. The reports show that since the early 1980s, there has been a dramatic reduction in anesthesia-related maternal deaths. Increased use of neuraxial anesthesia, aspiration prophylaxis for CD, and improvement in airway training has likely contributed to this decrease.11
a. In 1967 to 1969, there were 35 deaths directly attributed to anesthesia; in the last three reports, including the 2003 to 2005 report, an average of six deaths were considered to be a direct result of anesthetic management and associated with difficult tracheal intubation.
b. In the 2003 to 2005 report, all six GA-related deaths were deemed due to suboptimal airway management. Additionally, reviewers expressed concern regarding the proficiency of junior anesthesia practitioners in providing GA for emergency CD without supervision and discussed the need for the participation of consultants in emergency cases.11
2. Using the UK Obstetric Surveillance System (UKOSS) of data collection, a recent survey found the incidence of failed tracheal intubation in obstetric anesthesia to be 1:224. Higher maternal age, obesity, and Mallampati score >1 were significant independent predictors of failure.12
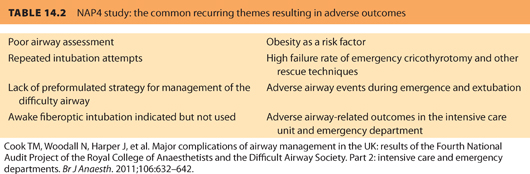
3. The Fourth National Audit Project (NAP4) of the Royal College of Anesthetists and the Difficult Airway Society were designed to study the incidence of major complications of airway management in hospitals in the United Kingdom and perform a quantitative and qualitative analysis. Four events in pregnant women, who had problems at the time of intubation during emergency CD, were examined. All of these cases took place outside of normal working hours, involved complex patients, and were managed by senior anesthetists. The airway complications noted were aspiration, a failed cricothyroidotomy attempt, and one successful surgical airway. All patients were admitted to the intensive care unit (ICU) and made a full recovery13 (see Table 14.2).
CLINICAL PEARLAlthough maternal morbidity and mortality due to GA and inadequate airway management have declined in recent decades, most anesthetic-related deaths are still associated with difficult airway management.
VI.Maternal deaths and airway-related issues following emergence
A. United States data
1. In earlier reports of airway-attributed maternal death, failed ventilation or pulmonary aspiration associated with difficult intubation at the induction of anesthesia were more commonly reported. More recent reports note the events are increasingly associated with tracheal extubation or occur in the early postoperative period.
2. A review of anesthesia-related maternal deaths in Michigan (1985 to 2003) reported that obesity and African American race were important risk factors for anesthesia-related maternal mortality.14 Most deaths resulted from hypoventilation or airway obstruction during emergence, extubation, or recovery. Vigilance in monitoring oxygenation and ventilation throughout the entire perioperative period is important.
B. Data from the United Kingdom
1. In the Confidential Enquiry into Maternal Deaths from 2003 to 2005, there were six maternal deaths related to anesthesia, a number similar to that reported during the previous triennium. Of the six deaths, one resulted from respiratory distress after tracheal extubation and two from postoperative respiratory insufficiency. No deaths resulted from airway management during induction of GA.
2. Seven anesthesia-attributed deaths were reported in the triennium 2006 to 2008 and only two of the deaths were airway related. One of the deaths was due to persistent attempts to intubate the trachea despite adequate ventilation through a laryngeal mask, and the other was the result of pulmonary aspiration following extubation of the trachea after emergency CD in a woman with a full stomach.15
CLINICAL PEARLExtubation and the postanesthetic period convey the same risk for airway-related morbidity and mortality as airway management during anesthetic induction.
VII.Anatomic and physiologic changes during pregnancy contributing in difficult airway management
Anatomic and physiologic factors alter the airway during pregnancy, placing the parturient at risk for difficult mask ventilation, difficult laryngoscopy, and difficult intubation. Difficult mask ventilation and difficult laryngoscopy may be due to excessive maternal weight gain, increased upper airway edema (further increased in preeclampsia), and breast enlargement. The respiratory (decreased functional residual capacity [FRC]) and circulatory changes during pregnancy increase the risk for hypoxemia. Gastrointestinal changes place the parturient at risk for pulmonary and respiratory-related complications.
A. Airway changes
1. The hormonal changes in pregnancy, particularly the increase in estrogen, increase the ground substance of maternal airway connective tissue, circulating blood volume, and total body water. Hypervascularity and edema of the oropharynx, nasopharynx, and respiratory tract are the result. Mallampati scores have been shown to increase during pregnancy, labor, and delivery.16
2. Excessive weight gain during pregnancy, preeclampsia, iatrogenic fluid overload, and bearing down efforts during labor can lead to increased mucosal edema.
3. Due to the increased vascularity of the respiratory mucosa and swelling of the airway, the parturient is at increased risk for epistaxis following manipulation of nasopharynx.
B. Respiratory changes
1. The gravid uterus displaces the diaphragm cephalad with progression of pregnancy and leads to a 20% decrease in FRC, which is exacerbated in the supine position.
2. Oxygen consumption and carbon dioxide production are increased by 20% to 40% secondary to the metabolic needs of the growing fetus, uterus, and placenta.
3. The decrease in FRC, along with increased oxygen consumption, shortens the safe apnea time in a parturient compared to a nonpregnant patient.
C. Cardiovascular changes
1. The gravid uterus compresses the inferior vena cava in the supine position resulting in a decrease in venous return and cardiac output. The decrease in cardiac output and the resulting hypoxemia during a difficult/failed intubation predispose the mother to the risks of myocardial hypoxemia, compromised uteroplacental perfusion, and cardiovascular arrest.
2. Left uterine displacement, establishing an airway with adequate oxygenation and ventilation in a timely manner, and maintenance of adequate perfusion in mother and baby through periods of cardiovascular stability are important in creating a safe outcome.
D. Gastrointestinal changes
1. Risk is increased for gastric regurgitation and pulmonary aspiration during a GA.
2. Decreases in gastric pH and increases in intragastric pressure are associated with an increasingly incompetent gastroesophageal sphincter and a predisposition to pulmonary aspiration.
3. The updated 2007 ASA Practice Guidelines for Obstetric Anesthesia recommend that practitioners should consider the timely administration of nonparticulate antacids, H2-receptor antagonists, and/or metoclopramide for aspiration prophylaxis in parturients undergoing CD.17
E. Recommendations for airway management: implications of the physiologic changes of pregnancy
1. Careful attention is required when evaluating and managing a parturient’s airway. Placing a nasal airway or nasotracheal tube can lead to brisk epistaxis; therefore, manipulation of the nasopharynx must be avoided if possible. The mucosal swelling decreases the area of the glottic opening and smaller size ETTs are recommended. Attempts at intubation should be gentle because the airway is more vulnerable to trauma and hemorrhage.
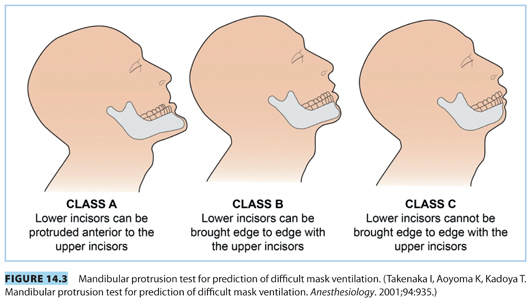
2. Increased weight gain during pregnancy and enlarged breasts can hinder laryngoscopy and result in difficult intubation. In the recumbent position, the enlarged breasts tend to fall against the neck, hindering laryngoscopy. Solutions to minimize direct laryngoscopy in these patients include (1) taping of breasts laterally and caudad, (2) use of the proper sniffing position, facilitated by the use of blankets or sheets, to create a ramp under the shoulders, and (3) use of a short laryngoscope handle.
3. The aim of proper positioning is to ensure that an imaginary horizontal line connects the external auditory meatus to the sternal notch so that the patient’s head is above the level of the chest to facilitate face mask ventilation, optimal laryngoscopy, and tracheal intubation (see Fig. 14.1).
VIII.Airway assessment
A. History. An airway history should be obtained, whenever possible, and previous anesthetic records can yield useful information regarding prior airway management.
B. Physical examination. The ASA Practice Guidelines for Obstetric Anesthesia recommend physical examination of the airway prior to initiation of anesthetic care and airway management in all patients.17
C. Specific individual tests for assessment of difficult tracheal intubation. The airway examination of the airway should focus on the following six items to assess the difficulty of tracheal intubation: (1) Mallampati classification, (2) jaw protrusion or mandibular protrusion test, (3) atlanto-occipital joint extension, (4) mouth opening, (5) thyromental distance, and (6) mentohyoid distance.
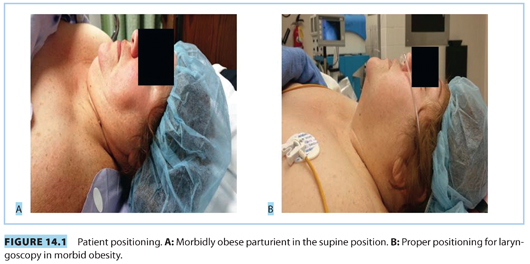
1. Mallampati classification (see Fig. 14.2)
a. The Mallampati classification has been used either as a single univariate predictor, or as a part of multivariate analysis, to predict difficult tracheal intubation. Changes in Mallampati classification during pregnancy illustrate the airway changes during pregnancy and highlight the importance of preoperative assessment of the airway. Pilkington and colleagues18 photographed women at 12 and 38 weeks of pregnancy and found that there was an increase in Mallampati class at 38 weeks. Increases were correlated with increases in body weight and advanced gestation, as well as increases in airway connective tissue and increased vascularity.
b. Kodali and colleagues16 performed a two-part study to evaluate Mallampati changes during labor and delivery. In the first part of the study, the airway was photographed at onset and at the end of labor and the Samsoon modification of the Mallampati classification was used to measure airway change. In the second part of the study, upper airway volumes were measured using acoustic reflectometry at the onset and conclusion of labor. In the first part of the study, there was a significant increase in the Mallampati class from pre- to postlabor. In the second part of the study, there were significant decreases in oral volume and pharyngeal volume area after labor and delivery.
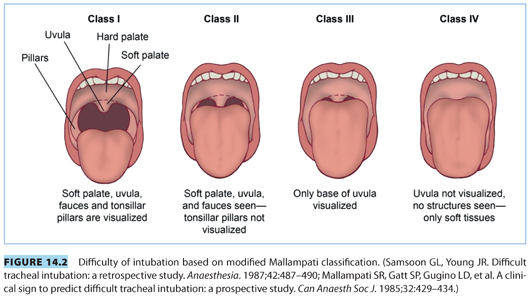
2. Jaw protrusion or mandibular protrusion test. The ability to slide the lower incisors in front of the upper ones may be classified as A, B, or C (see Fig. 14.3). Class C protrusion is often associated with difficult laryngoscopy and difficult mask ventilation, whereas Class A protrusion is rarely associated with any difficulty.19,20 Limited jaw protrusion can help predict both difficult mask ventilation and difficult laryngoscopy as a jaw thrust is required for adequate mask ventilation and movement of the mandible to expand the submental space for the tongue to ensure adequate laryngoscopy.5,19
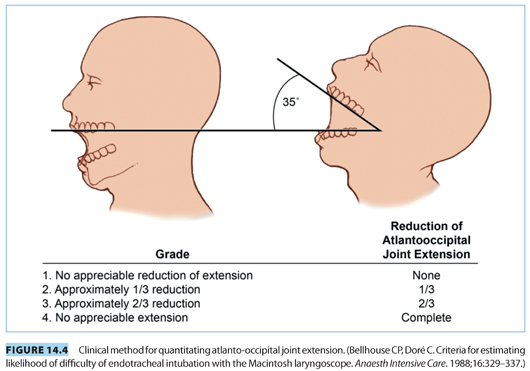
3. Atlanto-occipital joint extension. The sniffing position depends on adequate atlanto-occipital joint extension and is considered the “optimal” position of the head and neck for facilitating tracheal intubation. To measure this, the patient is asked to face directly to the front, hold their head erect, extend the head maximally, and the examiner estimates the angle traversed by the occlusal surface of the upper teeth. Normal atlanto-occipital joint extension is a 35-degree extension of the head over the neck (see Fig. 14.4). Any reduction in the extension helps predict difficulty with laryngoscopy and intubation.
4. Mouth opening. The interincisor distance is the distance between the upper and lower incisors. The normal distance is >4.6 cm; a distance <3 cm or <2 fingerbreadths is nonreassuring and may predict difficult laryngoscopy. A distance of <1 fingerbreadths will impair insertion of a regular LMA, whereas a distance of 2 cm is needed to insert an ILMA.
5. Thyromental distance. Thyromental distance is the distance from the chin (mentum) to the top of the notch of the thyroid cartilage, when the head is fully extended. This distance gives an estimate of the mandibular space into which the tongue is displaced during direct laryngoscopy and also helps to determine how readily the laryngeal axis will align with the pharyngeal axis when the atlanto-occipital joint is extended (see Fig. 14.5).
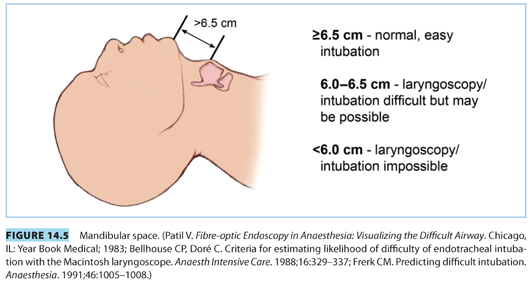
a. Thyromental distance >6.5 cm: This indicates easy intubation if no other abnormalities is present.
b. Thyromental distance 6.0 to 6.5 cm: There can be difficulty with laryngoscopy and intubation but is usually possible with the use of adjuncts for intubation such as gum elastic bougie or optical stylette.
c. Thyromental distance <6 cm: This indicates that laryngoscopy and intubation may be impossible.
6. Mentohyoid distance. Measurement of the mandibular length from the chin (mentum) to hyoid should be at least 4 cm.21 If the vertical distance between the mandible and the hyoid bone is increased, direct laryngoscopy may be encountered.
7. All of these tests have high sensitivity, but low specificity, and only moderate interobserver reliability. The low specificity of these tests, when combined with the low incidence of difficult airway, leads to a poor positive predictive value. However, a combination of these tests can predict a difficult airway more accurately.
8. Gupta and colleagues22 used a combination of Mallampati classification and the Wilson risk sum23 to predict difficult intubation in 372 obstetric patients undergoing elective and emergency CD.22 The Wilson risk sum score is calculated by adding scores of five factors, three objective, and two subjective criteria (weight, head and neck movement, jaw movement/jaw protrusion, receding mandible, and buck teeth). Combining the Mallampati classification and Wilson risk sum has been shown to improve the sensitivity, specificity, and positive predictive value for prediction of difficult airway in obstetric patients.22
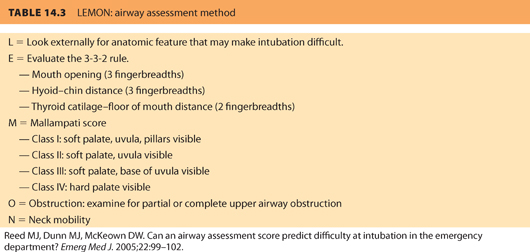
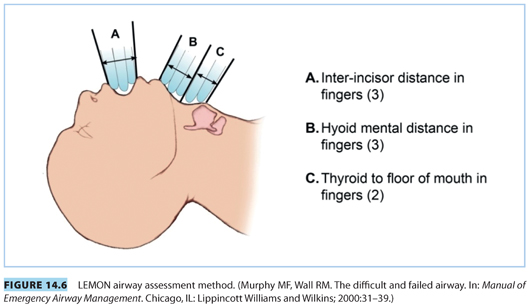
9. The “LEMON” mnemonic (developed by the U.S. National Emergency Airway Management course) labels a combination of tests to predict difficult intubation. Application is simple, quick, and can be performed on any emergency patient and has proven to have high predictive value.24 The LEMON method is an acronym for Look-Evaluate-Mallampati-Obstruction-Neck, which represents five elements for preanesthetic assessment shown in Table 14.3 and Figure 14.6.
10. Eighty-seven percent of emergency or urgent CDs can be anticipated by regular preoperative evaluation of patients admitted to the labor and delivery suite.25 The ASA recommends that all parturients undergoing an operative delivery should have a preanesthetic evaluation with emphasis on the airway examination.1 The parturient should also be evaluated for difficulty in mask ventilation (i.e., BMI >35 kg per m2, absence of teeth, snoring, etc.).26 Selection of anesthetic techniques, airway devices, and procedures will depend on airway evaluation and patient safety.
11. According to a recent obstetric anesthesia–related difficult airway survey comparing academic and private hospitals, 68% of respondents in academic institutions perform a preanesthetic evaluation on most patients in labor and delivery suite versus 39% of respondents in private hospitals.27
CLINICAL PEARLCombining the use of multiple tests of airway assessment will improve the ability of the anesthesiologist to assess the risk for difficult airway management compared to the use of single tests alone.
IX.Morbid obesity in pregnancy and the airway
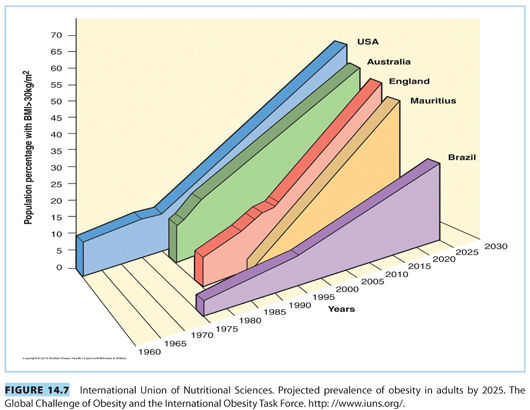
A. Prevalence of morbid obesity. The prevalence of morbid obesity in pregnancy has increased significantly over the last decade, with a significant impact on maternal morbidity and mortality (see Fig. 14.7). In 2005 to 2006, the U.S. Centers for Disease Control and Prevention reported that 34.3% of adults in the United States had a BMI above 30 kg per m2.
B. Technical challenges. Obese women pose technical challenges to obstetricians. Morbidly obese parturients are at increased risk for postpartum hemorrhage, cephalopelvic disproportion resulting in CD, hypertension, and gestational diabetes when compared with nonobese parturients.
C. Increased anesthetic risk. Obese parturients have increased anesthetic risks compared to nonobese parturients.
1. A study by Shiga et al.28 found that the incidence of difficult intubation by direct laryngoscopy increased threefold to 15.8% in patients with BMI above 30 kg per m2.
2. Obese parturients have an increased risk of difficult intubation and increased difficulty in maintaining adequate mask ventilation and are at risk for airway complications.26,29 In addition, these patients are also at risk for cardiopulmonary dysfunction and perioperative morbidity and mortality.30,31
3. In the supine position, breasts and chest wall soft tissue can hinder chest wall excursion, decrease compliance, hinder laryngoscopy, and result in difficult intubation. These problems are encountered more frequently in morbidly obese parturients (>130 kg).13,32
4. Most of the increased risk is from failed intubation and gastric aspiration during procedures that require GA.33,34 As noted earlier, a review of anesthesia-related maternal mortality from Michigan showed that obesity was a major risk factor for maternal mortality.14 Furthermore, four of the six deaths directly attributable to anesthesia from the 2003 to 2005 Confidential Enquiries into Maternal Deaths in the United Kingdom occurred in obese parturients, two of whom were morbidly obese (BMI >35 kg per m2).11
5. The ASA obstetric anesthesia closed claims files indicate that damaging events related to the respiratory system were significantly more common among obese (32%) than nonobese (7%) parturients. Furthermore, mortality was more common among obese parturients. The data illustrate the importance of increased awareness, caution, and immediate availability of resources (i.e., difficult airway algorithm) and equipment on all labor and delivery suites.10
6. The American College of Obstetricians and Gynecologists (ACOG) Committee Opinion No. 315 on Obesity in Pregnancy recommends that an anesthesiologist should be consulted before delivery when an obese parturient is identified.35 Anesthesia for both elective and emergency situations should be planned in advance with a difficult airway cart immediately available.
7. Positioning is very important to optimize the conditions for laryngoscopy and intubation in the morbidly obese parturient. Use of a ramp pillow or blankets under the shoulders to elevate the head, upper body, and shoulder above the level of the chest is strongly recommended (see Fig. 14.1).
CLINICAL PEARLMost surveys of maternal morbidity and mortality suggest that most difficult airway situations leading to poor outcomes occur in obese patients.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







