Fig. 47.1 Chest X-ray
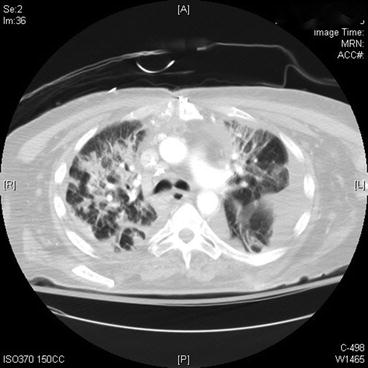
Fig. 47.2 Chest computed tomography
- 1.
What do the images above show and what is the differential diagnosis based on the appearance seen in the images above?
- 2.
What is the current definition of acute respiratory distress syndrome?
- 3.
Name some common triggers for the development of ARDS.
- 4.
What is the approach for mechanical ventilation on patients with the above diagnosis?
- 5.
Is there an indication for steroids, statins, or neuromuscular blockade (NMB) in ARDS?
- 6.
Which nonconventional therapies can be used to enhance oxygenation in severe ARDS?
- 7.
What is the role of nitric oxide and prostaglandins in ARDS?
Answers
- 1.
The chest X-ray (Fig. 47.1) shows diffuse bilateral coalescent opacities, whereas the CT chest (Fig. 47.2) shows ground-glass opacification, reflecting an overall reduction in the air content of the affected lung. It is also possible to visualize bronchial dilatation within areas of ground-glass opacification. Differential diagnosis include (a) ARDS, (b) congestive heart failure, (c) pulmonary hemorrhage, (d) pneumonia, (e) transfusion-related acute lung injury, and (f) non-cardiogenic pulmonary edema.
- 2.
The Berlin definition, dated 2012, states that acute respiratory distress syndrome is an entity characterized by hypoxemia and stiff lungs that occurs within a week of a known clinical insult or new/worsening respiratory symptoms. It presents with bilateral opacities on the chest X-ray involving at least three quadrants that are not fully explained by effusions, atelectasis, or nodules. Chest computed tomography (CT) findings are opacification that is denser in the most dependent regions as compared to more normal and hyper-expanded lung in the nondependent ones. In addition, CT chest shows widespread ground-glass attenuation, which is a nonspecific sign that reflects an overall reduction in the air content of the affected lung. Respiratory failure in ARDS must not be fully explained by cardiac failure, and an objective assessment for exclusion of such cause may be necessary by echocardiography. Finally, ARDS is classified as mild, moderate, or severe based on PaO2/FiO2 ratio and PEEP. If PaO2/FiO2 ratio is between 200 and 300 mmHg with PEEP ≥5, it is classified as mild. If PaO2/FiO2 ratio between 100 and 200 mmHg with PEEP ≥5, it is moderate. PaO2/FiO2 ratio less than 100 mmHg with PEEP ≥5 is classified as severe. Note that the term acute lung injury has been removed, as well as the requirement of pulmonary capillary wedge pressure ≤18 mmHg [1].
- 3.
Get Clinical Tree app for offline access
Common risk factors for ARDS are divided into two categories: direct and indirect.
- (a)
Direct causes are pneumonia, aspiration of gastric contents, inhalational injury, pulmonary contusion, pulmonary vasculitis, and drowning.
- (b)
Indirect causes are non-pulmonary sepsis, major trauma, pancreatitis, severe burns, non-cardiogenic shock, drug overdose, and multiple transfusions or transfusion-associated acute lung injury (TRALI).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



- (a)


