PURPOSE OF PROCEDURE
Defibrillation is the therapeutic use of electricity to depolarize the myocardium so coordinated contractions can occur. The term defibrillation is usually applied to an attempt to terminate a nonperfusing rhythm (e.g., ventricular fibrillation or pulseless ventricular tachycardia).
Cardioversion is the application of electricity to terminate a still perfusing rhythm (e.g., ventricular tachycardia with a pulse, supraventricular tachycardias including atrial arrhythmias) to allow a normal sinus rhythm to restart. By this definition, cardioversion is a less urgent procedure compared to defibrillation, although the patient requiring cardioversion may be hypotensive or hemodynamically unstable, rather than in cardiac arrest.
PATIENT SELECTION
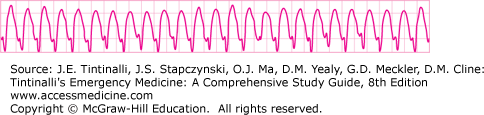
Indications for defibrillation include ventricular fibrillation (VF) (Figure 23-1) and pulseless ventricular tachycardia (VT) (Figure 23-2). Defibrillation is not indicated for asystole and pulseless electrical activity and is contraindicated for sinus rhythm, a conscious patient with a pulse, or when there is danger to the operator or others (e.g., from a wet patient or wet surroundings).
Cardioversion is indicated for a hemodynamically unstable patient with VT, supraventricular tachycardia, atrial flutter, or atrial fibrillation. It is also possibly indicated after failed pharmacologic therapy for the previously mentioned arrhythmias, especially if the patient becomes hemodynamically unstable. Cardioversion should be synchronized, which means the electric current will be timed with the patient’s intrinsic QRS complexes, to minimize the risk of inducing VF.
RISKS AND PRECAUTIONS
Electrical energy can terminate an abnormal rhythm, but if inappropriately delivered, it can also induce VF. This can happen if the electric shock is delivered during the relative refractory portion of the cardiac electrical activity.1
When preparing for defibrillation, check the patient and rhythm to ensure that a shock is truly indicated. Movement artifacts or loose leads may look like VF. New defibrillator technology is available that can filter compression or movement artifacts to “see through” the underlying rhythm. However, when using automated external defibrillators (AEDs), all manufacturers currently still recommend stopping all compressions and patient movement (e.g., during transport) before initiating analysis mode.
Make sure that no rescuer is inadvertently in contact with the patient when a shock is delivered. Neither single nor double gloves provide the rescuer with complete safety from current,2 so we still recommend “stand clear” drills during defibrillator training, “stand clear” practice during actual defibrillation, and minimizing rather than eliminating the pause in compressions for defibrillation. If the patient is on a wet or conducting surface, move the patient to a safe area and dry the body before delivering the shock. When using manual defibrillation paddles, make sure that the paddles are either on the defibrillator cradle or on the patient’s chest, with minimal time in transit from one position to the other. To prevent inadvertent discharges, always point the paddles downward and never wave the paddles around or face them toward each other, especially when charged. This is to prevent inadvertent discharges or “sparking.”
To avoid skin burns, remove all metallic objects and nitroglycerin patches from the patient. Ensure correct placement of defibrillation paddles/pads and remove all direct sources of oxygen to avoid fire.3,4 If paddles are used, do not allow the conducting gel to spread to within 5 cm of the other paddle. In patients with an internal pacemaker requiring defibrillation, ensure that the paddles/pads are placed well away (12.5 cm or 5 inches) from the pacemaker before discharging.
Avoid prolonged pauses (>10 seconds) to CPR when performing defibrillation.5,6 Thus, the emphasis is on minimal interruptions to CPR for analysis, a single shock instead of three “stacked” shocks, and immediate resumption of CPR without a pulse or rhythm check immediately after defibrillation. In addition, if a mechanical CPR device is being used, defibrillation can be safely performed without stopping ongoing mechanical compressions to reduce unnecessary pauses.
EQUIPMENT
Defibrillator: This can be a manual, semi-automated, or fully automated external defibrillator.
Paddles or self-adhesive defibrillation pads.
Conductive gel or gel pads for defibrillation paddles.
Related resuscitation equipment (e.g., bag-valve mask device, airway devices, suction, IV cannulation, drugs).
Defibrillators should be properly maintained and in a constant state of readiness. We recommend the use of checklists7 to identify defibrillator malfunction and ensure proper maintenance of batteries. Users should be trained in the proper use of checklists, and checks should be performed frequently (as often as every shift). Perform cardioversion in a resuscitation area with appropriate monitoring and standby resuscitation equipment, in case the patient deteriorates or develops cardiac arrest.