INTRODUCTION AND EPIDEMIOLOGY
Diabetes is subclassified into several different forms. Type 1 diabetes, previously referred to as insulin-dependent diabetes mellitus or juvenile-onset diabetes because of its earlier onset, is characterized by an abrupt and frequently complete decline in insulin production. Type 2 diabetes, formerly referred to as non–insulin-dependent diabetes mellitus or adult-onset diabetes, is marked by increasing insulin resistance and most commonly occurs in the overweight adult or adolescent; there is a strong genetic tendency toward the disease. The third main form of diabetes affecting children is gestational diabetes, which can affect pregnant teens as well as the infants of diabetic mothers. There has been an increase in the prevalence of type 1 diabetes of 21% between 2001 and 2009, and an increase of 31% in type 2 diabetes in the same time period.1 While the cause of the increase in type 1 diabetes is unknown, some experts suggest that the increasing prevalence of type 2 diabetes may be a result of minority population growth, obesity, exposure to diabetes in utero, and perhaps endocrine-disrupting chemicals.1 Diabetes is the most common pediatric endocrine disorder, with an estimated prevalence of 1 in 400. As many as 34% of children with new-onset type 1 diabetes present in diabetic ketoacidosis (DKA).2 In children with known diabetes, DKA is much less common and tends to be clustered in a small subset of patients, with 5% of children with diabetes accounting for nearly 60% of DKA episodes.3 DKA is the leading cause of mortality in patients with diabetes <24 years of age, and cerebral edema is the leading cause of mortality in DKA.4
PATHOPHYSIOLOGY
The fundamental cause of DKA is an absolute or relative insulin deficiency that results in the inability of cells to take up and use glucose. Levels of counterregulatory hormones (catecholamines, cortisol, growth hormone, and glucagon) are elevated, which drives many of the physiologic disturbances observed in DKA. These hormones increase glucose production by promoting glycogenolysis, gluconeogenesis, lipolysis, and ketogenesis, and further decrease glucose utilization by antagonizing insulin.
As the serum glucose level exceeds the renal absorption threshold, an obligatory osmotic diuresis ensues, which results in the classic symptoms of polyuria and polydipsia. If not recognized early, this can lead to profound dehydration and electrolyte disturbances. Acidosis stems from the complex metabolic derangements induced by insulin deficiency and unopposed glucagon. The cellular milieu of the body is essentially in a state of functional starvation, unable to use the excess serum glucose. Decreased lipid uptake by adipose tissue and increased lipolysis result in an overabundance of circulating free fatty acids, which are converted by the liver into the ketoacids acetoacetate and β-hydroxybutyrate.
Despite this profound shift in substrate production, ketoacid utilization and renal elimination are both impaired, which results in a wide anion gap metabolic acidosis. In certain patients, the acid-base status may be more complex. Persistent vomiting and severe volume depletion may result in a superimposed metabolic alkalosis that may mask the severity of the acidosis by producing a relatively normal pH. Severe dehydration and poor perfusion further lead to lactic acidosis, which results in a superimposed anion gap acidosis. Alternatively, a patient who remains relatively well hydrated will lose sodium with keto anions in the urine while retaining chloride and demonstrate a significant non–anion gap acidosis.
See the chapters 223 and 224, “Type 1 Diabetes Mellitus” and “Type 2 Diabetes Mellitus,” respectively, for more discussion of the pathophysiology of diabetes.
CLINICAL FEATURES
Polyuria, polydipsia, and polyphagia are the classic symptom triad of type 1 diabetes. Other common symptoms include weight loss, secondary enuresis, anorexia, vague abdominal discomfort, visual changes, and genital candidiasis in a toilet-trained child. The diagnosis is established by demonstrating hyperglycemia and glucosuria in the absence of other causes such as steroid therapy, Cushing’s syndrome, pheochromocytoma, hyperthyroidism, or other rare disorders. Signs of uncontrolled diabetes span the entire spectrum from simple hyperglycemia without ketonuria to diabetic ketosis (hyperglycemia with ketonuria) to full-blown DKA.
DKA
DKA is generally defined as a metabolic acidosis (pH <7.30 or serum bicarbonate level of <15 mEq/L) with hyperglycemia (serum glucose level of >200 milligrams/dL or 11 mmol/L) and ketonemia or ketonuria.5,6 DKA is much more common in patients with type 1 diabetes than in those with type 2, but it is not uncommon for patients with type 2 to develop acidosis under moderately severe physiologic stress. This acidosis has been referred to as the hyperglycemic hyperosmolar state, which can result in severe total body water, potassium, and phosphorus deficits. Hyperglycemic hyperosmolar state, which is estimated to account for 1% of all diabetic admissions, has a case fatality rate of 5% to 20%.5,7
In the patient with known diabetes, the diagnosis of DKA is relatively straightforward. The most common cause of DKA in children and adolescents with known diabetes is poor adherence to the prescribed insulin regimen. Other precipitants include intercurrent viral illness and focal infections such as urinary tract infection or gastroenteritis. Patients complain of polydipsia and polyuria (if not dehydrated), diffuse nonfocal abdominal pain often associated with vomiting, difficulty breathing, and generalized malaise, in addition to any localizing complaints related to a precipitating trigger. Kussmaul breathing may be mistaken for pulmonary pathology or even anxiety with hyperventilation.
Physical findings in DKA are due to dehydration and metabolic acidosis. Children appear dehydrated, are tachycardic, and may be hypotensive. Respiratory compensation for acidosis is noted in the deep Kussmaul respirations, which may be accompanied by paresthesias. Acetoacetate is converted to acetone and is responsible for the classic breath odor of nail polish. The level of consciousness may range from alert to somnolent to comatose. In a child with DKA and a depressed level of consciousness, consider the development of cerebral edema.
Abdominal pain and vomiting often accompany DKA. Distinguish nonspecific abdominal pain or gastroenteritis from more serious intra-abdominal disorders such as acute appendicitis. Focal abdominal tenderness, failure of pain to resolve with fluid therapy, and associated fever suggest an underlying intra-abdominal process.
An elevated glucose level in the presence of ketonemia/ketonuria and acidosis almost always indicates DKA. However, other rare conditions possess similar clinical characteristics. Any condition resulting in prolonged vomiting or excessive fasting can result in ketoacidosis, but the glucose level is not elevated. In adolescent patients without known diabetes, consider toxic ingestions of ethylene glycol, isopropyl alcohol, or salicylates.
CEREBRAL EDEMA
Cerebral edema, which occurs in approximately 0.5% to 1% of all children presenting with DKA, is the most dreaded complication, accounting for 60% to 90% of all pediatric DKA-associated deaths.4 Mortality rates range from 21% to 24%, and only 14% to 57% of children who develop the disorder recover neurologically normal.8 Cerebral edema more commonly develops in children <5 years old and is rare in persons >20 years old (see Table 145-1).8 It is likely that all patients with severe DKA have some degree of subclinical cerebral edema,9 but the specific risk factors associated with overt, life-threatening cerebral edema are young age, severe hyperosmolality, persistent hyponatremia, and severe acidosis.5,8 Failure of serum sodium level to rise commensurately with the fall in glucose level during therapy may be an important predictor.8 Newer studies refute the belief that overaggressive fluid resuscitation per se is a significant risk factor.2,10 The incidence of cerebral edema has not changed over the past 15 to 20 years, despite the introduction of gradual rehydration protocols over the same interval.10 Furthermore, a randomized study of two rehydration protocols in DKA was assessed for the risk of associated MRI-documented subclinical cerebral edema and showed no difference in the rate of cerebral edema between an aggressive and a more judicious rehydration protocol.11 A vasogenic process has been postulated as the predominant mechanism of cerebral edema formation in DKA rather than osmotic cellular swelling.9,12 A study using perfusion MRI during DKA treatment in children demonstrated increased cerebral blood flow suggesting a difference in the hemodynamic states of dehydrated and resuscitated children with DKA. The authors further noted that the patients with greater dehydration and more profound hypocapnia had an increased risk of cerebral edema, possibly as a result of cerebral hypoperfusion and ischemia prior to treatment.12 Regardless of the exact mechanism, caution in fluid administration is prudent, particularly in the extremely hyperosmolal child (i.e., osmolarity of >340 mOsm/L).
Factors indicating high risk
Prevention
Treatment
|
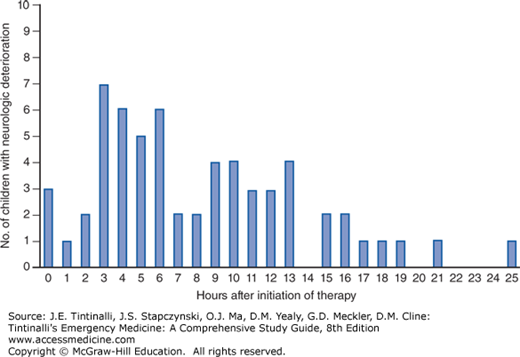
Cerebral edema typically manifests itself 6 to 12 hours after the onset of therapy (Figure 145-1).5 Many children appear to be improving clinically and biochemically prior to deterioration from cerebral edema. Premonitory symptoms occur in as few as 50% of patients and include severe headache, declining mental status, seizures, and papilledema. Unfortunately, respiratory arrest may be the first sign of cerebral edema. Early aggressive intervention based on the clinical evaluation, often before confirmatory CT findings, is vital to prevent respiratory arrest, herniation, and death.8,13 Once respiratory arrest has occurred, meaningful recovery is unlikely.8
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree