Continuous Brachial Plexus Nerve Block
A. Continuous Interscalene Block
Stephen M. Klein
Charles Pham Dang
Terese T. Horlocker
Andre P. Boezaart
1. Classic Approach
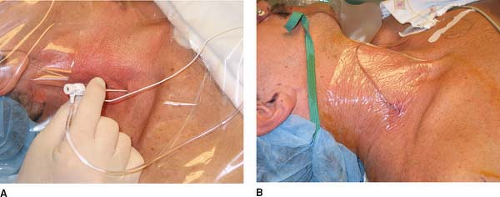
The fingers are gently slid posteriorly and the first bandlike muscle is the anterior scalene muscle. The next muscle is the middle scalene muscle. The interscalene groove is marked. The site of needle introduction is the intersection between the horizontal line drawn at the level of the cricothyroid membrane and the interscalene groove. The insulated Tuohy needle connected to a nerve stimulator (1.5 mA, 2 Hz, 0.1 ms) with the bevel oriented to the axilla is introduced through the skin and directed medially, slightly caudad, and posterior (Fig. 26-1A) at approximately 30° to the skin. As the needle punctures the fascia, there is a subtle “click” and sudden motor movement, which helps confirm proper placement. The position of the needle is adjusted to produce a motor response distal to the shoulder, which is maintained with a current less than 0.5 mA. After negative aspiration for blood, the local anesthetic is slowly injected with repeated aspiration for blood. Maintaining the introducer-insulated needle in the same position, the catheter is threaded 3 to 5 cm beyond the needle tip. The introducer needle is removed, and the catheter is secured in place with Steri-Strip (3M, St. Paul, MN) and covered with a transparent dressing (Fig. 26-1B).
To increase operator steadiness, the bed may be raised to chest height with the operator’s forearms resting on the bed.
The introducer needle should be manipulated cautiously.
The interscalene groove is subtle and narrow. It should not be confused with the groove between the SCM muscle and the anterior scalene muscle.
A pre-hole with a sharp 18-gauge needle helps reduce pressure on the neck while introducing the dull insulated Tuohy needle.
Avoid aggressive searching with the 18-gauge needle. If necessary, find the plexus first with a 22-gauge insulated needle.
Seek a stimulus distal to the shoulder with the lowest achievable current (<0.5 mA).
If a deltoid stimulus is obtained, this may be acceptable, but make sure it is not pectoralis or suprascapular stimulation, since these nerves usually have already separated from the main plexus.
Phrenic stimulation (diaphragm contraction) indicates that the needle is >1 cm too far anterior.
A pectoralis muscle stimulation indicates that the needle is slightly (<0.5 cm) anterior.
A suprascapular muscle (posterior shoulder) stimulation suggests that the needle is slightly (<0.5 cm) posterior.
If subtle redirection produces constant anterior/posterior stimulus but not arm movement, consider moving the entry point caudad.
There is slight resistance as the catheter passes the needle tip, but afterward it should pass easily. After 3 to 4 cm in the sheath, resistance is typically encountered. Gradually withdraw the needle and advance the catheter another 3 to 4 cm in the subcutaneous tissue. This tunnels the catheter and helps secure it.
Careful attention should be paid to securing the catheter. Subcutaneous tunneling is helpful.
Suggested Readings
Borgeat A, Tewes E, Biasca N, et al. Patient-controlled interscalene analgesia with ropivacaine after major shoulder surgery: PCIA vs PCA. Br J Anaesth 1998;81:603–605.
Lierz P, Schroegendorfer K, Choi S, et al. Continuous blockade of both brachial plexus with ropivacaine in phantom pain. Pain 1998;78:135–137.
Singelyn F, Seguy S, Gouverneur J. Interscalene brachial plexus analgesia after open shoulder surgery: continuous versus patient-controlled infusion. Anesth Analg 1999;89:1216–1220.
Tuominen M, Haasio J, Hekali R, et al. Continuous interscalene brachial plexus block: clinical efficacy, technical problems and bupivacaine plasma concentrations. Acta Anaesthesiol Scand 1989;33:84–88.
Winnie AP. Plexus anesthesia: perivascular techniques of brachial plexus block. Philadelphia: WB Saunders Co, 1993.
2. Intersternocleidomastoid Approach
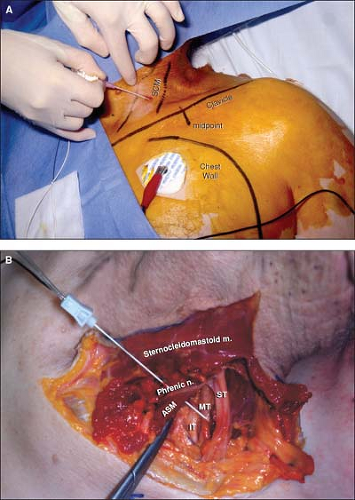
midclavicle. This initial orientation leads to stimulation of the lateral border of the superior trunk (Fig. 26-2B) which is lateral to the rest of the brachial plexus and produces glenohumeral coaptation and contraction of the supraspinatus muscle. From this initial position lateral to the brachial plexus, the needle can be slightly walked medially and inferiorly to seek for stimulation of the middle trunk. The following motor responses help identify which part of the brachial plexus is being stimulated:
The superior trunk frontally—contraction of the biceps brachii muscle with elbow flexion.
The superior trunk medially—contraction of the deltoid with abduction of the arm.
The middle trunk—contraction of the triceps and elbow extension.
The inferior trunk frontally—contraction of the pectoralis major muscle, ulnar inclination of the wrist, and flexion of the fourth and fifth fingers.
After appropriate positioning of the needle allowing the same motor response to be maintained with a current less than 0.5 to 0.6 mA, and after negative aspiration for blood, the local anesthetic solution is injected slowly, 5 mL at a time, with aspiration in between.
The catheter is introduced 2 to 3 cm beyond the tip of the introducer needle. The introducing cannula is removed, and the catheter is secured in place with Steri-Strip and covered with a transparent dressing.
In the intersternocleidomastoid block, the brachial plexus can be reached at the level of the superior, middle, or inferior trunk when the needle is directed into the supraclavicular area. The brachial plexus will be contacted at a depth varying from 3 to 8 cm, depending on needle direction and the size of the patient.
Catheter insertion seems to be easier following stimulation of the middle trunk than following stimulation of the superior trunk.
This approach minimizes the risk for inadvertent spinal injection of anesthetics and pleural puncture.
This approach does not require tunneling the catheter because it approaches the brachial plexus from a distance.
The rotation of the neck should be moderate to avoid distortion of the anatomic landmarks, particularly in patients with long necks.
The presence of fat may obscure the SCM triangle. Asking the patient to elevate the head and breathe deeply allows easier palpation of the muscles.
Compressing the SCM triangle above the clavicle with the forefinger helps to determine the puncture site, raise the clavicular head of the SCM, and facilitate the passage of the needle behind the clavicular head.
To prevent misdirection of the needle, which may result in pleural puncture, it is recommended to mark the superior border of the chest wall, and keep the needle lateral and away from the dome of the pleura.
To avoid a puncture of the internal jugular vein, especially during the local infiltration, the needle should be directed in the same direction as described in the intersternocleidomastoid technique. Such an infiltration provides more comfort during insertion of the introducer needle.
The introducer needle may transmit an arterial pulsation, indicating proximity to the subclavian artery. In this case, the needle is withdrawn and directed slightly more posterior to prevent puncture of the subclavian artery.
To minimize the risk for associated diaphragmatic palsy, the tip of the catheter should be placed in an infraclavicular position.
Movements of the abdomen (contraction of the diaphragm) can be seen in response to stimulation of the phrenic nerve. Since the phrenic nerve is anterior to the scalene muscle and medial to the brachial plexus, these stimulations require withdrawal and redirection of the needle.
The position of the catheter can be controlled radiologically before starting the infusion. The use of a stimulating catheter may also increase the likelihood of an appropriate placement.
Complications of these techniques include the risk for internal jugular puncture (during local anesthesia of the region) and subclavian artery puncture (in the case of misdirection of the needle), pleural puncture (misdirection of the needle), associated diaphragmatic palsy, Horner syndrome (uncomfortable for the patient), and recurrent laryngeal nerve palsy due to catheter misplacement.
Suggested Readings
Carter C, Mayfield JB. Evaluation of a new supraclavicular brachial plexus catheter technique for shoulder surgery anesthesia and analgesia. Anesthesiology 2000;93:A849.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree