CHAPTER 41
Cumulative Trauma Disorder
Stephen A. Ferrara, DNP, RN, FNP-BC, FAANP
Cumulative trauma disorder (CTD) and repetitive strain injury are collective terms for a range of soft-tissue injuries and conditions that primarily involve tendons, tendon sheaths, muscles, or nerves, and are characterized by discomfort, paresthesia, numbness, weakness, impairment, or persistent pain in the joints, muscles, tendons, and other soft tissues, with or without physical manifestations. Although they have been described in the literature since the 1700s, CTDs have received increased attention because of changes in occupational and recreational activities, as well as advances in the field of ergonomics. The legal profession and issues of workers’ compensation have also been driving factors in this resurgence. Although CTDs can also involve the lower extremities, such as the patellar and Achilles tendons, this chapter focuses on the common CTDs of the upper extremity that a primary care provider is likely to encounter.
Many common daily activities at home, at work, and in the community require functional upper extremities. The upper extremities are used to perform basic activities such as dressing and eating, to communicate with others through gesturing and writing, to operate machinery and recreational equipment, and to meet the many demands inherent in a tactile world. When the upper extremity cannot function as desired because of pain, weakness, numbness, or paresthesias, problems occur. Concerns may arise regarding ability to meet demands at home, at work, and in social or recreational situations. Given the impact that upper-extremity dysfunction can have, thorough evaluation, proper diagnosis, and adequate treatment are essential.
 ANATOMY, PHYSIOLOGY, AND PATHOLOGY
ANATOMY, PHYSIOLOGY, AND PATHOLOGY
Anatomy and Physiology
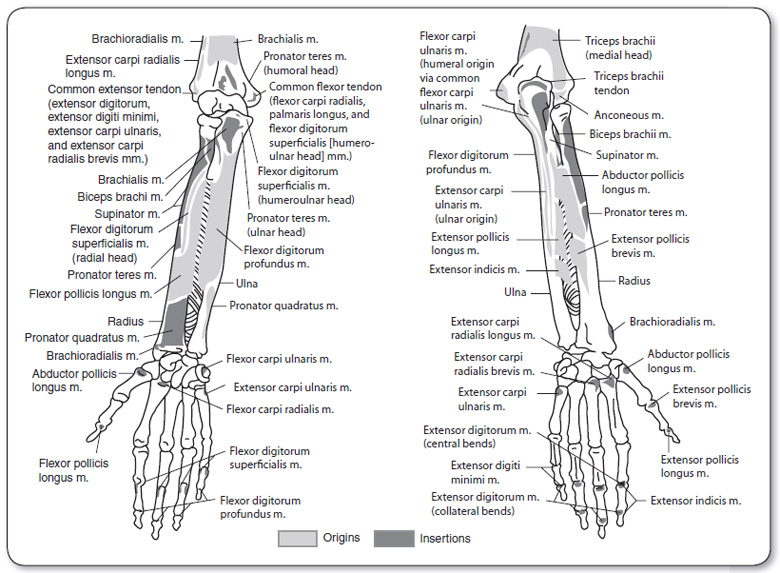
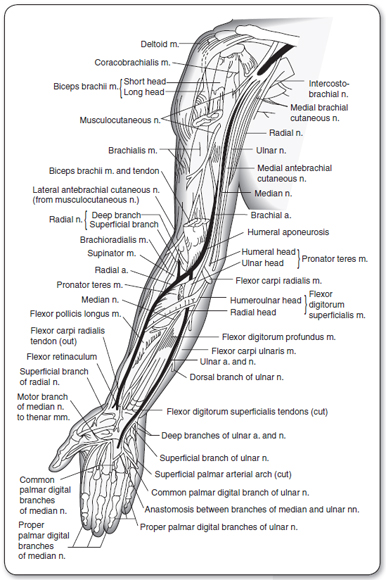
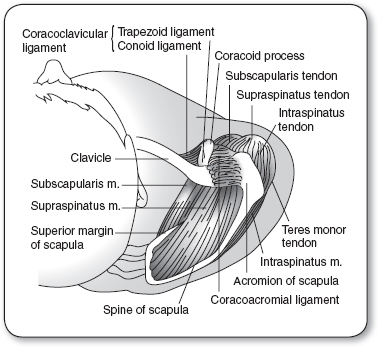
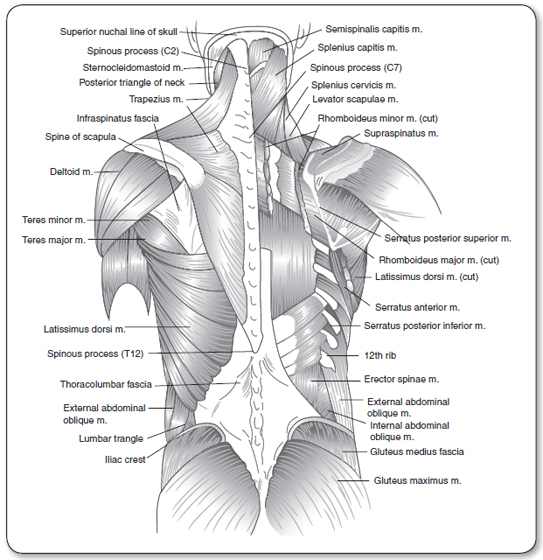
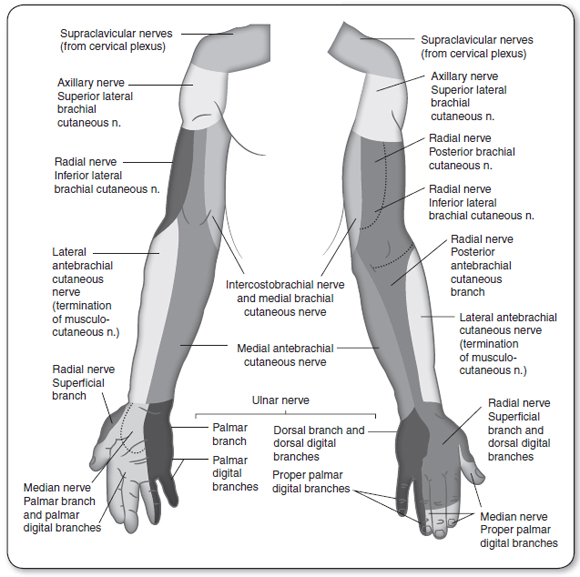
The provider needs a working knowledge of the bones, muscles, tendons, nerves, and vessels of the upper extremity, neck, and back (Figures 41.1–41.4). The hand is innervated by the median, ulnar, and radial nerves. Each nerve passes through a muscle in the forearm, and each passes through potential points of entrapment. These nerves are involved in the control of the wrists, fingers, and thumbs. The sensory branches of the nerves are depicted in Figure 41.5.
Pathology
Although the etiology of CTDs remains controversial, two distinct views are emerging. One perspective is that CTDs are the result of a musculotendinous injury caused by force, repetition, abnormal postures, and vibrations over time. The second perspective is that workplace psychosocial factors account for conditions identified as CTDs (National Research Council & Institute of Medicine, 2001). No single explanation for the diversity of disorders and the multiplicity of symptoms has been identified, but there is consensus that these disorders develop gradually and are not the result of a single episode of trauma (Armstrong, Fine, Goldstein, Lifshitz, & Silverstein, 1987a; Higgs, Edwards, Seaton, Feely, & Young, 1993; Mackinnon & Novak, 1994; Putz-Anderson, 1988).
 PHYSIOLOGICAL PERSPECTIVE
PHYSIOLOGICAL PERSPECTIVE
Three hypotheses, either in isolation or in combination, support the perspective that CTDs are a result of a musculotendinous injury (Mackinnon & Novak, 1994). The first hypothesis purports that muscle and tendon overuse is the primary etiology of CTDs. The second hypothesis maintains that there is a neurogenic origin to CTDs. The third hypothesis is based on an integration of neuropathic compression, myofascial pain, and muscle imbalance. A summary of each is provided here.
Muscle and Tendon Overuse
The premise behind the first hypothesis is that pain results directly from an overused muscle or as a result of pathological changes that occur in the muscle fibers of overused muscles. With repetitive motion, there is reduced relaxation and increased tension in these tissues, reducing essential blood supply. This can lead to a rapid rate of wear and tear, with a greatly reduced ability to repair. Over time, a cumulative overload results in inflammation, edema, compression, ischemia, tearing, and fibrosis of affected tissues.
When muscles hold their contraction at more than about 15% to 20% of their maximal capability, they pull on their tendons and compress their joints, which decrease the blood supply to the tissues (Hebert, 1993). This can result in tissue ischemia and delayed dissipation of metabolites, causing irritation and inflammation. Additionally, overstrain of the muscles can cause microtears at the tendinous insertions; this leads to less diffusion, which causes a relative ischemia and subsequent inflammation at the tendon insertion. This results in mechanical attrition, a thickening of the tendon with irregular surfaces, and further abrasions and tearing (Childre & Winzeler, 1995). When there is insufficient time between episodes of heavy usage for a tissue to recover or repair itself, CTD can occur (Frederick, 1992; Hebert, 1993).
When a muscle or tendon unit is repeatedly tensed, the end result can be tendinosis (Khan, Cook, Kannus, Maffulli, & Bonar, 2002; Maffulli, Khan, & Puddu, 1998). The term tendinitis has traditionally been used to describe this condition, which was believed to be predominantly inflammatory in nature. However, histological examination of these tissues reveals minimal inflammation (Khan, Cook, Bonar, Harcourt, & Astrom, 1999). Tendons have both a biomechanical and a physiological response to stressors. Tendons function as mechanical links that transmit forces, stabilize movements, and move the kinematic chains of the extremities. Consequently, tendons are subjected to tensile stresses by the muscle and to compressive and shearing stresses from adjacent bones and ligaments. Tendons respond mechanically to these stresses; if the stresses exceed a certain point, the tendons can become deformed. Normal tendon structure can be disrupted in response to three stressors: tension, compression, and abrasion secondary to friction (Gross, 1992). Mechanisms of injury may involve stressors that are too high in magnitude, too frequent in repetition, or both. Local mechanical stresses can also irritate tendons via excessive force or high frequency of physical contact between soft tissues and an object or tool in the work environment.
Tendons also respond physiologically to stressors. Physiological responses include metabolic, circulatory, and adaptive changes in the accessory tissues, synovial and mesenteric membranes, and adjacent ligaments. The changes are likely to be related to the occlusion of blood flow and the subsequent deprivation of nutrients that can occur with compression of a tendon against adjacent surfaces, thickening of tendon sheaths, or increased diffusion distances because of thickened sheaths (Manske, Ogata, & Lesker, 1985). Therefore, chronic degenerative changes in tendon structure reflect scarring and/or a failed healing response rather than inflammation processes.
A typical inflammatory response is seen, however, with ruptures of the tendon (Legerlotz, Jones, Screen, & Riley, 2012). These tendon ruptures may be micro, partial, or complete. The tendon area will swell and feel warm, tender, and painful. Movement is limited as a result of increased muscle tension and muscle spasm. If this occurs repeatedly, the frequent episodes of acute inflammation may prompt the formation of extraneous fibrous tissue, which is largely responsible for establishing a permanent or chronic condition.
Compression Neuropathy
A second hypothesis points to a neurogenic origin for CTDs, targeting multilevel compression neuropathy as the primary etiology. The mechanism by which acute compression affects the peripheral nerve is not completely understood, but is thought to involve both ischemic and mechanical factors. Nerve entrapment syndromes result from repeated or sustained compression of a peripheral nerve between ligaments or constricted anatomic structures. In addition to external compression, nerve entrapment may also be caused, aggravated, or precipitated by posture (Mackinnon & Novak, 1994).
It is proposed that the hypoxia from compression of the blood supply by muscles and tendons leads to problems with the nerves (Mackinnon & Novak, 1994; Ranney, 1993). With compression of a nerve, there is obstruction of venous return.
The increased venous pressure results in slowed circulation in the nerve complex and dilatation of the small vessels and capillaries within the nerve segment. There is edema, proliferation of fibroblasts, and scarring in the nerve segment, which compress the nerve (Childre & Winzeler, 1995).
Critics of this hypothesis raise concerns regarding lack of an explanation for the etiology of the muscular component seen with CTDs.
Neuropathic Compression, Myofascial Pain, and Muscle Imbalance
The third hypothesis is an integration of the existing hypotheses relating to neuropathic compression and myofascial pain, with the addition of muscle imbalance (Higgs & Mackinnon, 1995; Mackinnon & Novak, 1994). The basic tenet of this hypothesis is that prolonged and frequent assumption of abnormal postures, positions, or movements of the head, neck, and upper extremity has two major influences on the body. First, specific extremity positions cause increased pressure around certain nerves and, if encountered frequently and for long periods, will eventually result in chronic nerve compression. Both chronic tension and direct mechanical compression decrease blood flow to the nerve, producing fibrosis in and around the nerve; this in turn inhibits full excursion during normal extremity movement. In addition, placing the nerve on stretch will cause increased tension within the nerve, provoking symptoms from both sensory and motor fibers. Nerve compression at one point along the nerve may cause both distal and proximal sites to be less tolerant of the effects of compression. Chronic nerve compression is thought to be progressive unless specific interventions are initiated.
Second, abnormal postures can result in a set of muscles being maintained and used in shortened positions, which can lead to muscle imbalance. Underuse of some muscles subsequently leads to a weak set of muscles; this ultimately results in a compensatory overuse of a second set of muscles, and a cycle of muscle imbalance will be established. The muscles maintained and used in shortened positions become tight and painful, especially when stretched. Some muscles secondarily compress neurovascular structures when in a tightened position. It is this self-perpetuating cycle of tight muscles becoming tighter and weak muscles becoming weaker that explains why rest alone will not relieve all the symptoms of CTDs (Mackinnon & Novak, 1994).
The second perspective on CTDs is denial of their very existence. Proponents of this explanation (Ferguson, 1987; Hadler, 1990; Lam, 1995; Ranney, 1993; Weiland, 1996) believe that CTDs are not primarily physiological in nature but rather are based on psychosocial and sociopolitical factors. As such, they suggest that CTDs are a reflection of modern society without clearly identifiable pathology. The difficulty in the objective determination of the work relatedness of CTDs and the frequently associated financial compensation factor add to the difficulty of accepting CTD as a diagnosis. For the most part, supporters of this perspective recommend that syndromic titles such as CTD be abandoned in favor of clearly definable and diagnosable entities with a known histological appearance and etiology.
Although there are different perspectives on the causative factors of CTDs, all but the psychosocial theory accept that both biomechanical and physiological factors are involved. Most would agree that repeated or sustained exertion, in combination with certain postures, causes, precipitates, or aggravates chronic upper-extremity tendon and nerve disorders. Additional contributing factors may include the force used in performing movements, increased muscle tension associated with mental stress, and factors external to the person (e.g., faulty workstation, equipment, task design, and maintenance of equipment).
 EPIDEMIOLOGY
EPIDEMIOLOGY
The overall incidence and prevalence of CTDs, as well as the distribution and determinants, are difficult to ascertain. No definition of CTD has been agreed on. Use of such a broad term does not specify the exact anatomical or pathological involvement. This creates difficulty when the provider is pressed to determine an etiology and recommend a treatment plan. To complicate matters, several terms are used synonymously with CTD, including repetitive strain injuries, overuse syndromes, work-related musculoskeletal disorders, and repetitive motion injuries. For consistency, the term CTD is used throughout this chapter.
In addition to variations in diagnostic terminology and criteria, differences in attitudes of health care providers about reporting CTDs contribute to the inadequacies of the epidemiologic data. Many of the published data involve occupation-related CTDs, but occurrence can also be related to intrinsic factors of the person and recreational activities. The epidemiologic literature also separates clinically well-defined disorders such as tendinopathy, tendinosis, and carpal tunnel syndrome from the nonspecific diagnoses referred to as CTDs (Maffulli et al., 1998).
The incidence rates for CTDs in the U.S. workplace was 38 cases per 10,000 full-time workers in 2012, and CTDs accounted for 34% of all workplace injuries requiring time away from work (U.S. Department of Labor, 2013). Given the inconsistencies in reporting and the occurrence of CTDs that are not work related, these data are useful for interpreting trends and identifying high-risk industries.
The prevalence of upper-extremity CTDs depends on the occupation studied, the risk factors present, and the specific body part studied. The prevalence of CTDs may be related to ergonomic factors. The following six occupations accounted for more than 25% of reported CTDs: laborers and freight, stock, and material movers; nursing assistants; janitors and cleaners; heavy and tractor–trailer truck drivers; registered nurses; and maintenance and repair workers (U.S. Department of Labor, 2013). However, the reporting of CTDs is inconsistent, and there may be other industries with high occurrences.
Many factors, both occupational and nonoccupational, have been reported to cause, precipitate, or aggravate conditions categorized as CTDs. The specific contribution of occupational and nonoccupational factors has not been determined. Occupational factors include repetitive motion, forceful exertions, mechanical insult, sustained and awkward postures, and frequent exposure to low-frequency vibrations and cold temperatures, as well as lack of training and experience, poor workstation design, and inappropriate tools. The association of job demand and workplace psychosocial factors should also be considered. Factors that have the most consistent association include high workloads, perceived time pressure, work pressure, high workload variability, poor work content, and monotonous work (Hales & Bernard, 1996). Examples of nonoccupational factors thought to contribute to CTDs include congenital defects, use of birth-control pills, pregnancy, chronic disease, recreational factors, and use of the antibiotic fluoroquinolone (Armstrong et al., 1987a; Hebert, 1993; Kroemer, 1992; Putz-Anderson, 1988; Stephenson, Wu, Cortes, & Rochon, 2013). Few epidemiologic data are available to determine how age relates to CTDs; the influence of age and gender on the susceptibility to CTDs is controversial.
 DIAGNOSTIC CRITERIA
DIAGNOSTIC CRITERIA
CTDs include a variety of familiar clinical entities, such as tenosynovitis, tendinosis/tendinitis, epicondylitis, trigger finger, and carpal tunnel syndrome, as well as vague complaints of pain. Assessment and management of these familiar conditions are better understood in contrast to the more challenging and often perplexing disorders associated with compressive neuropathies and nonspecific complaints of pain. The major problem in assessing and managing CTDs occurs when paresthesias are accompanied by ambiguous complaints, such as pain in the entire upper extremity, neck, back, subscapular area, and shoulder (Higgs & Mackinnon, 1995).
Diagnosis is based on a careful history, physical examination, and the exclusion of other well-described entities. There are no specific pathological or radiological features to support a diagnosis of CTD, and definitive diagnostic criteria have not been established. There is, however, a distinct history that is suggestive of CTD:
 Symptoms appear gradually.
Symptoms appear gradually.
 Symptoms worsen over weeks, months, or even years.
Symptoms worsen over weeks, months, or even years.
 Initially, the symptoms may subside with rest, but as time goes on, symptoms worsen and are no longer relieved with rest (Armstrong et al., 1987a; Higgs et al., 1993; Mackinnon & Novak, 1994; Putz-Anderson, 1988).
Initially, the symptoms may subside with rest, but as time goes on, symptoms worsen and are no longer relieved with rest (Armstrong et al., 1987a; Higgs et al., 1993; Mackinnon & Novak, 1994; Putz-Anderson, 1988).
Subjective and objective signs and symptoms consistent with the diagnosis of CTD include:
 Soft-tissue swelling and muscle atrophy
Soft-tissue swelling and muscle atrophy
 Pain and tenderness
Pain and tenderness
 Decreased range of motion
Decreased range of motion
 Loss of grip strength
Loss of grip strength
 Reproduction of paresthesia and numbness by provocative maneuvers
Reproduction of paresthesia and numbness by provocative maneuvers
 Decline in work performance
Decline in work performance
 Functional impairment
Functional impairment
 Fatigue
Fatigue
 Sensory changes (Browne, Nolan, & Faithfull, 1984; Isernhagen, 1992; Millender, Tromanhauser, & Gaynor, 1996; Putz-Anderson, 1988).
Sensory changes (Browne, Nolan, & Faithfull, 1984; Isernhagen, 1992; Millender, Tromanhauser, & Gaynor, 1996; Putz-Anderson, 1988).
One of the difficulties in evaluating these disorders is trying to establish a diagnosis in the absence of objective physical findings or confirmatory diagnostic imaging or laboratory data. For the most part, authorities advocate using the diagnostic label that is most specific to the presenting condition (e.g., de Quervain’s tenosynovitis), reserving CTD for situations that do not meet the criteria of other known clinical entities (Millender et al., 1996) but contain the signs and symptoms described here.
 HISTORY AND PHYSICAL EXAMINATION
HISTORY AND PHYSICAL EXAMINATION
Early diagnosis and prompt treatment require adequate assessment. Key aspects of the history and physical examination are delineated in Table 41.1.
Physical Examination of the Upper Extremity |
EXAMINATION | FINDINGS |
Inspection | |
Note skin turgor, color, swelling, wrinkles, scars, atrophy, contractures, masses, obvious deformity, symmetry, arm length discrepancies, and posture |
|
Palpation | |
Assess skin temperature, moisture, and areas of tenderness |
|
Range of Motion | |
Passive, active, resisted Assess flexion, extension, hyperextension, opposition, abduction, adduction, supination, pronation, ulnar deviation, radial deviation, and internal and external rotation. Compare right and left extremities. Determine joint stability and presence of crepitation. Assess for muscle tenderness by assessing pain with resisted activity. |
|
Motor Strength | |
Conduct gross muscle strength testing with right to left comparison. |
|
Measurement of grip and pinch strength to establish a baseline and subsequently as an indicator of improving or worsening condition. Use a grip dynamometer and a pinch dynamometer to make three successive determinations and calculate percentage relative to pretreatment value, if available, as well as to value from contralateral hand. |
|
Sensibility | |
Assess radial, median, and ulnar nerve distribution. Standard sensory testing includes two-point discrimination and threshold testing of vibration and pressure (Table 41.2). |
|
Vascular Status | |
Assess ulnar, radial, and brachial pulse as appropriate. See Figure 41.9 for Allen test to determine patency of the arteries supplying the hand. |
|
CTD, cumulative trauma disorder.
Source: American Society for Surgery of the Hand (1990); Higgs and Mackinnon (1995); Messer and Bankers (1995); Ranney (1993); Rempel, Harrison, and Barnhard (1992).
Focused History
 Elicit general information: age; hand dominance; past medical, surgical, and injury history; and current medications.
Elicit general information: age; hand dominance; past medical, surgical, and injury history; and current medications.
 Identify usual activity level and note any current impairment (occupational, recreational, exercise routine, and activities of daily living).
Identify usual activity level and note any current impairment (occupational, recreational, exercise routine, and activities of daily living).
 Elicit the location, duration, frequency, intensity, and onset of discomfort (pain, swelling, aching, tingling, numbness, burning, or stiffness).
Elicit the location, duration, frequency, intensity, and onset of discomfort (pain, swelling, aching, tingling, numbness, burning, or stiffness).
 Determine relieving and exacerbating factors.
Determine relieving and exacerbating factors.
 Assess the impact the condition is having on the person’s life (activities of daily living; family relationships; economic, work, and social situations).
Assess the impact the condition is having on the person’s life (activities of daily living; family relationships; economic, work, and social situations).
 Identify existing stressors and current coping techniques.
Identify existing stressors and current coping techniques.
 Elicit sleep patterns and sleep positions.
Elicit sleep patterns and sleep positions.
If the condition appears to be related to occupational activities, include the following:
 Exposure to occupational risk factors (high force, repetitive motions, awkward or sustained positioning, local mechanical contact stress, exposure to low-frequency vibration and cold temperatures)
Exposure to occupational risk factors (high force, repetitive motions, awkward or sustained positioning, local mechanical contact stress, exposure to low-frequency vibration and cold temperatures)
 Length of time in current occupation
Length of time in current occupation
 Previous occupations with similar risk factors
Previous occupations with similar risk factors
 Relation of symptoms to work; duration of work at a particular task before the onset of symptoms
Relation of symptoms to work; duration of work at a particular task before the onset of symptoms
Physical Examination
Examination of the upper extremity includes inspection, palpation, and evaluation of range of motion, motor strength, sensibility, neurological function, and vascular status. Tables 41.1 and 41.2 outline key aspects of the examination and interpretation of common findings. Provocative tests to elicit specific findings are illustrated in Figures 41.6 to 41.10.
 DIAGNOSTIC STUDIES
DIAGNOSTIC STUDIES
Diagnostic imaging should be ordered based on the history and thorough physical examination results. MRI or ultrasonography can be used to identify changes in tendon appearance, identify microscopic tears, and determine if there is involvement of other structures possibly contributing to tendinosis. Because soft tissues are involved, radiographs in general are not necessary unless accurate location of the pain is uncertain or if there is a history of trauma. Electromyography (EMG) is useful for diagnosing peripheral nerve entrapment syndromes, such as carpal tunnel (Cherniak, Moalli, & Viscolli, 1996).
Two-point discrimination: A subjective measure of cutaneous sensibility. With a blunt instrument, gently apply pressure, beginning at 6 mm between the two points. Increase or decrease to determine the distance at which the person can distinguish two points from one. Applied pressure should not blanch the skin. Responses are recorded with specific measurements or as normal, <6 mm; fair, 6–10 mm; poor, 11–15 mm; protective, one point perceived; and anesthetic, no point perceived (American Society for Surgery of the Hand, 1990).
Tuning fork: A subjective measure of vibration. It can be used on each digit to determine a baseline and change in perception of vibration.
Semmes-Weinstin monofilament test: An objective measure of cutaneous sensibility involving light touch to deep pressure testing with monofilaments of increasing force. Standardized nylon filaments of specific length and diameter are applied three times to the same spot to ascertain perception. The filament design controls the force and velocity of application. The standardized testing instrument has 20 filaments, each of a different size. This test can be used serially to determine changes in neural status or as an initial evaluation of touch threshold in areas of normal sensibility and areas of diminution. Responses are recorded as normal, diminished light touch, diminished protective sensation, loss of protective sensation, and untestable based on responses to application of the monofilaments (Bell-Krotoski, 1995). This test is often conducted by an occupational therapist.
FIGURE 41.6
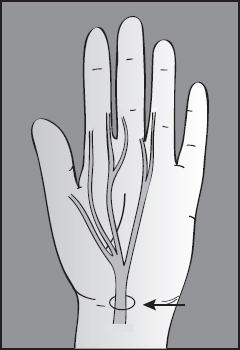
Tinel’s test consists of a gentle tapping over the nerve. A positive response is pain or paresthesia in the distribution of the nerve. A positive response is indicative of compression or entrapment of the nerve.
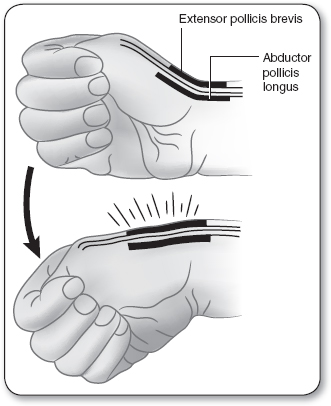
FIGURE 41.7
Finkelstein’s test is ulnar deviation of the hand with the thumb flexed against the palm and the fingers flexed over the thumb. A positive response is pain at the radial styloid due to stretching of the abductor pollicis longus and extensor pollicis brevis. A positive response is indicative of de Quervain’s tenosynovitis.
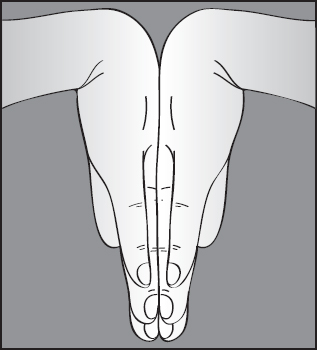
FIGURE 41.8
Phalen’s sign involves flexion of both wrists at 90° with the dorsal aspect of the hands held in apposition for 60 seconds. A positive response is pain or anesthesia in at least one finger innervated by the median nerve. A positive response is suggestive of entrapment of the median nerve.
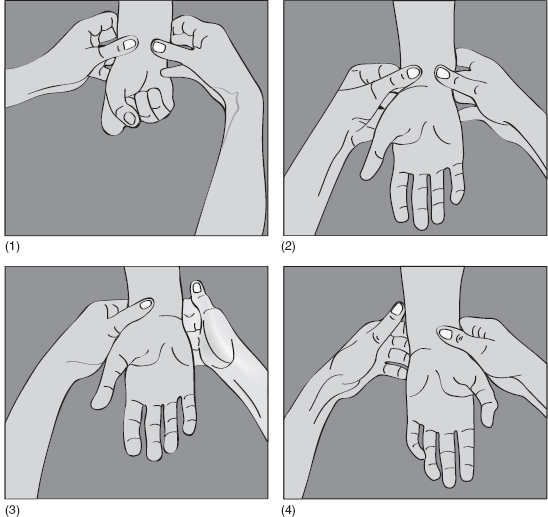
FIGURE 41.9
The Allen test is used to determine patency of the arteries supplying the hand. It is done as follows: (1) Compress the radial and ulnar arteries at the wrist; (2) have the person make a fist, open and close it several times to exsanguinate the hand, and then open the hand again into a relaxed position, avoiding hyperextension; (3) release the radial artery only. If the entire hand pinks up in color, the radial artery is patent with good collateral flow into the ulnar artery system. Repeat the first two steps. (4) Release the ulnar artery only. If the entire hand pinks up in color, the ulnar artery is patent with good collateral flow into the radial artery system.
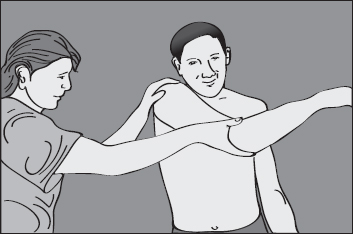
FIGURE 41.10
A positive impingement sign is pain at 90° with resisted abduction and normal strength or forcibly forward-elevating the affected arm while stabilizing the scapula; pinching of the supraspinatus tendon between the humeral head and the anterior-inferior aspect of the acromion.
Source: Neer (1983).
 TREATMENT OPTIONS, EXPECTED OUTCOMES, AND COMPREHENSIVE MANAGEMENT
TREATMENT OPTIONS, EXPECTED OUTCOMES, AND COMPREHENSIVE MANAGEMENT
Primary Prevention
Primary prevention of CTDs requires both health promotion and health protection interventions. Health promotion interventions have as a goal the achievement and maintenance of strong upper-extremity muscles. Health protection interventions focus on the avoidance of known causative factors. The acquisition of a CTD occurs over time, and thus prevention is an ongoing process.
 HEALTH PROMOTION AND SPECIFIC PROTECTION
HEALTH PROMOTION AND SPECIFIC PROTECTION
General recommendations for health promotion—a healthy diet, regular aerobic and strengthening exercises, and achievement and maintenance of ideal body weight—are all considered beneficial for the prevention of CTDs (Nathan, Keniston, Meadows, & Lockwood, 1995). An awareness of risk and nonrisk positions for nerve compression and muscle imbalance (Mackinnon & Novak, 1995) would also be helpful. The prevention and the resolution of CTDs require an all-encompassing approach: CTDs and cumulative life experiences cannot be viewed in isolation from each other.
Most of the CTD prevention literature is related to the occupational environment. The same principles, however, apply regardless of the setting. Recognition of the potential for injury is the first step, followed by specific strategies (outlined later) to minimize the risks associated with both occupational and recreational activities.
Systematic analysis of work sites to identify ergonomic hazards is an aspect of primary prevention for occupational risk factors. A checklist can be used to determine the presence of ergonomic risk factors associated with the development of upper-extremity CTDs (Keyserling, Stetson, Silverstein, & Brouwer, 1992). The checklist should address the presence of and duration of exposure to the following stressors: repetitiveness, local mechanical contact stress, forceful manual exertions, awkward upper-extremity posture, vibration, cold temperature, and hand-tool use. It should be regarded as an initial screening tool used to increase awareness of potential risk factors.
Hebert (1993) suggested the five “Es” of injury elimination: engineering, education, exposure reduction, exercise, and enforcement. Engineering refers to the correction of faulty design in work processes, tools, materials, and procedures to avoid stressful motions or postures. Exposure reduction refers to job rotation frequent enough to provide effective interruption of stressful job demands and to provide a variety of movements and posture loads. Education refers to the training of managers, supervisors, and workers so that they might be motivated to adopt CTD avoidance behaviors. Exercise refers to stretching musculoskeletal tissues frequently to reduce fatigue and restore circulation. Enforcement implies a structure of expectations and responsibility for all involved to carry out their CTD-prevention roles. As isolated initiatives, each action has a limited effect. However, when all are applied in a coordinated and controlled manner, successful outcomes can be achieved.
The role of the primary care provider is to identify persons at risk and encourage an adequate conditioning program, with a focus on the upper extremity. Furthermore, provision of information specific to certain postures and motions that are thought to be causative factors may be beneficial. Tables 41.3 to 41.5 give specific examples. Persons whose job activities include rapid repetitive movements, forceful movements, static muscle loading, inappropriate body postures, vibrations, and cold should be advised to discuss ergonomic issues with their supervisor and the occupational health provider at their place of work (NIOSH, 1997). Preventing a problem is much easier than resolving one;
 Repetitive motion
Repetitive motion
 Prolonged or repeated forceful exertion
Prolonged or repeated forceful exertion
 Sustained or awkward positioning
Sustained or awkward positioning
 Exposure to low-frequency vibration
Exposure to low-frequency vibration
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree