CHILD ABUSE/ASSAULT
JOANNE N. WOOD, MD, MSHP, JAMES M. CALLAHAN, MD, AND CINDY W. CHRISTIAN, MD
GOALS OF EMERGENCY CARE
Prompt recognition and evaluation of injuries resulting from physical abuse is important to allow for (1) appropriate treatment of the presenting injury, (2) identification of occult injuries including fractures, traumatic brain injury (TBI), or intra-abdominal injury that may require medical intervention, and (3) protection of the child and possibly other children from further injury. Distinguishing abusive injuries from accidental injuries in the ED, however, can be challenging especially in young, preverbal children due to the potential unreliability of caregiver histories and limitations of physical examination in this population. Thus, providers should consider the possibility of physical abuse in young children with injuries without a clear accidental etiology. In children with injuries suspicious for abuse, a thorough evaluation including history and physical examination should be performed once the patient is medically stabilized (Tables 95.1–95.3). Depending on the age of the child, radiologic and laboratory testing for occult injuries may be indicated as victims of physical abuse presenting with minor injuries may have more serious clinically occult injuries (Table 95.4). A report to child protective services (CPS) must be made if the provider has reasonable suspicion that the child may be a victim of abuse. Physicians and nurses are mandated reporters of child abuse in all states; in many states, other healthcare workers are also mandated reporters. Emergency department providers should be familiar with the mandatory child abuse reporting laws governing the area in which they practice. Failure to recognize, evaluate, and report cases of physical abuse can result in children suffering complications from injuries undiagnosed at the time of presentation, and keeps children vulnerable to future abuse that can lead to additional injuries and death.
KEY POINTS
 Physical abuse is common; over 120,000 children are substantiated as victims of physical abuse each year in the United States.
Physical abuse is common; over 120,000 children are substantiated as victims of physical abuse each year in the United States.
 Abuse should be considered in the differential diagnosis of injuries without obvious accidental etiologies.
Abuse should be considered in the differential diagnosis of injuries without obvious accidental etiologies.
 Children <1 year old are at the highest risk of serious and fatal abuse.
Children <1 year old are at the highest risk of serious and fatal abuse.
 Victims of physical abuse may present with misleading histories.
Victims of physical abuse may present with misleading histories.
 Young victims of abuse frequently have occult injuries including fractures, TBI, and intra-abdominal injuries not detected on history or physical examination.
Young victims of abuse frequently have occult injuries including fractures, TBI, and intra-abdominal injuries not detected on history or physical examination.
 Medical providers are mandated to make a report to CPS if there is a reasonable suspicion for abuse.
Medical providers are mandated to make a report to CPS if there is a reasonable suspicion for abuse.
RELATED CHAPTERS
Resuscitation and Stabilization
• Approach to the Injured Child: Chapter 2
Signs and Symptoms
Medical, Surgical, and Trauma Emergencies
• Abdominal Trauma: Chapter 111
• Musculoskeletal Trauma: Chapter 119
• Thoracic Trauma: Chapter 123
INJURIES FROM PHYSICAL ABUSE: GENERAL
Clinical Considerations
Clinical Recognition
Children of all ages may present to the emergency department with abusive injuries, but infants are at the greatest risk of sustaining severe or fatal injuries. Victims of physical abuse may present with injuries to any body system, but cutaneous injuries and fractures are the most common injuries for which victims of physical abuse are brought for care. TBI is also common among young victims of physical abuse and is the leading cause of morbidity and mortality in this population. Intra-abdominal injuries are rare but are the second leading cause of morbidity and mortality from physical abuse.
Triage Considerations
The triage of children with suspected abusive injuries is similar to children with accidental injuries and is dependent on the severity and type of the injury. The severity of the child’s clinical condition may be underestimated initially because the history provided at triage is often false or incomplete.
Clinical Assessment
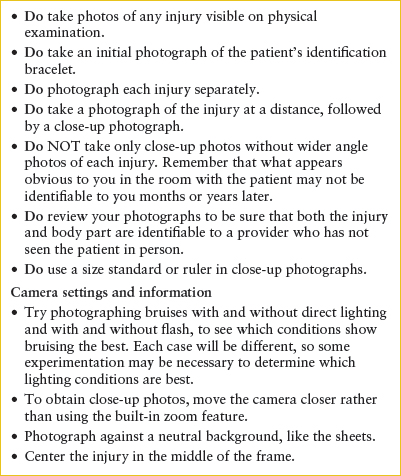
The initial clinical assessment of a child with possible abusive injuries does not differ from the approach for a child with similar accidental injuries. After the child is stabilized, further evaluation is necessary to determine the level of concern for abuse and guide next steps in ensuring the safety of the child. Distinguishing abusive injuries from accidental injuries in the ED can be difficult as there are few single injuries pathognomonic for abuse and overlap exists in the spectrum of injuries resulting from accidental and abusive trauma. Findings on history and physical examination, however, can help to identify cases concerning for abuse that warrant further evaluation (Tables 95.1 and 95.2). A thorough history including history of trauma, developmental history, past medical history, and social history should be performed. A complete physical examination including review of vital signs, thorough skin examination, and neurologic examination, should be performed in addition to the assessment of the presenting injury. If available, photodocumentation with a size standard or ruler should be performed for cutaneous findings (Table 95.5).
TABLE 95.1
FINDINGS IN THE HISTORY THAT MAY BE SUGGESTIVE OF PHYSICAL ABUSE
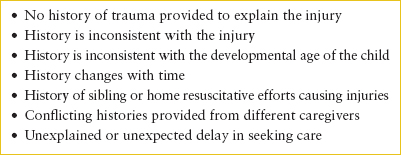
TABLE 95.2
DIFFERENTIAL DIAGNOSIS OF CUTANEOUS FINDINGS SUSPICIOUS FOR PHYSICAL ABUSEa
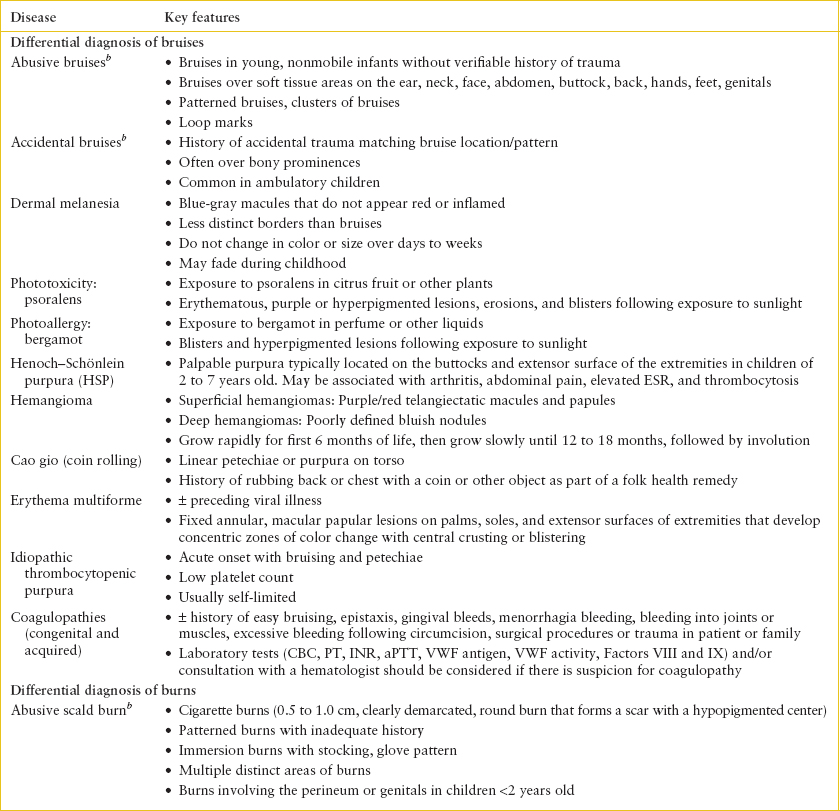
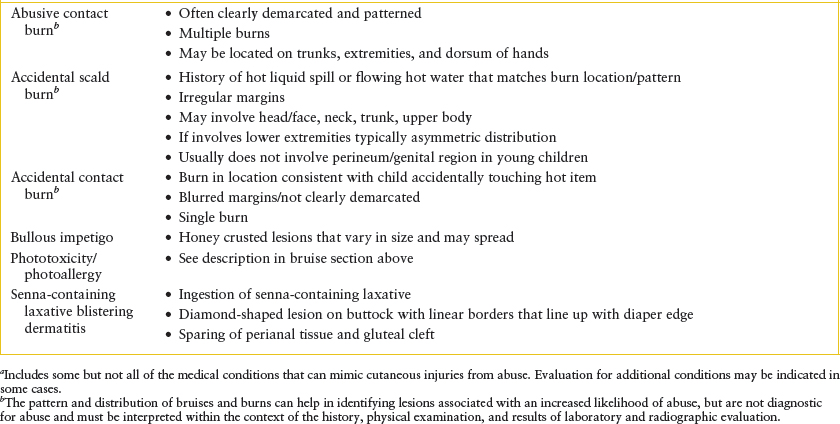
TABLE 95.3
DIFFERENTIAL DIAGNOSIS OF FRACTURES SUSPICIOUS FOR PHYSICAL ABUSEa
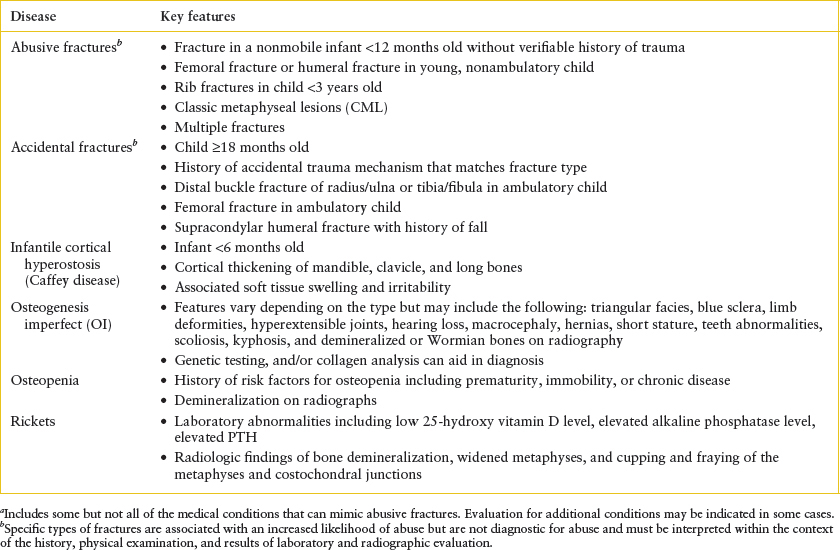
TABLE 95.4
LABORATORY AND RADIOLOGIC TESTS FOR EVALUATION OF OCCULT INJURIES IN CASES OF SUSPECTED PHYSICAL ABUSE
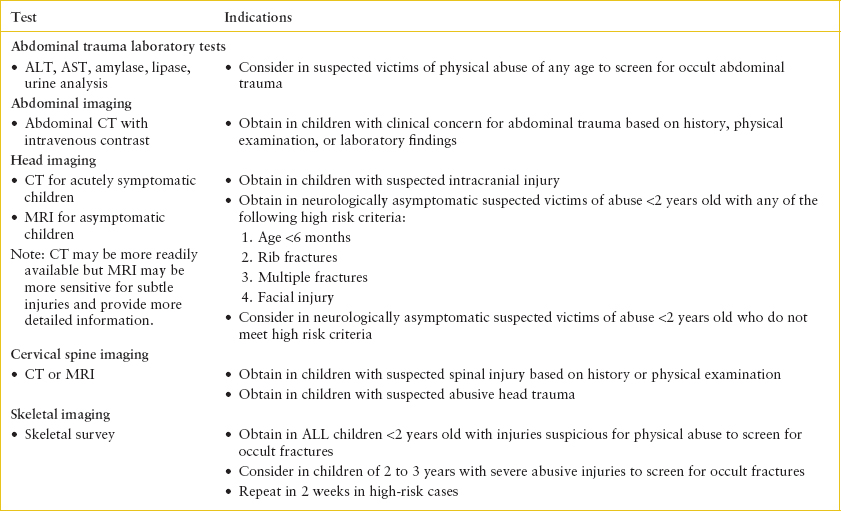
If results of the history and physical examination suggest that an injury is suspicious for abuse, laboratory and/or radiologic studies to screen for occult injuries may be indicated based on the age of the child (Table 95.4). Testing for diseases that may mimic abusive injuries or predispose a child to sustain injuries with minimal accidental trauma such as bleeding disorders in children with unexplained bruising or osteogenesis imperfecta in the children with multiple fractures should be considered as well (Tables 95.2 and 95.3). Although screening tests for some of these disorders may be able to be obtained in the emergency department, it may be necessary to refer patients to appropriate specialists for further testing (e.g., referral to a hematologist for specialized testing for bleeding disorders if a platelet count and basic coagulation profile testing is normal or to a geneticist if there is a concern for osteogenesis imperfecta).
Management
With few exceptions, the initial management of patients with abusive injuries does not differ from the management of children with accidental injuries. Severely injured children should be stabilized prior to the evaluation for suspected abuse being performed. If based on the history, physical examination, and laboratory and radiographic evaluation, the ED provider has a reasonable suspicion to suspect physical abuse; a report to CPS must be made and should be discussed with the caregivers. Children with injuries from physical abuse can be discharged from the ED if the following conditions have been met: (1) Injuries do not require further inpatient management, (2) medical evaluation including evaluation for occult injuries is complete, and (3) a safe discharge environment has been identified; this requires collaboration with the local child welfare agency. If these conditions have not been met, hospital admission may be advisable.
Once the medical provider makes a report, the CPS agency will make a determination as to whether there is sufficient information to suggest that an investigation for suspected child abuse is warranted. If the report is “screened in” for investigation, a CPS caseworker will initiate an investigation which may include but is not limited to speaking with the family, child, medical providers, and other contacts as well as performing a home assessment. After making the report, the medical provider should cooperate with the CPS investigation and provide the relevant medical information. The Health Insurance Portability and Accountability Act (HIPAA) rules allow for medical providers who have made a mandatory report of suspected child maltreatment to share information with CPS without legal guardian authorization. During the investigation, the CPS caseworker will also assess the family’s strengths and needs, and when appropriate provide services to support the family. If there is an immediate concern for the safety of the child in the home environment, the child may be discharged from the hospital to foster care, a relative’s home, or a shelter while the investigation is being conducted, but only a minority of children reported to CPS enter out-of-home placement.
TABLE 95.5
PHOTODOCUMENTATION TIPS
If based on the results of the investigation the CPS worker determines that there is sufficient evidence to conclude that the child was abused, the case will be substantiated or founded. The CPS agency may initiate child protection or child dependency hearings in juvenile court if deemed necessary for the child’s protection. Depending on the severity of the maltreatment and perceived risk for future maltreatment, the CPS agency may determine that the child is safe to remain in their home with voluntary or mandated services for the family. In cases of severe abuse or high risk, the child may be placed in a foster home, relative’s home, or shelter.
CUTANEOUS MANIFESTATIONS OF ABUSE: BRUISES, BURNS, AND BITES
Goals of Treatment
Most cases of abusive bruising do not require medical intervention. Prompt recognition and evaluation of abusive bruising is important, however, to allow for (1) identification of occult injuries including fractures, TBI, or abdominal trauma that may require medical intervention, and (2) protection of the child from further injury. In cases of extensive bruising with muscle breakdown, monitoring for and treatment of rhabdomyolysis and renal failure may be necessary. Abusive burns and bite marks should be medically managed as clinically indicated based on the type and severity of the injury with the addition of the need to evaluate for and treat any additional occult injuries (Table 95.4) and make a report to CPS.
CLINICAL PEARLS AND PITFALLS
• Skin is the most commonly injured body organ in physical abuse.
• Accidental bruising is very uncommon in young nonmobile infants.
• Bruises may be the only external sign of injury in abuse victims with serious internal injuries.
• Bleeding disorders and other medical diseases should be considered in the differential diagnosis of cutaneous findings suspicious for abuse.
• The majority of burns in children result from accidental trauma.
• A high percentage of genital/perineal scald burns in children <2 years old are abusive.
Current Evidence
Cutaneous injury, and bruising in particular, is the most common injury identified in young victims of physical abuse. Cutaneous injuries such as bruising can be the only outward sign of more serious abusive injuries including fractures and abusive head trauma (AHT). Abusive bruising is a frequent precursor to more serious forms of physical abuse including AHT.
Clinical Considerations
Clinical Recognition
Bruises. The age and developmental stage of the child as well as the distribution and pattern of injuries can help to distinguish abusive from accidental bruises (Table 95.2). Young nonmobile infants infrequently sustain accidental bruises during routine daily activities. Therefore, any
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







