Clinical Vignette
One of your patients is a newly minted volunteer firefighter in a rural community in Colorado. That morning he was called to a metal finishing plant where a chemical accident, involving hydrochloric acid and cyanide salts occurred. Fearing that the HCl might interact with the CN−, the area surrounding the plant was evacuated. The local hazmat team entered the area wearing SCBA gear and chemically protective clothing.
Your patient did not enter the building, but complained of feeling tired, dizzy, and short of breath in the building’s parking lot and was told to seek medical attention. In your office, he denies any headache, coughing, or GI complaints. No other firefighters complained of any symptoms. His physical exam was unremarkable: specifically no tachycardia, tachypnea, or flushing. Your differential diagnosis includes mild cyanide toxicity or possible anxiety reaction. What tests, if any, would you order?
Background
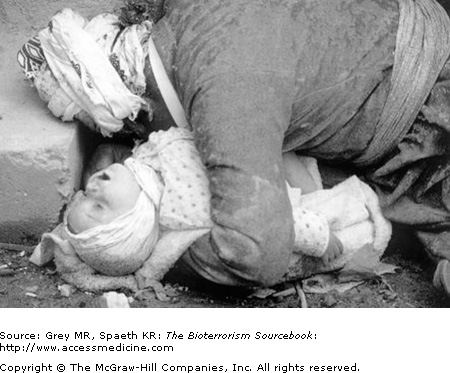
Cyanide has been used for thousands of years in intentional poisonings, though it wasn’t until the end of the 18th century that the actual compound was identified. Its role in infamy is unquestionable with such uses by Nero to murder his family and “friends,” by Reverend Jim Jones in Guyana for a mass cult suicide of over 900 people in 1978, and in the 1982 Tylenol contamination episode in which seven people died. More recently, Iraqi military used cyanide gas as part of the Iraqi chemical attack on Kurdish citizens, killing thousands in the late 1980s (Fig. 26–1).
Hydrogen cyanide (HCN) is a byproduct of the combustion of molecules containing carbon and nitrogen, including most plastics. HCN is felt to be a major cause of inhalational injury from residential and commercial fires. Worldwide, probably the single biggest source of cyanide exposure comes through cigarette smoking.
Cyanide (CN−) itself is omnipresent in living things. In fact, cyanide is naturally occurring in relatively low levels in many plants as well as in plant foods; such as corn, spinach, lima beans, cherries, soy, tapioca, peaches, bitter almonds, and cassava beans (Fig. 26–2). It is even produced by certain species of bacteria, fungi, and algae and is an important and vital part of many metabolic processes such as in the making of vitamin B12. Cyanide becomes toxic beyond a certain threshold of exposure. Because of the biological ubiquity of cyanide, there are intrinsic metabolic pathways for its removal. However, exposure levels at sufficiently high levels can readily overwhelm normal clearance mechanisms.
Cyanide is also a byproduct of a number of industrial and commercial processes including metallurgy and mining, organic chemical production, and photographic development. It is found in vehicle exhaust, in some pesticides, and commonly in combustion products. The result of all of this is that there is a presence of cyanide in the natural and industrial environments, which means some degree of exposure is probably more common than we realize.
As a chemical weapon, cyanide was first used during WWI by the French. The Nazis used a form of cyanide gas, known as Zyklon B, in the concentration camps systematically killing millions of Jews and other “undesirables” (Fig. 26–3). In the 1980s, cyanide gas is believed to have been used by Saddam Hussein both against the Kurds in Northern Iraq and against Iran during the Iran–Iraq War. It is still used as a method of capital punishment in some places.
The term blood agent came out of WWI as a way of differentiating the effects of cyanide gas from other gases at the time, which all had specific target organs: skin, eyes, or lungs, whereas cyanide, it was thought, affected primarily the blood.
Sources
Cyanide is a naturally occurring chemical that is present in a variety of food sources, soil, and water. Industrial exposures occur through metallurgical, iron and steel mills, electroplating, gold refining, photochemical manufacturing processes, plastics, fumigants, and mining. It is used as an industrial intermediate and as a byproduct in chemical industries. Environmental sources of CN− include cigarette smoke, vehicle exhaust, and biomass burning. Cyanide is commonly present as waste, and many hazardous waste sites have cyanide in both the soil and in water runoff. Firefighters are at particular risk given the ubiquity of cyanide in building materials.
Physical Properties
Cyanide is likely to be disseminated via bomb or aerosolization. It is stored as a colorless liquid but is extremely volatile so that, once released, it almost entirely vaporizes. Because it has such low persistence, cyanide vapor rather than liquid is the major threat. Although there is a characteristic description of cyanide smelling like “bitter almonds,” this is only so for the hydrogen cyanide form. Even then it is not a reliable means of identifying the gas; only 50% of people can detect it even under ideal environmental conditions.
Pathophysiology
Cyanide’s most important toxicity results from inhibition of normal cellular energy metabolism. Specifically, CN− binds to the iron moiety on cytochrome oxidase, a key enzyme in mitochondrial electron transport (Fig. 26–4). This inhibition disrupts oxidative phosphorylation, shifting the cell from aerobic to anaerobic metabolism. By interrupting normal cellular oxygen utilization, adenosine triphosphate (ATP) production comes to a halt and the ATP/ADP ratio declines, choking off all energy-dependent cellular metabolism. The resultant histotoxic hypoxia shifts the oxygenhemoglobin dissociation curve and diminishes tissue oxygen uptake.