CHAPTER 71
Chronic Obstructive Pulmonary Disease
Viswanath P. Vasudevan, MD
The term chronic obstructive pulmonary disease (COPD) is commonly used to denote chronic bronchitis and emphysema, as these diseases frequently coexist in patients. The Global Initiative for Chronic Obstructive Pulmonary Disease (GOLD), a joint project of the National Institute of Health (NIH) and the World Health Organization (WHO), defines COPD as “a common preventable and treatable disease, characterized by persistent airflow limitation that is usually progressive and associated with an enhanced chronic inflammatory response in the airways and the lung to noxious particles or gases, primarily caused by cigarette smoke. Exacerbations and comorbidities contribute to the overall severity in individual patients” (Vestbo et al., 2013).
COPD is a leading cause of disability and death. Patients with COPD experience recurrent life-threatening exacerbations requiring intensification of therapy, emergency department visits, and hospitalizations. The primary care provider can play a key role in identifying the disease in at-risk patients, providing counseling in smoking cessation, controlling symptoms with medications, preventing exacerbations, improving exercise capacity, and enhancing health-related quality of life.
 ANATOMY, PHYSIOLOGY, AND PATHOLOGY
ANATOMY, PHYSIOLOGY, AND PATHOLOGY
The airway changes in COPD that lead to obstruction include marked enlargement of bronchial mucous glands, gland duct dilation, hypertrophy of airway smooth muscle, and squamous metaplasia of the airway epithelium, causing hypersecretion of mucus and inflammation. The respiratory bronchioles show epithelial hyperplasia, increased numbers of pigmented macrophages, edema, and fibrosis. The membranous bronchioles are obstructed by inflammation, mucus plugs, goblet cell metaplasia, fibrosis, and increased smooth muscle.
In emphysema, there is destruction of alveoli and dilatation of air space distal to terminal bronchioles. In emphysema, smoke-induced elastase overwhelms the inhibitory action of endogenously synthesized protease inhibitors and destroys alveolar capillary membranes and causes dilatation of airspace distal to the terminal bronchiole. Based on the location of the disease within the acinus/lobule, three forms of emphysema are described:
 Centriacinar emphysema initially involves the respiratory bronchioles, with later involvement of the acinus.
Centriacinar emphysema initially involves the respiratory bronchioles, with later involvement of the acinus.
 Centrilobular emphysema is associated with cigarette smoking and predominantly involves the upper lobes.
Centrilobular emphysema is associated with cigarette smoking and predominantly involves the upper lobes.
 Panacinar emphysema uniformly affects the acinus and predominantly involves the lower lobes.
Panacinar emphysema uniformly affects the acinus and predominantly involves the lower lobes.
Paraseptal emphysema occurs in areas adjacent to fibrous septa or pleura. Airflow limitation is mild, but it is implicated as a potential cause of pneumothorax.
Functional residual capacity (FRC), the end exhalation lung volume during tidal breathing, reflects the balance between expiratory lung elastic recoil and inspiratory chest wall elastic recoil. Alveolar pressure is normally zero at FRC. Emphysema reduces lung elastic recoil, causing a new equilibrium of lung and chest wall elastic forces at an increased FRC and causes lung hyperinflation.
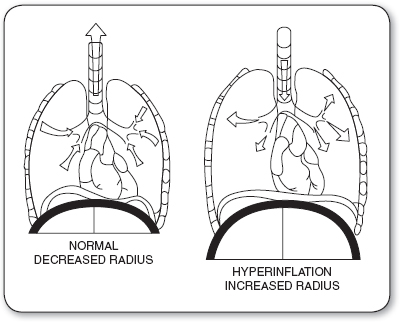
Hyperinflation flattens the contour of the diaphragm and increases its radius of curvature (picture the diaphragm as part of the circumference of a circle that extends over the abdomen). It also shifts the operational lung compliance from the normal region to the low-compliance region, thus increasing pressure requirements for a tidal volume. The increased radius of curvature impairs diaphragmatic contractility and increases respiratory muscle work (Figure 71.1).
Increased airway resistance from airway narrowing in chronic bronchitis and loss of radial traction in emphysema prolongs expiration and produces premature airway closure. Premature airway closure results in the trapping of gas volume with positive alveolar pressures at end expiration (PEEP), also called auto-PEEP. This positive pressure must be overcome before inspiration can proceed. This increases the inspiratory work of breathing.
The emphysematous lung is ventilated but not perfused. It forms dead space, that is, wasted ventilation with areas of low gas diffusion, increasing the work of breathing. The respiratory muscles compensate by increasing the global minute ventilation and maintain PaCO2 in the eucapnic range in earlier stage of the disease. The patient huffs and puffs to maintain ventilation and has thus been called a “pink puffer.”
FIGURE 71.1
The normal lung on the left has a small radius of curvature for the diaphragm. The hyperinflated lung of chronic obstructive pulmonary disease on the right has a large radius of curvature. The pressure generated by the diaphragm is inversely related to the radius of the curvature of the diaphragm.
In chronic obstructive bronchitis, poorly ventilated alveoli remain perfused. This causes hypoxemia with cyanosis and hypercapnia results from depressed chemosensitivity of the respiratory center in the medulla. Chronic respiratory acidosis, compensated by metabolic alkalosis, blunts the ventilatory response to hypercarbia. Uncontrolled oxygen therapy abolishes the hypoxemic ventilatory drive and produces carbon dioxide narcosis.
Chronically elevated pulmonary vascular resistance from hypoxia results in pulmonary arterial hypertension and chronic cor pulmonale. This is manifested by tricuspid valve insufficiency, right atrial dilatation, dilated neck veins, hepatic congestion, and pedal edema. The appearance of cyanosis with edema yields the designation “blue bloater” for such patients.
Total ventilation in these patients is high compared to that of normal persons. This reflects high dead space ventilation and an unusually high respiratory drive. Emphysematous patients have a still higher respiratory drive.
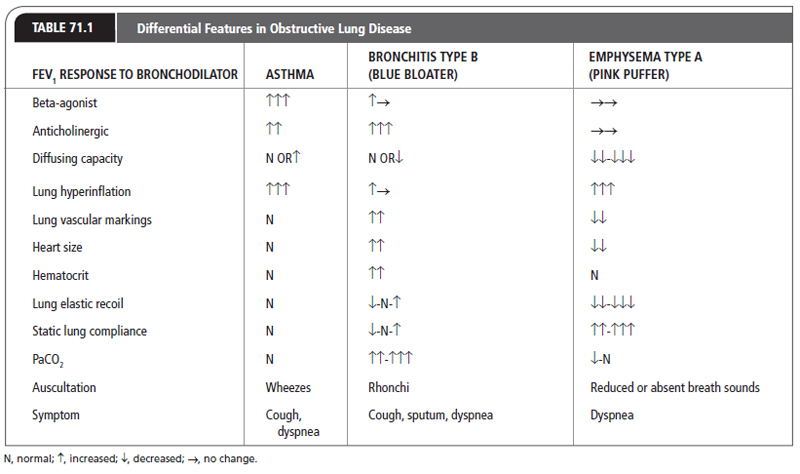
The features of asthma, bronchitis, and emphysema are compared in Table 71.1.
 EPIDEMIOLOGY
EPIDEMIOLOGY
In the United States, COPD affects more than 5% of the adult population; it is the third leading cause of death (120,000 deaths annually) and the 12th leading cause of morbidity. The total economic costs of COPD in the United States were estimated to be $49.9 billion in 2010, and the total direct cost of medical care is approximately $29.5 billion per year. The burden of COPD is projected to increase in coming decades due to continued exposure to COPD risk factors and the aging of the world’s population (American Thoracic Society/European Respiratory Society Task Force, 2013; Lung Health Study Research Group, 2000).
About 1% to 2% of patients with COPD have alpha-1 antitrypsin deficiency (AAT). The genetic locus responsible for AAT production is termed Pi. The Mallele and phenotype Pi MM is found in 90% to 95% of the normal White population. Persons homozygous for the phenotype of the Z allele (Pi ZZ) manifest AAT deficiency. Those with disease have AAT levels that average 16% of normal. These patients present with early-onset panacinar lower-lobe emphysema.
 DIAGNOSTIC CRITERIA
DIAGNOSTIC CRITERIA
A clinical diagnosis of COPD should be considered in any patient who has dyspnea, chronic cough with sputum production, and a history of exposure to risk factors for the disease, that is, tobacco smoke, occupational dusts, organic and inorganic indoor air pollution liberated from heating and cooking with biomass fuel in poorly ventilated dwellings. The diagnosis of chronic bronchitis is based on the presence of a chronic cough with sputum production for 3 months per year in 2 successive years. Chronic bronchitis accompanied by airway obstruction is called chronic obstructive bronchitis to distinguish it from simple bronchitis, which does not limit airflow.
The diagnosis of emphysema is made by histologic findings of abnormally widened air spaces and destruction of lung tissue distal to the terminal bronchioles. Clinically the diagnosis is made by a combination of history, physical exam, and radiologic and pulmonary function findings. Alveolar destruction transforms the gas-exchanging surface into a nonfunctional air space. This is identified on pulmonary function testing as a decrease in the diffusing capacity of the lung.
The typical patient with COPD presents with overlapping features of more than one of these diseases. Most have a history of cigarette smoking, often exceeding 20 pack-years. However, only 15% of cigarette smokers develop clinically significant COPD. For patients who progress to disease, the long interval between the onset of smoking and the onset of clinical findings reflects the tremendous reserve of lung function that has to be destroyed before a patient becomes symptomatic. This also explains why most patients begin to seek help in their fifth and sixth decades of life.
Although most patients with COPD are older, long-time cigarette smokers, an important exception is the young patient with AAT-deficiency emphysema. This inherited defect, characterized by a very early onset of emphysema, involves the lower lobes of the lung instead of the upper lobe, found in older patients. Smoking causes an even earlier onset of the disease. This defect can now be corrected with replacement of the deficient AAT, making an accurate diagnosis essential.
 HISTORY AND PHYSICAL EXAMINATION
HISTORY AND PHYSICAL EXAMINATION
Chronic cough with morning sputum production is the first symptom of chronic bronchitis. Sputum usually has a clear, mucoid appearance, but becomes mucopurulent and thick and increases in quantity and frequency during acute exacerbations.
Lung hyperinflation may manifest as an increased anteroposterior diameter of the chest. In the stable patient, auscultation of the lung reveals decreased or absent sounds in emphysema and low-pitched sonorous rhonchi in bronchitis. During exacerbations, higher-pitched wheezes are heard. Dyspnea and tachypnea become more prominent and can progress to both inspiratory and expiratory use of accessory muscles of respiration. Increased intrapleural pressure excursions manifest as inspiratory intercostal muscle retractions, expiratory supraclavicular apical bulging, neck vein distention, and increased tracheal movement.
In severe exacerbations, prominent flaring of the alae nasi occurs. Patients place their elbows on firm surfaces, enabling the shoulder girdles to project away from the chest to enhance the effect of respiratory muscle motion.
During exacerbations of emphysema, patients become tachypneic and may manifest cyanosis if there is significant impairment of alveolar gas exchange. In the chronically hypoxemic patient, signs of cor pulmonale may be present. These include jugular venous distention, hepatomegaly, and pedal edema. Acute and chronic hypercapnia contribute to alveolar hypoxia, and produce cerebral vasodilatation with symptoms of headache and mental obtundation.
Patients with COPD have worsening hypoxemia and hypercarbia most pronounced during rapid eye movement (REM) sleep. This produces sleep fragmentation, nonconsolidated sleep, and excessive daytime sleepiness. Nocturnal prolonged hypoxemia can manifest as polycythemia, pulmonary arterial hypertension, and right heart failure.
 DIAGNOSTIC STUDIES
DIAGNOSTIC STUDIES
Chest x-ray is insensitive for the diagnosis of COPD. It may reveal lung hyperinflation, better visualized in the lateral projection as increased in retrosternal air space and flattened diaphragms. Paucity of vascular markings and bullae are visualized in patients with emphysema. Chest x-ray is a valuable tool to exclude alternative diagnoses or detect complications like pneumonia, pneumothorax, or heart failure. Finger pulse oximetry can be used to evaluate a patient’s oxygen saturation and assess the need for supplemental oxygen therapy. Arterial blood gas analysis is needed to confirm clinical suspicion of decompensated ventilatory failure in patients who present with acute exacerbations. AAT should be suspected in young (<45 years of age) patients of Caucasian descent with a strong family history of COPD and basilar panacinar emphysema. Effort tolerance is objectively measured by 6-minute walking distance or by measuring maximal oxygen consumption (VO2) during incremental maximal cardiopulmonary exercise test.
CT of the lungs is a very sensitive tool in the detection of the location and severity of emphysema and has facilitated early diagnosis, thus enabling intervention early in the disease.
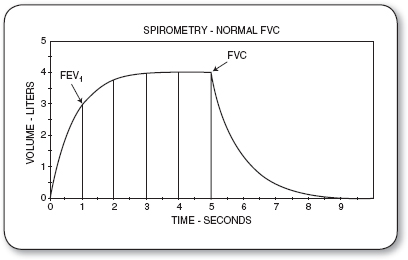
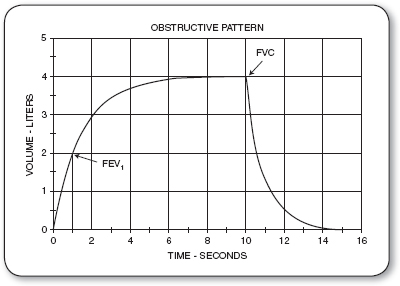
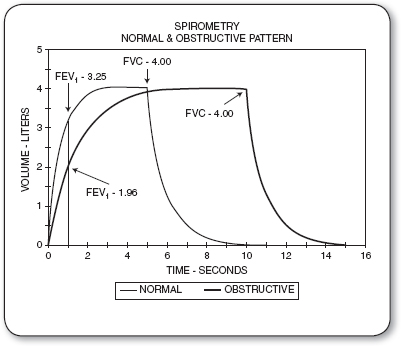
Spirometric measurement of the ratio of the volume expired in the first second (FEV1) divided by the maximal volume that can be exhaled from the lung after a maximal inspiration (forced vital capacity [FVC]) gives a measure of the expiration rate, or the FEV1/FVC ratio. Airway obstruction is associated with a low FEV1/FVC ratio (<0.70, age corrected; Figures 71.2–71.4). This is related to a reduction in the FEV1. The response of the FEV1 to the administration of a bronchodilator establishes the degree of reversibility of the obstruction (Wedzicha et al., 2008).
The asthmatic airway responds to beta-adrenergic agonist inhalation with significant increase in FEV1 by >200 mL and >12%, but the airway in COPD demonstrates insignificant response, that is, by <200 mL and <12% change. The bronchodilator response helps identify the phenotype group of patients with overlap of asthma and COPD, who could benefit from inhaled corticosteroid (ICS) therapy.
The diffusing capacity of the lung for carbon monoxide (DLCO) is useful in differentiating the three main obstructive diseases. It is normal or slightly decreased in chronic bronchitis, and always significantly decreased in emphysema. A low DLCO is required to establish the diagnosis of emphysema by pulmonary function testing. A small subset of patients with emphysema may have isolated reduction in diffusing capacity without airflow obstruction.
Static lung volumes are often increased in COPD. Emphysema shows the largest increases in static lung volumes, that is, residual volume (RV), FRC and total lung capacity (TLC) with increased RV/TLC ratio, and a sign of air trapping. This pattern fails to reverse completely with inhaled bronchodilator therapy. In asthma, the increased lung volumes are reversible after therapy. Chronic bronchitis may show a slight irreversible increase in lung volume. An increased RV/TLC ratio is characteristic of all obstructive diseases.
FIGURE 71.2
Normal pattern. The expired volume trace rises steeply so that at 1 second, a major part of the volume has already been expired (FEV1). The total expired volume is the forced vital capacity (FVC) and is expired in 5 seconds.
FIGURE 71.3
Obstructive pattern: The expired volume trace rises with a low slope in contrast to the normal spirometric pattern. At 1 second, less volume has been expired compared to the normal trace. The total expired volume in this example is comparable to that of the normal but has required 10 seconds to be expired.
FVC, forced vital capacity; FEV1, volume expired in the first second.
FIGURE 71.4
Comparison of the expiratory volume-time traces for the FVC and FEV1 in a normal subject and in COPD. Note the difference in volume expired at 1 second and the duration in seconds for full expiration.
COPD, chronic obstructive pulmonary disease; FVC, forced vital capacity; FEV1, volume expired in the first second.
The shape of the spirometric flow-volume curve in a FVC is useful in assessing airway disease. After peak flow has been attained, normal spirometric flow slopes downward in a linear relation with respect to expired volume. In obstruction, this linearity is transformed into a concave relation of flow to volume. In contrast, in advanced emphysema, the slope is converted into a low peak followed by plateau of flow. The linear and concave slopes reflect a change in diameter of the airway during expiration. The plateau of emphysema reflects a fixed airway diameter due to a loss of the tethering effect of elastic fibers in the surrounding lung structures.
 TREATMENT OPTIONS, EXPECTED OUTCOMES, AND COMPREHENSIVE MANAGEMENT
TREATMENT OPTIONS, EXPECTED OUTCOMES, AND COMPREHENSIVE MANAGEMENT
In the Western world, the major risk factor for the development of COPD is cigarette smoking, accounting for 80% to 90% of the total risk. The prevalence of COPD increases with age and reflects the cumulative effects of cigarette smoke. Cigarette smoking has a greater effect on lung function before age 40 years than later in life. The number of cigarettes smoked daily is strongly associated with the risk of chronic bronchitis. Among cigarettes, maize leaf cigarettes are associated with the highest risk and filtered cigarettes the lowest.
The FEV1 in the normal nonsmoking population declines annually by 25 to 30 mL starting at about age 35 years. The rate of decline is greater in smokers. On cessation of smoking, the rate of FEV1 decline can revert to that of the nonsmoking population. The slope for rate of decline can thus resume a course parallel to that of nonsmokers, but at a lower level of absolute FEV1.
In developing countries, indoor air pollution liberated from heating and cooking with biomass fuel in poorly ventilated dwellings has been implicated as a risk factor for COPD. The combination of tobacco smoke and air pollution appears to increase the risk for development of COPD.
Prevention
Goals of therapy in stable COPD are identification and reduction of exposure to risk factors. Smoking cessation has the greatest capacity to positively impact the natural history of COPD. It has the greatest impact in reducing annual decline in lung function. Health care providers should encourage all patients who smoke to quit. Group smoking cessation programs and information on smoking cessation are provided by organizations such as the American Lung Association, the American Cancer Society, and the American Heart Association. Pharmacotherapy and nicotine replacement are effective in sustaining long-term smoking abstinence rates. Provider counseling significantly improves quit rates over self-initiated strategies. Nicotine replacement therapy (nicotine gum, inhaler, nasal spray, transdermal patch, sublingual tablet, or lozenge, and potentially the electronic cigarette), as well as pharmacotherapy with varenicline, bupropion, and nortriptyline, reliably increase long-term smoking abstinence rates and are significantly more effective than placebo. Patients should be counseled to eliminate/reduce exposures to air pollutants, that is, avoid indoor air pollution from biomass fuel, burned for cooking and heating in poorly ventilated dwellings. Patients are advised to monitor public announcements of air quality and stay indoors during pollution episodes.
Patients with COPD are at greater risk for developing infectious bronchitis and pneumonia. Influenza vaccines can reduce serious illness. Pneumococcal polysaccharide vaccine is recommended for COPD patients 65 years and older and for COPD patients younger than age 65 years with an FEV1 <40% predicted. Influenza and pneumococcal vaccinations help reduce the risks of future exacerbations.
Treatment
Personalized therapy based on GOLD assessment, COPD phenotypes, symptoms, airflow limitation, and future risk of exacerbations should be incorporated into the management strategy (Niewoehner et al., 2005).
Severity Assessment
The goals of COPD assessment are to categorize disease severity, based on severity of obstruction to airflow, daily symptom burden, risk for periodic exacerbations, and impact on the patient’s overall health status. COPD patients are at an increased risk for cardiovascular diseases, osteoporosis, respiratory infections, anxiety, depression, diabetes mellitus, and lung cancer. These chronic comorbid conditions may influence mortality and hospitalizations.
Symptoms are assessed by using any of the following validated tools:
 COPD self-assessment questionnaire test (CAT): An eight-item measure of health status impairment in COPD (catestonline.org).
COPD self-assessment questionnaire test (CAT): An eight-item measure of health status impairment in COPD (catestonline.org).
 Breathlessness measurement using the modified British Medical Research Council (mMRC) questionnaire (Figure 71.5): Relates well to other measures of health status and predicts future mortality risk.
Breathlessness measurement using the modified British Medical Research Council (mMRC) questionnaire (Figure 71.5): Relates well to other measures of health status and predicts future mortality risk.
 Clinical COPD Questionnaire (CCQ): Self-administered questionnaire developed to measure clinical control in patients with COPD (www.ccq.nl).
Clinical COPD Questionnaire (CCQ): Self-administered questionnaire developed to measure clinical control in patients with COPD (www.ccq.nl).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree