Chapter 37
Delirium in the Intensive Care Unit
Diagnosis and Treatment 
Delirium is defined as an acute brain dysfunction with a set of characteristic clinical features (Box 37.1). Delirium occurs in 50% to 80% of patients in intensive care units (ICUs). Although causality has not been established, delirium in ICU patients is associated with longer hospital stays, new cognitive impairment at discharge and often long-term postdischarge, and an increased risk of mortality after adjusting for possible confounding factors.
Diagnosis
Although various methods have been previously used for the recognition of delirium in the ICU, the Confusion Assessment Method for the Intensive Care Unit (CAM-ICU) is currently the most widely used method (Figure 37.1 and Figure 37.E1). ![]() CAM-ICU encompasses all aspects of the traditional definition of delirium; allows for the assessment of nonverbal patients; and has a sensitivity between 93% and 100%, a specificity between 98% and 100%, and excellent interrater reliability. In addition, it can be used for serial bedside monitoring by clinicians and takes ∼2 minutes to complete with minimal training. It can even be used to assess patients who are intubated or who have baseline dementia or severe depression. The CAM-ICU worksheet guides the practitioner through these steps and allows for objective documentation of changes in delirium from day to day (Figure 37.E2)
CAM-ICU encompasses all aspects of the traditional definition of delirium; allows for the assessment of nonverbal patients; and has a sensitivity between 93% and 100%, a specificity between 98% and 100%, and excellent interrater reliability. In addition, it can be used for serial bedside monitoring by clinicians and takes ∼2 minutes to complete with minimal training. It can even be used to assess patients who are intubated or who have baseline dementia or severe depression. The CAM-ICU worksheet guides the practitioner through these steps and allows for objective documentation of changes in delirium from day to day (Figure 37.E2) ![]() .
.
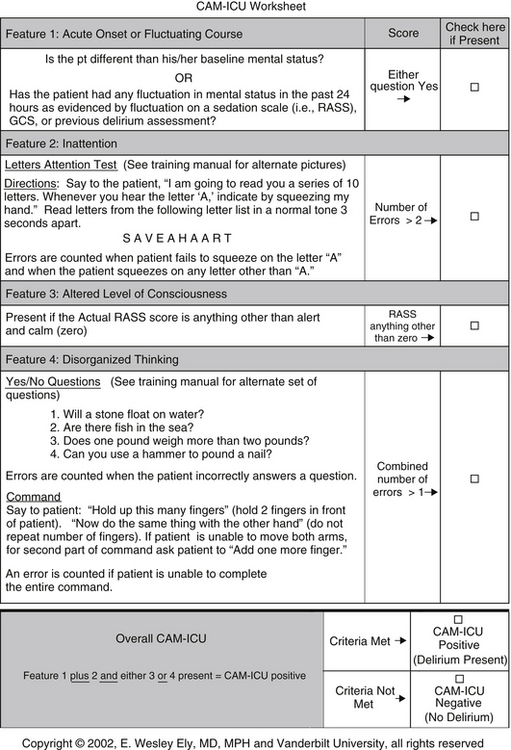
Figure 37.1 Confusion Assessment Method for the Intensive Care Unit (CAM-ICU) worksheet to assess for the presence of delirium. RASS, Richmond Agitation-Sedation Scale (see Table 5.1 in Chapter 5); GCS, Glasgow Coma Scale. (Copyright © 2002, E. Wesley Ely, MD, MPH, and Vanderbilt University, all rights reserved.)
As the CAM-ICU worksheet (Figure 37.1) shows, one should first evaluate the patient for degree of sedation. This is best accomplished by using the Richmond Agitation-Sedation Scale (RASS) (see Table 5.1 in Chapter 5). Quantifying sedation levels by means of the RASS not only allows clear goals to be set for the amount of sedative needed but also allows the ICU practitioner an objective and reliable scale to monitor the fluctuations in a patient’s level of arousal, the first component in the CAM-ICU assessment. If the patient’s RASS score has changed since a previous assessment or there is an acute change in mental status, the first feature of delirium is considered to be present.
Once an acute change from baseline or fluctuation in mental status is determined to be present, the second feature of delirium, inattention, can be assessed using the Letters Attention Test (see Figure 37.1). This consists of having the patient squeeze the examiner’s hand when the examiner says certain letters aloud. If the patient is unable to perform this test, a set of pictures is also included in the CAM-ICU (www.ICUdelirium.org) to assess for inattention.
Treatment
Nonpharmacologic Preventive Measures
Nonpharmacologic preventive measures aimed at some of the multiple possible causes can reduce the risk of delirium in ICU patients. These include frequent orientation by caregivers, early mobilization, sleep protocols including lights on during daylight hours and off at night, removal of restraints and catheters in a safe and timely manner, and minimizing unnecessary noise (See Chapter 44). Also, the RASS can be used to set a target goal of sedation to reduce the practice of giving more sedatives or opioids than necessary to achieve the desired level (see Chapter 5). ICUs may have a sedation-analgesia protocol to use for intubated and ventilated patients (Figure 37.E3). Likewise, some ICUs may have a delirium-related protocol (Figure 37.E4). ![]()
Nonpharmacologic and Pharmacologic Treatment Interventions
Even with preventive measures, however, delirium in ICU patients still occurs and must be diagnosed and treated in a timely manner. The goal is to decrease the risk of injury to self or staff as a result of delirium-associated agitation and possibly the risk of long-term cognitive impairment and even death.
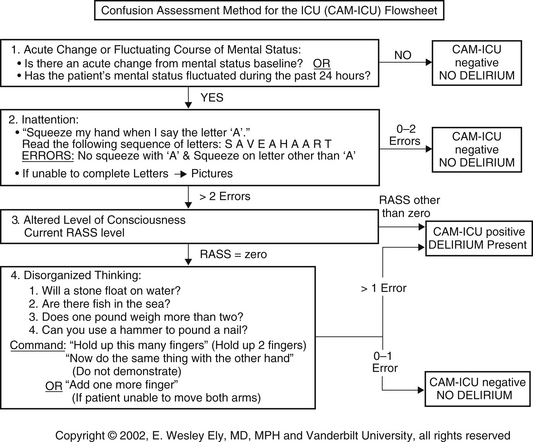
Figure 37.E1 Confusion Assessment Method for the Intensive Care Unit (CAM-ICU) flow sheet to assess for the presence of delirium. This is a shortened version of CAM-ICU worksheet (see Figure 37.1) (www.icudelerium.org). RASS, Richmond Agitation-Sedation Scale. (Copyright © 2002, E. Wesley Ely, MD, MPH, and Vanderbilt University, all rights reserved.)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



