CHAPTER 15
Contact Lens Complications
Presentation
A patient who wears hard, impermeable, or rigid gas permeable contact lenses comes to the emergency department in the early morning complaining of severe eye pain after he has left his lenses in for longer than the recommended time period. Extended-wear soft contact lenses can cause a similar syndrome when worn for days or weeks and have become contaminated with bacteria and/or irritants. The patient may not be able to open his eyes for examination because of pain and blepharospasm. He may have obvious corneal injury, with signs of iritis and conjunctivitis, or may have no findings visible without fluorescein staining.
What To Do:
 Instill topical anesthetic drops such as proparacaine (Alcaine, Ophthaine) to provide comfort for examination.
Instill topical anesthetic drops such as proparacaine (Alcaine, Ophthaine) to provide comfort for examination.
 Perform a complete eye examination, including best-corrected visual acuity, assessment of pupil reflexes, examination with funduscopy, and inspection of conjunctival sacs. Use a slit lamp if available.
Perform a complete eye examination, including best-corrected visual acuity, assessment of pupil reflexes, examination with funduscopy, and inspection of conjunctival sacs. Use a slit lamp if available.
 With a bright light examination, note whether there are any hazy areas or ulcerations on the cornea.
With a bright light examination, note whether there are any hazy areas or ulcerations on the cornea.
 Instill fluorescein dye (use a single-dose dropper or wet a dye-impregnated paper strip and touch it to the tear pool in the lower conjunctival sac), have the patient blink, and examine the eye under cobalt blue or ultraviolet light, looking for the green fluorescence of dye bound to dead or areas of absent corneal epithelium. Rinse out the dye afterward.
Instill fluorescein dye (use a single-dose dropper or wet a dye-impregnated paper strip and touch it to the tear pool in the lower conjunctival sac), have the patient blink, and examine the eye under cobalt blue or ultraviolet light, looking for the green fluorescence of dye bound to dead or areas of absent corneal epithelium. Rinse out the dye afterward.
 When a corneal defect is visualized, sketch the area of corneal injury on the patient record.
When a corneal defect is visualized, sketch the area of corneal injury on the patient record.
 When the symptoms consist of a mild burning, a foreign body sensation, and/or dryness, and examination with fluorescein staining shows mild punctate uptake (superficial punctate keratitis; Figure 15-1), treatment consists of discontinuation of lens use and the instillation of fluoroquinolone drops—ciprofloxacin 0.3% (Ciloxan), 1 to 2 drops q1-6h (use more frequently for the first 2 to 3 days). Prescribe analgesics (e.g., naproxen, ibuprofen, oxycodone) as needed, and administer the first dose if appropriate.
When the symptoms consist of a mild burning, a foreign body sensation, and/or dryness, and examination with fluorescein staining shows mild punctate uptake (superficial punctate keratitis; Figure 15-1), treatment consists of discontinuation of lens use and the instillation of fluoroquinolone drops—ciprofloxacin 0.3% (Ciloxan), 1 to 2 drops q1-6h (use more frequently for the first 2 to 3 days). Prescribe analgesics (e.g., naproxen, ibuprofen, oxycodone) as needed, and administer the first dose if appropriate.
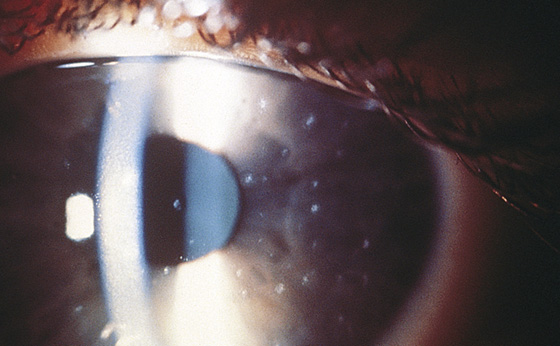
Figure 15-1 General appearance of superficial punctate keratitis under slit-lamp examination. (Adapted from Yanoff M, Duker JS: Ophthalmology, ed 2. St Louis, 2004, Mosby.)
 Instruct the patient to avoid wearing his lenses until cleared by the ophthalmologist and to seek ophthalmologic follow-up within 1 day.
Instruct the patient to avoid wearing his lenses until cleared by the ophthalmologist and to seek ophthalmologic follow-up within 1 day.
 Contact lens–induced acute red eye (CLARE) can occur with extended-wear contact lenses and has been defined as an acute onset of a red eye associated with corneal infiltrates. Typically, symptoms of ocular discomfort, foreign-body sensation, and redness are noted on awakening. These findings are usually unilateral, and, on examination, conjunctival injection, mild chemosis, and peripheral corneal infiltrates are seen. The corneal epithelium overlying the infiltrates may be intact, or a mild punctate keratopathy may be present. Treatment consists of discontinuation of contact lens wearing until complete resolution has occurred. There is apparently no medical therapy indicated for this condition, but it would be considered reasonable and prudent to initiate the same treatment as that provided for superficial punctate keratitis.
Contact lens–induced acute red eye (CLARE) can occur with extended-wear contact lenses and has been defined as an acute onset of a red eye associated with corneal infiltrates. Typically, symptoms of ocular discomfort, foreign-body sensation, and redness are noted on awakening. These findings are usually unilateral, and, on examination, conjunctival injection, mild chemosis, and peripheral corneal infiltrates are seen. The corneal epithelium overlying the infiltrates may be intact, or a mild punctate keratopathy may be present. Treatment consists of discontinuation of contact lens wearing until complete resolution has occurred. There is apparently no medical therapy indicated for this condition, but it would be considered reasonable and prudent to initiate the same treatment as that provided for superficial punctate keratitis.
 When patients complain of severe pain, irritation, photophobia, and tearing associated with infiltrates and epithelial defects, they are at high risk for the most serious complication of contact lens wear (microbial keratitis; Figure 15-2). The most commonly cultured organisms are gram negative, particularly Pseudomonas aeruginosa. The more severe the symptoms are, the larger the corneal epithelial defect (>1.5 mm), and the more central its location, the greater the morbidity is likely to be, with resultant permanent loss of vision. These patients demand prompt ophthalmologic consultation, along with the initiation of treatment with the most potent topical antibiotics (i.e., a combination of either fortified cefazolin or vancomycin and fortified tobramycin or gentamicin). Suspected microbial ulcers must be scraped and cultured and a Gram stain performed. Contact lens care solutions and the contact lens case should also be cultured along with the ulcer if possible. Patients with less severe cases can be treated with moxifloxacin (Vigamox), 0.5% solution, 3 mL, 1 to 2 drops every 2 hours when awake or gatifloxacin (Zymar), 0.3% solution, 5 mL, 1 to 2 drops every 2 hours when awake then taper to 1 to 2 drops qid. Ophthalmologic consultation with next-day follow-up is still very important.
When patients complain of severe pain, irritation, photophobia, and tearing associated with infiltrates and epithelial defects, they are at high risk for the most serious complication of contact lens wear (microbial keratitis; Figure 15-2). The most commonly cultured organisms are gram negative, particularly Pseudomonas aeruginosa. The more severe the symptoms are, the larger the corneal epithelial defect (>1.5 mm), and the more central its location, the greater the morbidity is likely to be, with resultant permanent loss of vision. These patients demand prompt ophthalmologic consultation, along with the initiation of treatment with the most potent topical antibiotics (i.e., a combination of either fortified cefazolin or vancomycin and fortified tobramycin or gentamicin). Suspected microbial ulcers must be scraped and cultured and a Gram stain performed. Contact lens care solutions and the contact lens case should also be cultured along with the ulcer if possible. Patients with less severe cases can be treated with moxifloxacin (Vigamox), 0.5% solution, 3 mL, 1 to 2 drops every 2 hours when awake or gatifloxacin (Zymar), 0.3% solution, 5 mL, 1 to 2 drops every 2 hours when awake then taper to 1 to 2 drops qid. Ophthalmologic consultation with next-day follow-up is still very important.
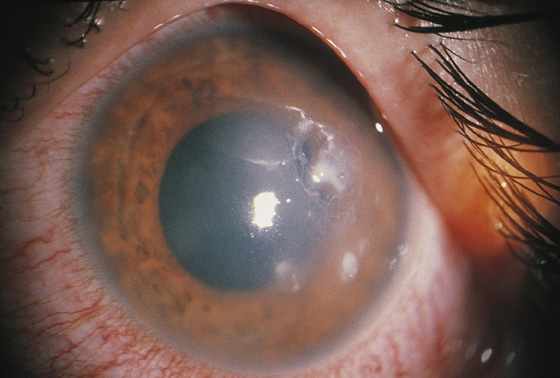
Figure 15-2 Microbial keratitis. Intraepithelial infiltration of the cornea by Pseudomonas organisms in a hydrophilic contact lens wearer. (Adapted from Yanoff M, Duker JS: Ophthalmology, ed 2. St Louis, 2004, Mosby.)
 In the presence of minimal signs of inflammation in a patient with significant pain that is out of proportion to the findings, consider the possibility of Acanthamoeba keratitis. This form of infection from overwearing of soft lenses can damage the eye rapidly and may require excision and hospitalization.
In the presence of minimal signs of inflammation in a patient with significant pain that is out of proportion to the findings, consider the possibility of Acanthamoeba keratitis. This form of infection from overwearing of soft lenses can damage the eye rapidly and may require excision and hospitalization.
What Not To Do:
 Do not discharge a patient with topical anesthetic ophthalmic drops for continued administration; they potentiate serious injury.
Do not discharge a patient with topical anesthetic ophthalmic drops for continued administration; they potentiate serious injury.
 Do not let a patient reuse contaminated or infected lenses.
Do not let a patient reuse contaminated or infected lenses.
 Do not patch eyes damaged by contact lens abrasions or early ulcerative keratitis.
Do not patch eyes damaged by contact lens abrasions or early ulcerative keratitis.
 Do not prescribe antibiotic ointments that do not provide prophylaxis against Pseudomonas organisms (e.g., erythromycin and sulfas).
Do not prescribe antibiotic ointments that do not provide prophylaxis against Pseudomonas organisms (e.g., erythromycin and sulfas).
 Do not use drops or ointments containing steroids without an ophthalmologist’s recommendation.
Do not use drops or ointments containing steroids without an ophthalmologist’s recommendation.
Discussion
Hard or rigid gas-permeable contact lenses and extended-wear soft lenses left in place too long deprive the avascular corneal epithelium of oxygen and nutrients that are normally provided by the tear film. This produces diffuse ischemia, which can cause an increase in bacterial binding to the corneal epithelium. Soft lenses can absorb chemical irritants, allergens, bacteria, and amoebas if they soak in contaminated cleaning solution.
Patient-related factors—such as alteration of the recommended wearing or replacement schedules and noncompliance with recommended contact lens care regimens for economic reasons, convenience, or in error—contribute to contact lens–related complications.
Studies have shown that the major risk for infection with conventional contact lenses is overnight wear. The risk for infection is still 5 times greater with extended-wear contact lenses compared with that for daily wear. Initial results of studies looking at silicone hydrogel contact lenses (Pure Vision) worn for extended periods are encouraging in that they appear to result in a lower incidence of microbial keratitis than seen with the standard extended-wear lenses.
There are millions of contact lens wearers in the United States. Adverse reactions range from minor transient irritation to corneal ulceration and infection that may result in permanent loss of vision caused by corneal scarring. Pseudomonas organism infection is most commonly associated with contact lens–related microbial keratitis. Thus the management of these cases should differ from the routine care of mechanical corneal abrasions that are not caused by contact lens wear. Occlusive patching and corticosteroid medications favor bacterial growth and are, therefore, not generally recommended for initial treatment in the setting of contact lens use.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


