5 Jeffery M. Jones and Dan Miulli Consciousness is defined for medical purposes as the awareness of self and environment. Coma is a more severe form of depressed consciousness in which the patient’s view of self and environment is not only inaccurate or misperceived, but is a state in which the brain is not able to receive stimuli from the environment without aggressive stimulation. Even with aggressive stimulation the patient is not awake enough to process environmental stimuli to any significant extent, and awareness of self is only on the very basic sensory levels (e.g., pain). The patient’s interaction with the environment during coma is, at best, reflexive. The most commonly used grading system of consciousness (or coma) is the Glasgow Coma Scale (GCS). Coma is usually defined as a GCS score of 8 or less. Comatose patients, at best, open their eyes to painful stimulation and will localize to pain. Anatomically, coma can be caused by diffuse cortical dysfunction or by a dysfunction of the reticular activating system located in the brainstem (midbrain) (see Table 4–1 on page 35).1 Most neurosurgical services do not become involved in the initial evaluation of a patient presenting to the ER in a coma of unknown etiology; however, it is useful to review the proper initial management of a comatose patient who has not received any laboratory or radiographic workup (Table 5–1).
Coma
 Initial Care of the Coma Patient
Initial Care of the Coma Patient
| Goal | Method |
| Ensure patent airway and adequate oxygenation | Start mechanical ventilation or O2 by mask if patient is breathing on his or her own |
| Protect C-spine | Immobilize C-spine with cervical collar |
| Maintain MAP above 100 | Use fluids and vasopressors as necessary |
| Treat possible metabolic cause(s) after initial blood draw | Thiamine 100 mg IV, then glucose 25 g IV (d50) |
| Treat increased ICP if there is strong suspicion | Mannitol 0.25–1 g/kg bolus |
| Treat seizures | Benzodiazepine IV (Ativan 2 mg IV) |
| Restore acid–base balance | Judicious use of fluids (0.9% saline preferred) |
| Treat any suspected drug overdose | Naloxone 0.2 mg IV and repeat; physostigmine 1 mg IV; flumazenil 0.2 mg IV |
| Rule out space-occupying lesion | Stat CT scan of head |
| Normalize body temperature | Warm fluids and warming blankets |
| Treat any suspected meningitis or systemic infection | Wide-spectrum antibiotics |
| Specific therapy ASAP |
ASAP, as soon as possible; CT, computed tomography; d50, dextrose 50; ICP, intracranial pressure; IV, intravenous; MAP, mean arterial pressure.
 Causes of Coma
Causes of Coma
Causes of coma can be broken down into two main categories, structural and metabolic. Structural causes are due to lesions physically interfering with nervous system pathways by trauma, compression due to the lesion, or increased pressure. Metabolic causes are due to chemical imbalances leading to improper functioning of the nervous system or some of its components (Table 5–2).1
| Structural coma | Metabolic coma | |
| Hematoma | Hypoglycemia | Hypothermia/hyperthermia |
| Trauma | Adrenal failure | Hypo-/hyperosmolarity |
| Tumor | Liver disease | Diabetic ketoacidosis |
| Hydrocephalus | Renal disease | Encephalopathy |
| Abscess | Pulmonary disease | Drugs |
| Dialysis disequilibrium | Toxins |
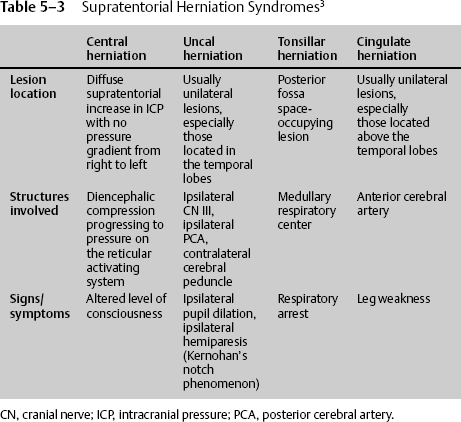
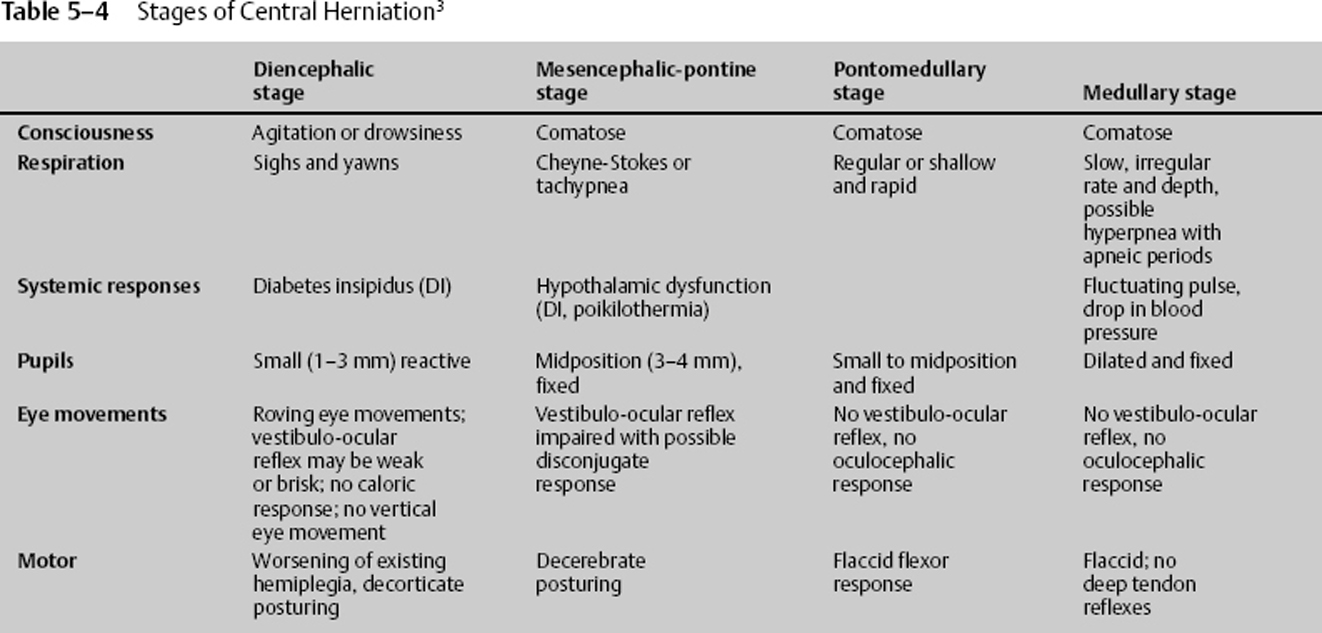
Structural lesions can cause coma through three general mechanisms: compression of the brainstem, direct damage to the brainstem, or diffuse dysfunction of the cerebral hemispheres. Damage to the brainstem can occur through a primary effect on the brainstem such as a tumor, hemorrhage, or infarct of the brainstem, or it can be due to external pressure on the brainstem by another part of the brain that contains the pathology. This can be due to pathology that causes transtentorial herniation of the diencephalon or medial temporal lobe, or it can be due to a posterior fossa lesion causing compression of the brainstem. Supratentorial pathology tends to lead to one of the herniation syndromes listed in Table 5–3. The herniation syndromes, especially uncal and central herniation, pass through the diencephalic, mesencephalic-pontine, pontomedullary, and medullary stages. The tonsillar and cingulate herniation syndromes may be progressive, but their progression is less well defined. Posterior fossa lesions may also lead to supratentorial herniation by causing an obstructive hydrocephalus, which can also result in herniation (Tables 5–4 and 5–5).2
| Early third nerve stage | Late third nerve stage | |
| Consciousness | Agitated or drowsy | Obtunded |
| Respiration | Normal | Hyperventilation |
| Pupils | Relative dilation of ipsilateral pupil | Fully dilated pupil |
| Eye movements | Oculocephalic or normal disconjugate | |
| Motor | Appropriate to pain (localizes), contralateral Babinski’s sign | Possible ipsilateral hemiplegia (Kernohan’s notch), decerebrate |
 Evaluation of Coma Patient
Evaluation of Coma Patient
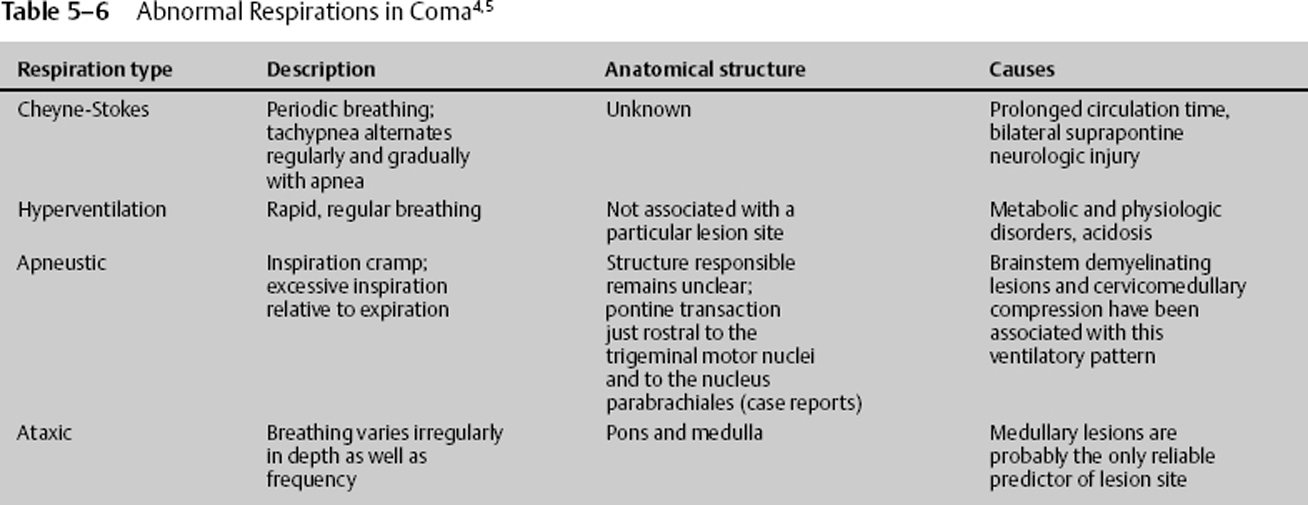
Respiratory Patterns in Coma
The pattern of respiration can give some insight as to the source of coma and possibly indicate where in the brain the dysfunction lies. Table 5–6 summarizes the different types of respiration and their meaning. Both metabolic and structural lesions can give rise to abnormal respiratory patterns.3,4
Ocular Findings in Coma
Ocular findings are most informative in comatose patients, especially in those who do not have a motor response to noxious stimuli. Some generalizations can also be made concerning the pupillary responses:
- Normal pupillary responses strongly favor a metabolic process in a coma of unknown origin.
- The size of the pupils can give a clue as to the type of metabolic process that may be involved (e.g., narcotic overdose, anticholinergic toxicity).
- Pupillary responses can be the most useful information regarding metabolic versus structural lesion short of imaging (Table 5–7).5
Outcome of Coma6
- Twenty percent of comatose patients (GCS = 3) survive; 10% have functional survival.
- Age > 60 years significantly reduces the chances of a good outcome.
- Hypotension and hypoxia double morbidity and mortality.
| Structure | Finding | Meaning |
| Eyelids | Widened palpebral fissure | Facial paralysis |
| Absent corneal reflex | Dysfunction of CN5 or CN7 or their connection | |
| Ocular movements | Ping-pong gaze | Bilateral cerebral dysfunction |
| Horizontal gaze deviation | Ipsilateral frontal eye field dysfunction, contralateral seizure; unilateral pons lesion gives ipsilateral gaze palsy | |
| Vertical gaze disturbance | Posterior diencephalic and midbrain dysfunction | |
| Ocular bobbing | Extensive structural pontine damage | |
| Disconjugate ocular bobbing | Pontomesencephalic damage | |
| Reverse bobbing (fast phase upward) | Metabolic encephalopathy, most prominently in anoxia |
CN, cranial nerve.
- Traumatic subarachnoid hemorrhage (SAH) is a significant independent prognostic indicator of poor outcome. It occurs in 26 to 53% of traumatic brain injuries, and mortality is increased twofold.
- Midline shift of 0.5 to 1.5 cm in patients > 45 years of age is correlated with poor outcome.
< div class='tao-gold-member'>