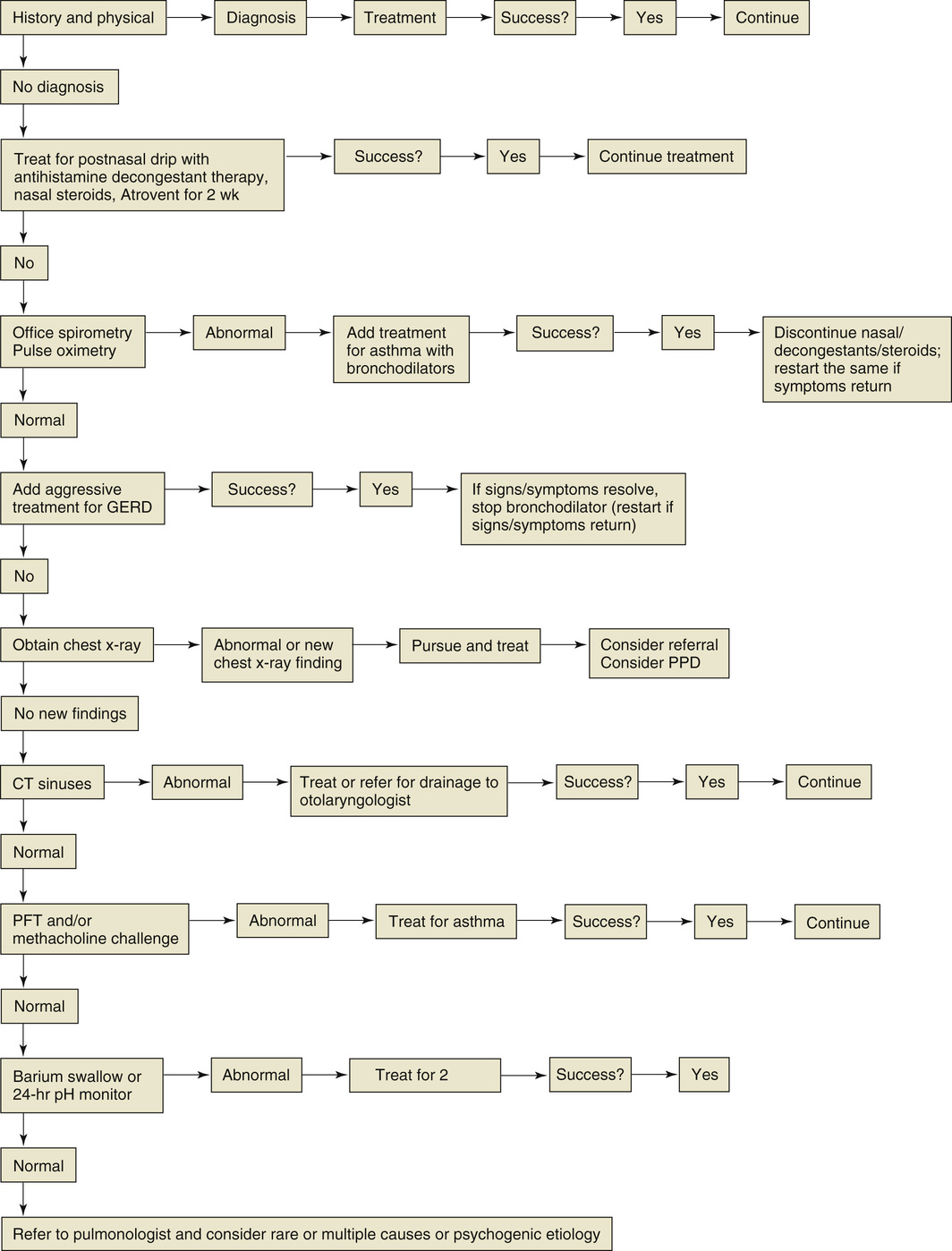
Patricia Polgar-Bailey Cough is a common symptom in persons with a wide range of respiratory and nonrespiratory diseases, as well as individuals who are not ill.1 Cough, an important reflex action and respiratory defense mechanism, is designed to prevent the aspiration of foreign material into the lower respiratory tract and to clear excessive secretions, mucus, fluids, foreign matter, and infectious organisms from the larynx, trachea, and large bronchi.2 Cough has a protective role that is illustrated by the possible complications resulting from cough suppression, such as infections. However, cough can also transmit disease through airborne droplets and the contamination of objects, and it can be associated with complications, particularly when it is chronic. Excessive and chronic cough can result in numerous complications, including headache, anorexia, vomiting, throat pain, subconjunctival hemorrhages, fatigue, insomnia, myalgia, dysphonia, perspiration, urinary incontinence, syncope, rib pain and rib fractures, inguinal or abdominal wall herniations, diaphragmatic rupture, anxiety, and depression.2,3 Chronic cough can have a profound psychological and emotional impact.3 Many adults with chronic cough report feeling self-conscious about their cough and can become socially isolated owing to the associated complications, such as incontinence. In addition, older adults with chronic cough often feel anxious that “something’s wrong”; in studies, a significant percentage have expressed a specific fear of cancer.3 Chronic cough may be a symptom of underlying disease. For these reasons, a persistent chronic cough is a cause for concern for both the patient and the health care provider. Coughs may be classified as acute (lasting less than 3 weeks), subacute (lasting 3 to 8 weeks), and chronic (persisting beyond 8 weeks).3 Most coughs are acute and self-limited; 90% are caused by viral upper respiratory tract infections, two thirds of which clear within 2 weeks.2 Nonviral causes of acute cough include exacerbations of asthma and exposure to environmental pollutants.2 A cough that persists for more than 3 weeks and for which initial treatment has failed should be investigated. Subacute cough is generally caused by bacterial sinusitis or asthma, but it can also be caused by upper respiratory infections. The cough that follows a viral or virus-like infection (e.g., Mycoplasma pneumoniae or Bordetella pertussis) is sometimes referred to as a postinfectious cough. A postinfectious cough, by definition, lasts no longer than 8 weeks; chest radiograph findings are normal, and the cough eventually resolves, generally without intervention.4 Thus, subacute postinfectious cough can be distinguished from chronic cough by the duration of symptoms; the chronic cough lasts for 8 weeks or more and usually much longer.3 The American College of Chest Physicians (ACCP) has developed evidence-based clinical practice guidelines for the management of postinfectious cough, which can be found at chestjournal.chestpubs.org. Cough is reportedly the most frequent reason for visits to primary care providers and accounts for approximately 8% of all encounters.5 In the United States and Europe, cough is estimated to affect 9% to 33% of the population, and its prevalence may be increasing as a result of worsening environmental pollution.1,2 Chronic cough is often related to cigarette smoking, and the prevalence of chronic cough is three times higher in smokers than in nonsmokers or ex-smokers.2 Chronic bronchitis (primarily from cigarette smoking) is another common cause of chronic cough. Exposure to secondhand smoke and other irritants also increases the risk for development of a chronic cough. Chronic cough can have many causes in addition to exposure to cigarette smoke, but only a few diseases account for most cases. In adults, the three most common causes of chronic cough with normal chest radiography include the corticosteroid-responsive eosinophilic airway diseases (asthma, cough variant asthma, and eosinophilic bronchitis), upper airway cough syndrome (previously referred to as postnasal drip syndrome), and gastroesophageal reflux disease (GERD).1 These have been referred to as the pathogenic triad of chronic cough, accounting for almost all cases of cough in immunocompetent, nonsmoking adults who have normal chest radiographs and are not taking angiotensin-converting enzyme (ACE) inhibitors. The incidence of ACE inhibitor–induced cough has been estimated at 10%, but there is geographic variation and in certain countries, such as China, the prevalence is estimated to be as high as 44%.3 An understanding of the anatomic, physiologic, and pathophysiologic aspects of cough is important for diagnosis and appropriate treatment. The systematic, diagnostic protocol uses the anatomic characteristics of the cough reflex and innervation as a guide to finding the cause of the cough (Box 105-1). When a neural receptor along the respiratory tree is stimulated, an afferent signal is transmitted to the “cough center” of the brain, which is located in the medulla. From this center, through a complex reflex arc, the impulse is passed down the efferent pathway to the expiratory musculature. The receptors of the afferent limb can be found anywhere along the respiratory tree. These include the vagus from the ears, larynx, trachea, bronchi, pleurae, and gastrointestinal tract; the trigeminal from the nose and the sinuses; the glossopharyngeal from the pharynx; and the phrenic from the diaphragm. The efferent limb consists primarily of the phrenic and spinal nerves. After the stimulus reaches the cough center, the cough begins with a deep inspiration to approximately 50% of the vital capacity. This allows maximum expiratory flow by increasing the lung elastic recoil and by decreasing airway frictional resistance. During this phase, the glottis opens widely to allow rapid entry of large amounts of air into the lung. The glottis rapidly closes and the abdominal and intercostal muscles contract, increasing the intrapleural pressures to 100 to 200 mm Hg. In a fraction of a second, the glottis reopens, causing an explosive release of air. During this phase, the tracheobronchial tree narrows, resulting in forces sufficient to strip mucus off the walls, creating sputum. A careful and detailed history will provide the diagnosis in the majority of cases of cough. Careful consideration of the various characteristics of cough may aid diagnosis (Fig. 105-1). A cough that lasts for 3 consecutive months for more than 2 consecutive years is indicative of chronic bronchitis. A sudden onset of cough in the supine position with an associated sour taste in the mouth suggests esophageal reflux. A cough associated with constant throat clearing and thick mucus production, especially on rising from bed, is consistent with upper airway cough and sinusitis. A cough associated with rhinorrhea or sneezing may be a viral syndrome or the common cold. If it recurs annually at the same time of year, allergic rhinitis is possible. Intermittent productive cough associated with wheezing is most probably asthma. A loud hacking cough during the daytime that is nonproductive, leads to exhaustion, and is associated with emotional stress may suggest psychogenic cough. In addition, some authors have attributed certain sputum characteristics to a particular disease process (Box 105-2). Evaluation of these attributes may also aid in diagnosis. ACE inhibitors can cause a nonproductive cough more commonly in women, nonsmokers, and persons of Chinese ethnicity.3 The onset of cough may occur within hours of the first dose or can be delayed for weeks to months after the initiation of ACE inhibitor therapy. The cough is not dose related and usually resolves within 1 to 4 weeks after cessation of therapy; however, in a small percentage of patients, the cough may linger for up to 3 months after termination of therapy.3 The history and physical examination can help establish the cause of cough in the majority of cases. Obvious physical examination findings include the following: • Diffuse inspiratory crackles characteristic of pulmonary edema or fibrosis • Expiratory wheezes as in asthma or chronic obstructive pulmonary disease (COPD) • Occasional hair rubbing against the eardrum or cerumen impaction in the canal resulting in the irritation of the auricular branch of the vagus nerve and triggering of cough2 If the cause of the cough remains elusive after a thorough history and physical examination, a chest radiograph should be obtained, even though radiographic findings are diagnostic in only a minority of cases. A normal chest radiograph usually excludes malignant disease, bronchiectasis, persistent pneumonia, sarcoidosis, and tuberculosis. The next step is to reconsider the most likely remaining causes of chronic cough, keeping in mind that chronic cough may fail to resolve because of inaccurate diagnosis or incorrect or insufficient therapy. A chest radiograph will reveal the presence of a lung mass or parenchymal abnormalities, such as sarcoidosis, fibrosis, emphysema, and congestive heart failure. If chest films reveal abnormalities, further diagnostic studies may be indicated, possibly including bronchoscopy, pulmonary function tests (PFTs), computed tomography (CT) scanning of the chest, barium esophagography, and cardiac studies. Bronchoscopy should be planned only for a specific diagnosis, keeping in mind that bronchoscopy has been shown to be of little diagnostic benefit when chest radiograph or CT findings are normal or nonlocalizing.5 If the diagnosis is still not found, routine PFTs are indicated, and if these results are negative, a methacholine challenge test is necessary. At this point, more than 50% of coughs will have been diagnosed. If the cause is still undetermined, a gastrointestinal evaluation with a barium swallow study and 24-hour pH esophageal monitoring should be considered. Further diagnostic tests include a CT scan of the sinuses and otolaryngologic evaluation. The majority of patients should now have a definitive diagnosis. Undiagnosed cases of cough may include psychogenic cough. There is a select group of patients who have a syndrome referred to as chronic idiopathic cough, for which the cause remains elusive. In some cases the precipitating cause of the cough may have disappeared, but its effect on the cough reflex may be more prolonged.1 An example of this might be a transient upper respiratory tract viral infection or an exposure to respiratory toxins, which can cause inflammatory neuropathic changes in the sensory nerves, thereby inducing more prolonged damage to the respiratory mucosa.1 Approximately 25% to 50% of patients have multiple causes of cough.6 Individuals with a compromised immune system require additional diagnostic testing as part of the initial workup. If a patient is immunocompromised, especially because of human immunodeficiency virus (HIV) infection, a chest radiograph and oxygen saturation level should be obtained earlier in the assessment. Chronic comorbid conditions and acute critical illnesses can cause further depression of the immune system, thereby increasing the risk of infection.
Chronic Cough
Definition and Epidemiology
Pathophysiology
Clinical Presentation
Physical Examination
Diagnostics
Chronic Cough
Chapter 105