INTRODUCTION
CHEST AND ABDOMINAL TRAUMA: TRAUMATIC ASPHYXIA
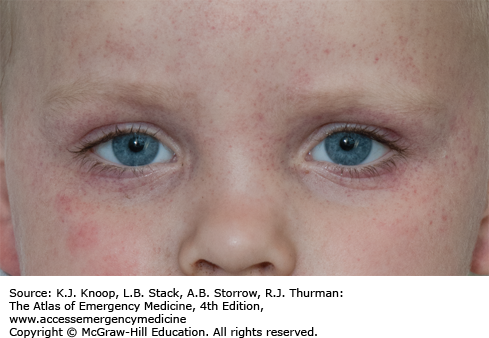
The clinical findings of traumatic asphyxia are due to a sudden increase in intrathoracic pressure against a closed glottis. The elevated pressure is transmitted to the veins, venules, and capillaries of the head, neck, extremities, and upper torso, resulting in capillary rupture. Strangulation and hanging are common mechanisms. Survivors demonstrate plethora, ecchymoses, petechiae, and subconjunctival and retinal hemorrhages. Severe injuries may produce central nervous system injury with blindness, seizures, posturing, and paraplegia.
Treatment is supportive, with attention to other concurrent injuries. Long-term morbidity is related to the associated injuries.
Facial petechiae are known as Tardieu spots.
One should be alert for associated rib and vertebral fractures.
Perthes syndrome is traumatic asphyxia following thoracic crush injury.
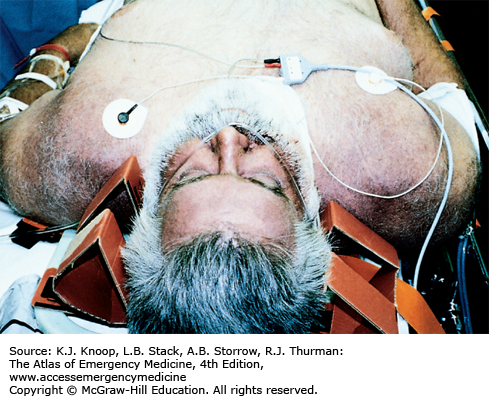
FIGURE 7.1
Traumatic Asphyxia. This 45-year-old man was pinned when the truck he was working under fell on his chest. He was unable to breathe for 3 to 4 minutes until his coworkers rescued him. The violaceous coloration of the shoulders, face, and upper chest is apparent. (Photo contributor: Stephen W. Corbett, MD.)
FLAIL CHEST
A flail chest occurs when multiple rib fractures allow a section of the thoracic cage to move independently. The negative inspiratory pressure created by the diaphragm is less effective since the flail segment paradoxically moves in, creating problems with adequate ventilation. Pulmonary contusion, hemothorax, pneumothorax, and great vessel injuries frequently accompany a flail chest.
Pain control and pulmonary toilet are initial standard therapy. Mechanical ventilation should be reserved for those with respiratory compromise, not simply as a mechanism to stabilize the flail segment. Treatment of underlying pulmonary injuries and intensive care unit admission are required for these critically ill patients.
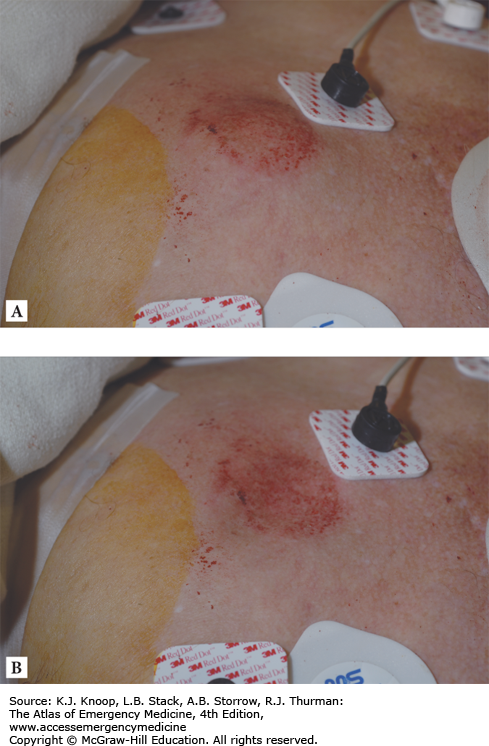
FIGURE 7.5
Flail Chest. Localized blunt trauma to the left anterior chest 4 cm inferior to the midclavicle, with resultant flail segment. Positive intrathoracic pressure (A) and negative intrathoracic pressure (B) demonstrate the paradoxical movement of the flail segment. (Photo contributor: Lawrence B. Stack, MD.)
Intercostal nerve blocks may help provide adequate analgesia so that pain does not prevent the patient from ventilating adequately.
Continuous positive airway pressure (CPAP) with patient-controlled analgesia may be as effective as mechanical ventilation.
Paradoxical movement of the flail segment is seen during the respiratory cycle in flail chest. As the rib cage expands with inspiration, the flail segment sinks into the chest. As it contracts in expiration, it balloons outward.
FIGURE 7.6
Flail Chest: Trauma Chest X-Ray. Fractures in two places of left ribs 3 and 4 result in a flail segment. Ribs 2 and 5 have single fractures. This is the chest x-ray of the patient in Fig. 7.5. (Photo contributor: Lawrence B. Stack, MD.)
FIGURE 7.7
Flail Chest: Chest CT Scan. A flail segment is seen of the left anterior chest on an axial cut of this chest CT scan. A chest tube is seen in the left pleural space. Subcutaneous emphysema is seen in the area of the fractures and tracking posteriorly. This is the chest CT of the patient in Fig. 7.5. (Photo contributor: Lawrence B. Stack, MD.)
STERNOCLAVICULAR DISLOCATION
Dislocations of the sternoclavicular joint (SCJ) are uncommon due to the strength of the supporting ligaments. Anterior dislocations are nine times more frequent than posterior dislocations. Posterior dislocations are clinically more important due to the potential for injury to underlying structures. SCJ dislocations typically occur from motor vehicle crashes and sports injuries. Examination findings of an anterior SCJ dislocation include tenderness and prominence of the proximal clavicle from the sternum. The arm is often held in adduction. Posterior SCJ dislocations may be more difficult to identify, as frequently they are associated with multiple injures. Pain and depression of the medial clavicle relative to the sternum may be seen. Superior and inferior dislocations may also be seen. CT scan through the SCJ is the best diagnostic study to evaluate this injury.
Orthopedic follow-up is required. Closed reduction of anterior SCJ dislocations is performed by placing the patient supine with a sandbag between their shoulders and placing downward pressure directly over the clavicle. A figure-of-eight clavicle harness is applied. Recurrence is common. Closed reduction of posterior SCJ dislocations may be attempted by an orthopedic surgeon by placing a towel clip around the medial clavicle and pulling the clavicle forward. Open reduction is often necessary.
While typically it requires a tremendous force to cause an SCJ dislocation, spontaneous dislocations have been reported.
In the apical lordotic radiograph (serendipity view), the clavicular head will be higher than the unaffected side in anterior and lower than the unaffected side in posterior dislocations.
One-fourth of posterior SCJ dislocations result in mediastinal injury; they always require reduction.
CLAVICLE FRACTURE
Clavicle fractures are common and are classified by location into proximal, middle, and distal thirds. Most clavicle fractures occur in the middle third. Point tenderness and contusion typically overly the fracture site. Deformity is often seen. Proximal fractures are least common and require significant force, and, therefore, they may have underlying life-threatening mediastinal injuries. Displaced distal clavicle fractures suggest injury to the coracoclavicular and acromioclavicular (AC) ligaments requiring orthopedic follow-up.
Most clavicle fractures are identified on an AP view of the shoulder. A 45-degree AP cephalad view maybe helpful if AP films are normal and suspicion is high for fracture. A contrast-enhanced chest CT should be performed if a proximal fracture is identified, looking for mediastinal injuries. Nonoperative management using a simple sling, analgesics, and ice is adequate for most injuries. Orthopedic consultation is indicated for any medial fracture, tenting of the skin, fractures with 100% displacement, severely comminuted, and for displaced distal third fractures.
Tenting requires closed reduction or surgical repair.
Stress radiographs (weighted views) help differentiate minimally or nondisplaced distal third fractures from an AC joint separation.
Glenoid neck fracture plus a clavicle fracture represents a “floating” shoulder and requires urgent orthopedic consultation.
Sixty percent of childhood clavicular fractures are nondisplaced.
FIGURE 7.9
Clavicle Fracture. This 12-year-old boy complains of pain, tenderness, and deformity over the mid left clavicle after an injury incurred during football drills. A “kick-stand” injury is seen on plain films (see Fig. 7.11). Fracture, though overriding, healed without reduction. (Photo contributor: Lawrence B. Stack, MD.)
TENSION PNEUMOTHORAX WITH NEEDLE THORACENTESIS
A tension pneumothorax results when air enters but does not exit the pleural space. Air in the pleural space accumulates and compresses the ipsilateral lung and vena cava, with a rapid decrease in cardiac output. The contralateral lung may suffer ventilation/perfusion mismatch. Subcutaneous air, tracheal deviation, jugulovenous distention (JVD), and diminished or hyperresonant ipsilateral breath sounds can be clues. Subcutaneous emphysema may be visible on the neck and chest radiographs and is easily diagnosed by palpation. The released air from a tension pneumothorax can be heard escaping from a needle thoracostomy.
Treatment requires rapid recognition of the tension pneumothorax, frequently without benefit of chest radiographs. A 14-gauge or larger needle should be placed over the superior rib surface of the second interspace in the midclavicular line. A rush of air with improvement of vital signs confirms the diagnosis. If there is no immediate improvement, do not hesitate to place a second needle in the next interspace. A chest tube should be placed immediately.
Do not overventilate patients with obstructive pulmonary disease. “Stacking” breaths trap air in the lungs and predispose to bleb rupture and pneumothorax. The pathophysiology of this disease requires a prolonged expiratory phase.
The diagnosis of a tension pneumothorax should be made clinically and treated immediately with needle thoracostomy and tube thoracostomy.
Tension pneumothorax may be a consequence of positive pressure ventilation in patients with undetected pneumothorax and a persistent air leak such as bronchopleural fistula.
Tension pneumothorax is a treatable cause of pulseless electrical activity (PEA).
FIGURE 7.12
Tension Pneumothorax. A 35-year-old man with severe asthma suffered respiratory arrest during transport by ambulance. He was intubated on arrival but soon became hard to ventilate and developed subcutaneous emphysema followed by hypotension. Needle thoracostomy produced a rush of air and bubbling from the needle with stabilization of vital signs. (Photo contributor: Stephen W. Corbett, MD.)
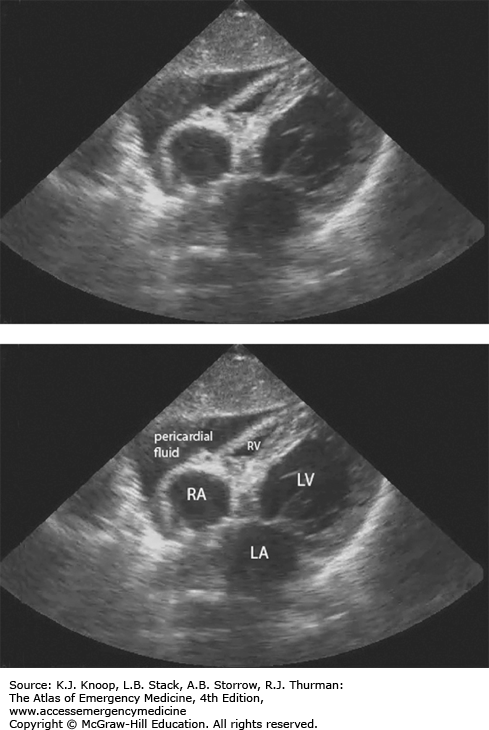
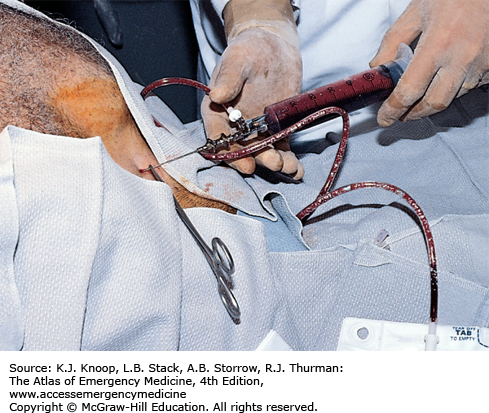
CARDIAC TAMPONADE WITH PERICARDIOCENTESIS
Beck’s triad of acute cardiac tamponade includes JVD from an elevated central venous pressure (CVP), hypotension, and muffled heart sounds but is present only 10% to 40% of the time. JVD may not be seen in hypovolemic states such as trauma. The simultaneous appearance of all three physical signs is a late manifestation of tamponade and usually seen just prior to cardiac arrest. Symptoms include shortness of breath, orthopnea, dyspnea on exertion, syncope, and symptoms of inadequate perfusion. Causes include trauma (especially penetration wounds), malignancy, hypothyroidism, uremia, myocardial or aortic rupture, and pericarditis. Rapid filling of the pericardial sac (50-100 mL) is more likely to cause compromise.
The clinical diagnosis of tamponade requires suspicion and a careful evaluation of the signs and, when available, imaging techniques. Bedside ultrasonography provides rapid diagnosis and facilitates pericardiocentesis. Goals of emergency department (ED) pericardiocentesis include identification of pericardial effusion and removal of blood or other fluid from the pericardial space to relieve the tamponade.
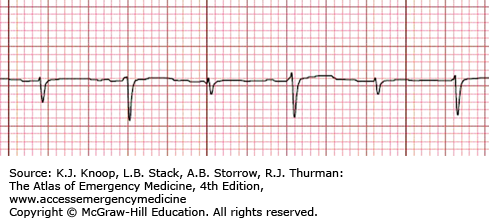
Electrical alternans seen on a 12-lead electrocardiography (ECG) suggests pericardial effusion.
Cardiac tamponade may cause a narrow pulse pressure, pulsus paradoxus (loss of palpable pulses on inspiration), and low-voltage ECG.
Ultrasonographic identification of pericardial fluid in patients with penetration chest trauma may lead to lifesaving pericardiocentesis or thoracotomy.
Cardiac tamponade is a treatable cause of PEA.
EMERGENCY DEPARTMENT THORACOTOMY
ED thoracotomy is a resuscitative procedure performed in patients with penetrating chest trauma, who have lost signs of life in the presence of prehospital or ED personnel. Thoracotomy in the ED has specific goals once the chest is opened: relief of cardiac tamponade, support of cardiac function (internal cardiac compressions, cross-clamping the aorta to improve coronary perfusion, and internal defibrillation), and control of hemorrhage from the heart, pulmonary vessels, thoracic wall, and great vessels.
Patients with penetrating thoracic trauma who lose their vital signs on arrival or have unstable vital signs despite resuscitation should receive an immediate thoracotomy in the ED. Survival rates following ED thoracotomy for penetrating trauma are 9%; stab wounds fare much better than gunshot wounds. Patients with blunt trauma who lose their vital signs en route to the ED should not undergo an ED thoracotomy, since they rarely survive. Surgical support should be obtained as soon as possible.
Injuries potentially responsive to ED thoracotomy include cardiac tamponade, pulmonary parenchymal and tracheobronchial injuries, large-vessel injuries, air embolism, and penetrating heart injuries.
ED thoracotomy should be performed immediately once the indications have been met, since the likelihood of survival is greater when this is performed earlier in the resuscitation.
Stab wounds and measurable ED vital signs are the best predictors of survival.
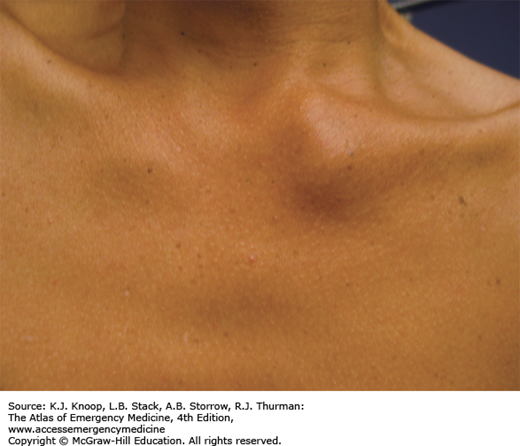
SEAT BELT INJURY
Two- and three-point seat belt restraints have reduced mortality and the severity of trauma due to motor vehicle crashes; however, they occasionally produce injury. Lap/shoulder belts are known to produce abdominal (most common), thoracic, and spinal injuries. The “seat belt sign,” abrasions or ecchymoses to the neck, chest, and abdomen in the pattern of the belt, occurs in less than 20% of patients, but is associated with a four-fold risk of intrathoracic and an eight-fold risk of intra-abdominal injury.
Patients with a mechanism for significant trauma or with other injuries requiring admission need to undergo a careful search for related injures. Patients discharged home from the ED should be given appropriate precautions to monitor for a delayed injury presentation.
Up to 36% of those with a seat belt sign have an abdominal injury requiring laparotomy.
Lap-belt-only passengers are more likely to have Chance fractures and small bowel injury if they have an abdominal seat belt abrasion after a motor vehicle crash.
GREY TURNER SIGN AND CULLEN SIGN
Bluish to purplish periumbilical discoloration (Cullen sign) and flank discoloration (Grey Turner sign) represent retroperitoneal hemorrhage that has dissected through fascial planes to the skin. Retroperitoneal blood may also extravasate into the perineum, causing a scrotal hematoma or inguinal mass. This hemorrhage may represent a hemodynamically significant bleed.
Cullen sign and Grey Turner sign are most frequently associated with hemorrhagic pancreatitis and are seen in 1% to 2% of cases, and typically are seen 2 to 3 days after onset. These signs may also be seen in ruptured ectopic pregnancy, severe trauma, leaking or ruptured abdominal aortic aneurysm, coagulopathy, or any other condition associated with bleeding into the retroperitoneum.
Treatment of patients with Grey Turner sign or Cullen sign depends on the etiology. Because the hemorrhage may represent a hemodynamically significant bleed, cardiovascular stabilization after airway stabilization is of the utmost importance. Once the patient has been stabilized, the source of bleeding can be elicited by selected laboratory tests (complete blood cell count, amylase, lipase, human chorionic gonadotropin, and diagnostic studies [ultrasound, computed tomography]). Because of the severity of diseases associated with Grey Turner and Cullen signs, these patients are usually admitted to the hospital.
Mortality rate in patients with Cullen or Grey Turner sign may be as high as 37%.
These signs are typically seen 2 to 3 days after the acute event.
These signs are seen in only 1% to 2% of patients with hemorrhagic pancreatitis.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree