Vulnerable Groups: A Summary of Relevant Concerns: Introduction
In the setting of bioterrorism, the medical and public health community must be prepared in advance to address the unique needs of vulnerable groups, including children, pregnant and breast-feeding women, the elderly, and the immunocompromised. Vulnerabilities may derive from medical, social, or economic conditions, each of which impacts the planning and response to any BCN events. Virtually all bioterror education, training, and outreach has focused largely on hospitals and emergency response and done so with the general population in mind. Preparation must also include consideration of those individuals and groups whose ability to withstand, respond, or survive BCN terror is modified by age, developmental or chronologic age, co-morbidities, or social standing. This chapter briefly summarizes these considerations, although each is also included in each agent specific chapter. The information in this chapter, drawn from historical experiences, is largely based on our current understanding of and extrapolation from physiological principles, toxicologic and animal studies, and not a small amount of common sense.
Children
As outrageous as it may seem to most of us, terrorists have been more than willing to attack targets where injury and death of children are very likely to occur. It is also the case that pediatric experience with Category A bioweapons is limited so that guidance regarding unique susceptibilities in children is based on a general appreciation of children’s unique physiologic, developmental, and social differences, extrapolation from animal studies, and general principles.
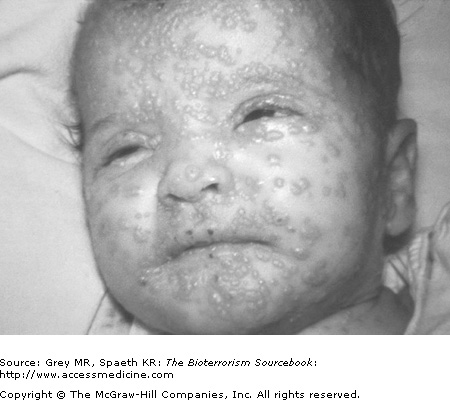
Children’s organ systems physiologically differ from adults in ways that have specific relevance to BCN agents. First and foremost, children have smaller bodies and body weights. Consequently, doses that might not affect adults may induce illness in children (Fig. 6–1). In quite specific ways, their physical stature can be a risk factor in and of itself. For example, being closer to the ground puts them at risk for inhalation exposures, particularly from chemical weapons that are often more dense than air. Further, they have increased respiratory rates and more permeable skin and blood–brain barriers providing opportunities for enhanced absorption of chemical and biological agents. Children have more immature neurologic and immune systems and so may be more vulnerable to infectious agents or to complications of chemical agents. For example, children who develop smallpox demonstrate more neurologic symptoms than adults do, including delirium, seizures, and coma. Their increased surface area-to-volume ratio and smaller volume reserves make children at risk for dehydration caused by gastrointestinal toxins or hypothermia as a result of decontamination procedures. Children will often show clinical effects at far smaller doses or intensity exposures compared to adults. Childhood lead poisoning comes to mind as a relevant analogy. Neurodevelopmental abnormalities occur at much lower blood lead levels in children than in adults. Children’s developmental state may have a disproportionate impact on their reaction to bioterrorism events, including the loss of parents or other caregivers, social isolation resulting from public health measures such as quarantine, and greater likelihood of PTSD following any significant life trauma. Caregiving adults may be called away to dangerous and unknown environments in order to respond to an emergency (health care workers, emergency response, and first responders), and they or members of their family may be forced into isolation or quarantine as a result of exposure to index cases or occupational risks. All of these possibilities may disproportionately and adversely affect children.
There are important systems issues that are often underappreciated as well. First responders are often affected emotionally when called to a scene with pediatric injuries. Treatments are often modified when a child is involved and overall experience is more limited. In the setting where a BCN attack may be involved, bulky and restrictive protective equipment, fear of the unknown, and worries about their own children and family may clearly impact the skill with which resuscitation, treatment, and triage are undertaken by individuals working under conditions of enhanced stress. Pediatric wards and specialized children’s hospitals will be overwhelmed in the setting of a mass casualty bioterrorism event. National planning does not yet include detailed preparation for surge capacity in the case of pediatric casualties.