Chapter 38 Chest Trauma
The most common cause of chest trauma is motor vehicle crashes (MVCs). Acts of violence, falls, blast injuries, and pedestrian versus automobile collisions are other etiologies of chest injuries. Chest or thoracic injuries can be categorized as immediately life-threatening, potentially life-threatening, or non–life-threatening (Table 38-1).
TABLE 38-1 CLASSIFICATION OF CHEST TRAUMA
| IMMEDIATELY LIFE-THREATENING CHEST INJURIES | POTENTIALLY LIFE-THREATENING CHEST INJURIES | NON–LIFE-THREATENING CHEST INJURIES |
|---|---|---|
| Tension pneumothorax | Aortic disruption | Simple pneumothorax |
| Cardiac tamponade | Blunt cardiac trauma (cardiac contusion) | Rib fracture |
| Open pneumothorax | Pulmonary contusion | Sternal fracture |
| Massive hemothorax | Tracheobronchial disruption | Clavicular fracture |
| Flail chest | Diaphragmatic tear | Scapular fracture |
| Esophageal disruption |
In any trauma patient, rapid initial assessment and identification and treatment of life-threatening conditions are immediate priorities; many life-threatening conditions are a result of chest trauma. Table 38-2 lists some abnormal findings on initial assessment and the life-threatening conditions to be considered and ruled out. See Chapter 35, Assessment and Stabilization of the Trauma Patient, for a detailed discussion of the approach used with any trauma victim.
TABLE 38-2 ABNORMAL ASSESSMENT FINDINGS RELATED TO LIFE-THREATENING CHEST INJURIES
| ASSESSMENT FINDING | POSSIBLE INJURY OR CAUSE |
|---|---|
| Breathing | |
| Unequal breath sounds, unequal chest expansion | Pneumothorax |
| Hemothorax | |
| Foreign body obstruction | |
| Misplacement of endotracheal tube | |
| Tension pneumothorax | |
| Paradoxical chest movement | Flail chest |
| Chest wall wound | Open (“sucking”) chest wound |
| Subcutaneous air | Tracheobronchial disruption |
| Bowel sounds auscultated in chest | Ruptured diaphragm |
| Circulation | |
| Signs of shock | Massive hemothorax |
| Tension pneumothorax | |
| Aortic disruption | |
| Cardiac tamponade | |
| Muffled heart sounds | Cardiac tamponade |
| Jugular venous distension, elevated central venous pressure | Cardiac tamponade |
| Tension pneumothorax | |
| Difference in blood pressure in arms | Incomplete aortic transection |
Immediately Life-Threatening Chest Injuries
Tension Pneumothorax
Signs and Symptoms
• Severe respiratory distress: dyspnea, restlessness, and tachypnea
• Signs of decreasing cardiac output: tachycardia, hypotension, poor peripheral perfusion, cyanosis, and restlessness
• Jugular vein distension because of mediastinal shift and “kinking” of the great vessels
• Deviated trachea, away from the affected side (points to the “good” lung) and possible mediastinal deviation
• Hyperresonance with percussion of chest wall on affected side
• Symptoms such as jugular vein distension, tracheal shift and cyanosis will become increasingly worse as the condition worsens, and the patient may show signs of continued hypoxic deterioration such as decreasing levels of consciousness.
Diagnostic Procedures
• Clinical findings may indicate need for needle decompression (see “Therapeutic Interventions” below) of the affected lung before performing specific diagnostic procedures, such as a chest radiograph
• Chest radiograph: tracheal deviation and mediastinal shift may be evident (Fig. 38-1)
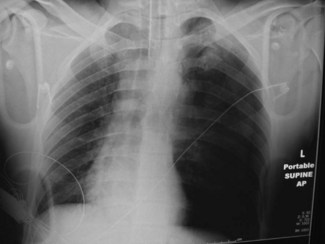
Fig. 38-1 Tension pneumothorax seen in intubated patient.
(From Marx, J., Hockberger, R., & Walls, R. [Eds.]. [2009]. Rosen’s emergency medicine [7th ed.]. St. Louis, MO: Mosby.)
Therapeutic Interventions
• Support the patient’s airway, breathing, and circulation; administer supplemental oxygen.
• Perform immediate needle decompression if severe hemodynamic compromise is present.
• Prepare for immediate chest tube insertion.
Cardiac Tamponade
Cardiac tamponade is the collection of blood or blood clots in the pericardial sac; the accumulating blood exerts pressure on the heart, limiting ventricular filling and decreasing cardiac output. The decrease in cardiac function is directly related to both rate and amount of fluid accumulation. If accumulation is rapid, as little as 100 to 150 mL of blood in the pericardial sac can adversely affect cardiac output. The leading cause of cardiac tamponade is penetrating chest injuries (80% to 90%) such as stab wounds.1
Signs and Symptoms
Diagnostic Procedures
• Electrocardiogram (ECG) may show:
• Chest radiograph may be normal initially; possibly widened mediastinum or enlarged heart shadow
• Focused Assessment with Sonography for Trauma (FAST) during the primary and secondary assessments has a significant false negative rate
• Chest computed tomography (CT) scan if patient is hemodynamically stable
Therapeutic Interventions
• Support airway, breathing, and circulation; administer supplemental oxygen.
• Rapid infusion of intravenous fluids to increase cardiac filling pressures.
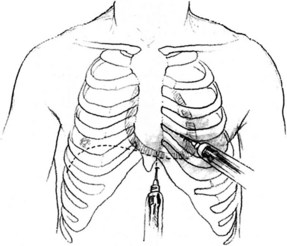
• In the hemodynamically unstable patient, needle pericardiocentesis may be needed to temporarily decompress the heart, “buying time” for transfer to the operating room or tertiary center (Fig. 38-2).
Open Pneumothorax
If a penetrating chest wound communicates with the plural space, room air enters the thorax and normal negative intrathoracic pressure is lost. As with a closed pneumothorax, the lung on the affected side collapses. Air continues to enter and exit the chest cavity through the wound as the patient breathes, producing a “sucking” sound. If the chest wound is approximately two thirds the diameter of the trachea, air may preferentially enter the plural space with inspiration rather than via the patient’s upper airways. This situation results in severe hypoxia and hypercapnea.3
Signs and Symptoms
• History of penetrating chest trauma; visible chest wound (may be as small as an ice pick hole)
• Signs of respiratory distress: dyspnea, tachypnea, restlessness, and cyanosis
• “Sucking” sound heard with respiration
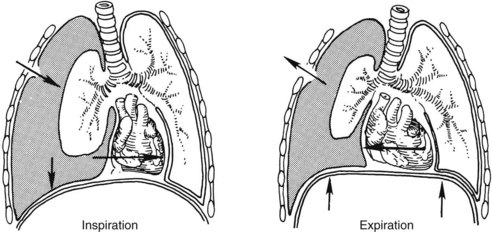
• Asymmetric chest expansion (Fig. 38-3)
• Bubbling of blood around a chest wound with exhalation. Subcutaneous emphysema may also develop
Therapeutic Interventions
• Support airway, breathing, and circulation; administer supplemental oxygen.
• Immediately cover the wound with an occlusive dressing taped on three sides.
Taping the occlusive dressing on three sides creates a flutter valve effect with an open pneumothorax. As the patient breathes in, the dressing prevents air from entering the pleural space; on exhalation, air is allowed to escape through the open end of the dressing thus preventing the development of a tension pneumothorax.3
• Observe patient closely for development of tension pneumothorax (increasing respiratory distress, jugular venous distension, hypotension). If tension pneumothorax occurs, remove dressing immediately to relieve tension.
Hemothorax
Hemothorax is the accumulation of blood in the pleural space and may result from either blunt or penetrating trauma (Fig. 38-4). Often accompanied by a pneumothorax, bleeding is the result of laceration of the intercostal vessels or internal mammary arteries, or from direct lung parenchymal damage. Massive hemothorax results from the rapid accumulation of more than 1500 mL of blood in the chest cavity and leads to respiratory and circulatory failure.

Fig. 38-4 Hemothorax.
(From Adam, A., & Dixon, A. K. [Eds.]. [2008]. Grainger & Allison’s diagnostic radiology [5th ed.]. Philadelphia, PA: Churchill Livingstone.)
Signs and Symptoms
Therapeutic Interventions
• Support airway and breathing; administer supplemental oxygen.
• Restore circulating blood volume with intravenous crystalloids and blood products.
• Assist with chest tube placement.
• Consider autotransfusion (Table 38-3).
• Prepare for emergent surgery if initial drainage is more than 1500 mL or initial drainage of 1000 mL is followed by 200 mL per hour for 2 to 4 hours.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree