Common Ophthalmic Medications
Kimberly Schertzer
This chapter provides an overview of medications used to diagnose and treat common ocular conditions.
DIAGNOSTIC MEDICATIONS
Stains
These topical solutions reveal areas of corneal and conjunctival epithelial disruption.
Fluorescein stains are by far the most commonly used stains in the emergency department (ED). These stains highlight defective epithelium within the cornea and conjunctiva, with defective areas enhancing under cobalt blue light after staining. Single-use, sterile paper strips are preferred instead of the 2% solutions for convenience and concern about contamination of multiuse containers. Evaluation must happen quickly, as the ability to see stained areas is limited, usually only 1 to 3 minutes after application.
Other stains such as rose bengal, are not commonly used in the ED and may be irritating. Rose bengal stains devitalize epithelium and is useful for differentiating a herpetic corneal ulcer from a healing corneal abrasion.
Anesthetics
By providing temporary anesthesia, topical anesthetics facilitate eye examination as well as application of diagnostic drops. Most patients cannot tolerate either the application of ocular stains or testing of intraocular pressure (IOP) without topical anesthesia. Application of a topical anesthetic to the eye of a patient with a presumed corneal epithelial defect can be both therapeutic and diagnostic. The topical anesthetic provides patients immediate pain relief and supports the diagnosis of a corneal injury. Topical anesthetics are not for repetitive use, as they suppress protective ocular blink reflexes, have been linked to delayed corneal healing, and may cause an anesthetic-induced keratitis.
Tetracaine hydrochloride (Pontocaine) (0.5% to 1% solution) may initially sting. Its effect lasts for approximately 15 minutes.
Proparacaine hydrochloride (Ophthetic, Ophthaine) (0.5% solution) is less irritating than other solutions.
Mydriatics and Cycloplegics (Red Cap)
These agents are used diagnostically or therapeutically to dilate the pupil (mydriasis) and/or to paralyze the ciliary body (cycloplegia). This effect facilitates evaluation of the internal ocular structures and blocks accommodation. In addition, these agents prevent formation of synechiae (adhesions of the iris to the lens and cornea) by reducing intraocular inflammation through stabilization of the blood–aqueous barrier and by physically pulling the iris away from greater contact with the anterior lens surface. Mydriatic agents are stored in containers capped in red. The duration of drug effects listed below are for normal, noninflamed eyes.
Phenylephrine hydrochloride (Neo-Synephrine, Mydfrin) constricts the surface vessels and dilates the pupil without causing cycloplegia. The 2.5% solution is recommended because of increased systemic (cardiovascular) side effects with 10% solution. The effect lasts approximately 3 hours.
Tropicamide (Mydriacyl 0.5% and 1%) provides short-term dilation of the pupil, plus cycloplegia (lasting 4 to 6 hours). Tropicamide is relatively easy to reverse if there is a concern about iatrogenic angle-closure glaucoma. It is commonly used by ophthalmologists.
Cyclopentolate hydrochloride (Cyclogyl 0.5%, 1%, and 2%) is the best short-term cycloplegic for determining refractive error; it may last from 6 to 24 hours.
Homatropine hydrobromide (1%, 2%, and 5%) lasts for several days. It is a useful short-term mydriatic and cycloplegic for low-level inflammation (iritis) caused by trauma or abrasions.
Scopolamine hydrobromide (Hyoscine 0.25%) lasts between 4 and 7 days; it is more effective for long-term inflammation seen postoperatively or in severe uveitis.
Atropine sulfate (0.25% to 2% solution, 0.5% and 1% ointment) lasts for 10 to 14 days; it is most commonly used postoperatively and in severe uveitis. It carries both corneal epithelial and systemic toxicities.
THERAPEUTIC AGENTS
Lubricants
Dry eyes may be the result of decreased tear production, systemic disease, environmental factors, medication effects, or inadequate lid function. Patients with dry eyes may complain of itching, blurred vision, burning, or a foreign-body sensation. Artificial lubricants temporarily restore the precorneal tear film and provide an effective but short-term treatment for dry eye-related symptoms.
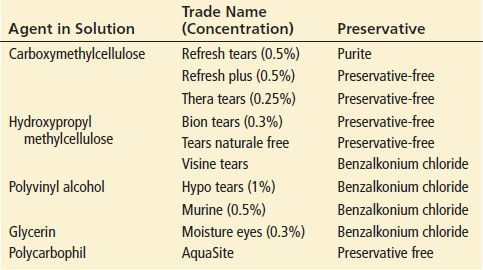
Artificial tears are often used. Most of these formulations (Table 55.1) contain “thickening” agents (such as methylcellulose or polyvinyl alcohol), which prolong retention of the tears on the ocular surface. Most formulations contain preservatives to prevent contamination, but patients who find these preservatives irritating may opt for more expensive, single-use packets. Artificial tears are generally recommended for use every 4 to 6 hours but may be used as frequently as hourly if needed.
TABLE 55.1
Artificial Tear Preparations
Bland lubricating ointments (Lacri-Lube, Refresh P.M.) are more viscous than drops, making these agents useful for maximizing sleep-related lubrication or for patients with incomplete lid closure (e.g., those who have seventh cranial nerve palsy).
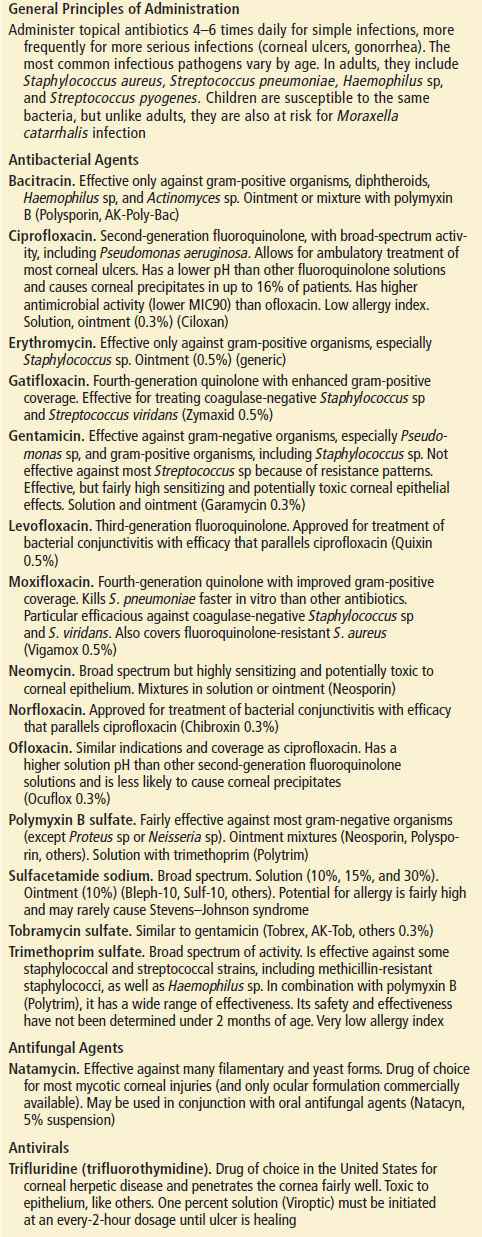
Antibiotics (Tan Cap)
The general principles of antibiotic therapy apply to topical antibiotics as well. See Table 55.2 for a detailed description of ocular antimicrobial agents.
TABLE 55.2
Antibiotics for Topical Use (Tan Cap)