Risk assessment tool
The process:
Proactive assessment
Undertaken to prevent a patient safety incident
For example, increasing numbers of deliveries in the unit. Rate of significant postpartum haemorrhage 1%. The fluid warming devices available were old and inadequate to manage the potential risk, put on the risk register (Consequence 5 × Likelihood 3 = 15). Two rapid infusors purchased within 6 weeks.
Reactive assessment (Table 28.2)
In response to an incident
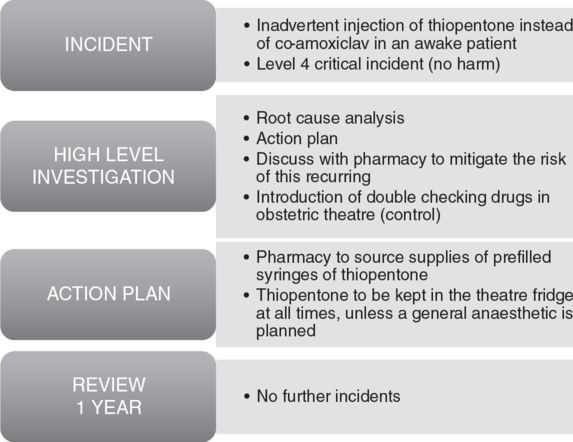
Reactive assessment
Risk control options
The main aim of risk management is to ensure effective controls are in place to mitigate established risks. As stated before, risks are inevitable in any healthcare system and it is important to understand that risks cannot be eliminated completely.
The controls put in place target both the elements of the risk and reduce the consequence to the patient and organization. Measures used to implement controls include: policies, guidelines, procedures, checks and human factors that are used by the organization. The residual risk must be regularly monitored and reviewed.
Complaints
Approximately 140,000 are made to the NHS annually. Any complaint about an aspect of treatment or care can be submitted by the patient or by someone else affected. This has to be within 12 months of the clinical episode. The patient advice and liaison service (PALS) will often resolve the issue at the time, if not then they will provide the information to make a formal complaint.
As a clinician, the best way to deal with dissatisfaction is to be honest and open about the patient’s concerns. The vast majority of complaints involve poor communication.
Written complaints must be acknowledged within 3 working days, together with an offer to discuss the matter. A response should be made within 6 months. Complaints should be part of the agenda at each clinical governance meeting.
Clinical negligence claims
The NHS Litigation Authority (NHSLA) was established in 1995: its purpose was to manage clinical negligence claims on behalf of the NHS in England.
The Clinical Negligence Scheme for Trusts (CNST) is administered by the NHSLA. The remit of the organization was to provide indemnity to member trusts and their employees with respect to clinical negligence claims.
The NHSLA provided a framework of risk management standards to reduce the likelihood of patient safety incidents. The Maternity CNST standards were related to all aspects of obstetric care. The assessment relied predominantly on guidelines and audit for each domain. The benefit of the assessment, if passed, was a reduction in the Trust indemnity payment to the NHSLA. The NHSLA website stated that assessments provided organizational information, but did not reflect quality of care or patient outcomes.
From 1st April 2014, there will be no more assessments and no further updates to the standards from the NHSLA. The standards will be devolved to clinical teams. The agenda will be focused on patient care, quality and patient safety improvements to reduce harm and provide meaningful outcome data.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






