CHAPTER 164
Cutaneous Larva Migrans
(Creeping Eruption)
Presentation
The patient has an intensely pruritic, thin, erythematous, serpiginous, raised eruption on the sole of the foot, hand, or buttock (Figure 164-1). The patient may remember recently walking barefoot or sitting in the sand or soil in an area frequented by dogs or cats. Most commonly, this is seen in travelers returning from tropical or subtropical locations in the Caribbean, Central America, and South America, as well as in the southeastern United States.
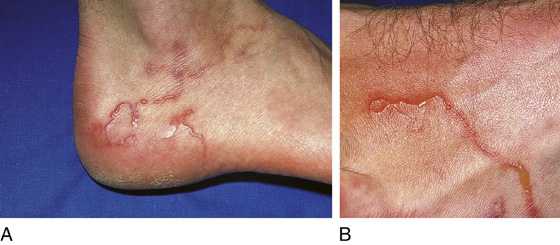
Figure 164-1 A and B, Cutaneous larva migrans. (From White G, Cox N: Diseases of the skin, ed 2. St Louis, 2006, Mosby.)
This is a dog or cat hookworm infection. Beaches and sandboxes provide excellent reservoirs for these parasites. Humans become a dead-end host for the microorganisms by walking through contaminated areas with bare feet or with open footwear, or by sitting in the tainted sand or soil.
What To Do:
 Prescribe ivermectin (Stromectol), 200 µg/kg, one single dose (supplied as 3-mg tablet). Alternatively, prescribe albendazole (Albenza), 200 mg PO bid, or 400 mg qd (supplied as 200-mg tablet or in a 200 mg/mL suspension) × 3 days, or topical thiabendazole lotion, tid × 7 to 10 days (pharmacist formulated—these dosages are the same for both adults and pediatric patients).
Prescribe ivermectin (Stromectol), 200 µg/kg, one single dose (supplied as 3-mg tablet). Alternatively, prescribe albendazole (Albenza), 200 mg PO bid, or 400 mg qd (supplied as 200-mg tablet or in a 200 mg/mL suspension) × 3 days, or topical thiabendazole lotion, tid × 7 to 10 days (pharmacist formulated—these dosages are the same for both adults and pediatric patients).
 Although it is only mildly effective, it may still be helpful to prescribe hydroxyzine (Atarax, Vistaril), 25 to 50 mg qid, or diphenhydramine (Benadryl), 25 to 50 mg qid prn to reduce itching.
Although it is only mildly effective, it may still be helpful to prescribe hydroxyzine (Atarax, Vistaril), 25 to 50 mg qid, or diphenhydramine (Benadryl), 25 to 50 mg qid prn to reduce itching.
What Not To Do:
 Do not refer patients for cryotherapy. This was a historic treatment but has been shown to be ineffective and sometimes locally harmful.
Do not refer patients for cryotherapy. This was a historic treatment but has been shown to be ineffective and sometimes locally harmful.
Discussion
This disease is now usually referred to as creeping eruption, cutaneous larva migrans, or both. To be more precise, it has been proposed that the term “hookworm-related cutaneous larva migrans” be used to describe the cutaneous migration of larvae of animal hookworms in humans.
These lesions result from infestation by the skin-penetrating filiform larvae of hookworms (Ancylostoma braziliense, Ancylostoma caninum, Uncinaria stenocephala, and others) that hatch from eggs that are passed in dog and cat feces. If a human accidentally comes into contact with soil or sand contaminated by these animal droppings, these larvae may then penetrate through the skin. The incidence of this rash is greatest in warm, moist, sandy areas, such as tropical beaches.
Migration of the larvae at several millimeters per day results in the characteristic meandering, snakelike burrows in the epidermis. During larval migration, a local inflammatory response is provoked, which causes moderate to intense pruritus. Man is not the normal host for these parasites, and therefore, the microorganisms lack the necessary collagenase to disrupt the basement membrane beneath the epithelial cells. Therefore the larvae usually die within 2 to 8 weeks, even without treatment, but may persist for up to 1 year. Lesions are mostly localized on the feet, but they also appear on the buttocks and thighs, trunk, and knees. The diagnosis of this parasitosis is essentially clinical and relies entirely on history and physical findings.
The use of topical compounds (e.g., 10% thiabendazole) is all too frequently accompanied by irritation, recurrence, and poor patient compliance. Ivermectin and albendazole, on the other hand, are effective and fast: 24 to 48 hours are enough to stop the larvae from migrating, with consequent regression of pruritus. The skin heals in 2 to 3 weeks, and adverse reactions are rare. Therefore, although hookworm-related cutaneous larva migrans is self-limited, medical treatment shortens the duration and may prevent complications such as impetigo that results from scratching.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



