Clinical Vignette
A 65-year-old patient not known to you arrives in your office complaining of dyspnea, chest tightness, and burning of his nose and eyes. He appears rather dyspneic and anxious and is immediately put into an exam room. The patient reports that he had just left a major industrial fire where he had been watching firefighters attempt to control the blaze. He noticed an acrid odor in the air, and when he began coughing, he decided to leave. Within a few minutes he noticed increasing difficulty breathing, and seeing your office, he pulled in to request urgent evaluation. His past medical history is significant only for childhood asthma. He specifically denies any foreign travel and has never been a smoker. On exam, he is tachypneic and tachycardic; you hear wheezes but no crackles. His pulse oximetry finds an SaO2 of 88%. You immediately call for an ambulance. What should you tell the emergency room?
Background
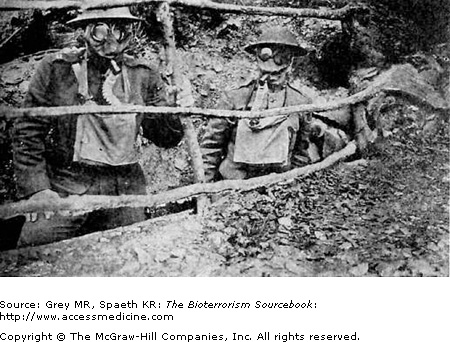
On April 22, 1915, the German army released over 150 tons of chlorine gas downwind toward British and Canadian troops at the Battle of the Marne in Ypres, France (Fig. 23–1). Of the 7,000 soldiers present at the front that day, 5,000 suffered injury or death (see Of Note . . box below). The modern era of chemical weapons had begun. Later that same year on the very same battlefront, the German army released phosgene gas, with far more deadly effects. Further development of chemical weapons proceeded throughout the war, prompting continuous refinement and development of field protective gear in order to limit casualties (Fig. 23–2). The devastating effect of chemical weapons during WWI mobilized the international community and prompted the League of Nations in 1918 to institute the first international treaty to ban chemical weapons. Relative to the most potent nerve agents, pulmonary agents are easy to make and inexpensive to buy. Chlorine and phosgene, two agents first introduced as chemical weapons in WWI, are still available commercially and are used widely in plastics, rubber, and dye industries worldwide. Industrial or transportation accidents with these agents are much more likely to occur than deliberate releases, but their potential as chemical weapons must be considered.
April 22, 1915, Yypres, France
We knew there was something wrong. We started to march towards Ypres but we couldn’t get past on the road with refugees coming down the road. We went along the railway line to Ypres and there were people, civilians and soldiers, lying along the roadside in a terrible state. We heard them say it was gas. We didn’t know what the hell gas was. When we got to Ypres we found a lot of Canadians lying there dead from gas the day before, poor devils, and it was quite a horrible sight for us young men. I was only twenty so it was quite traumatic and I’ve never forgotten nor ever will forget it.
Private W. Haye
Royal Scots
Properties
A wide variety of chemical agents damage lung tissues and have the potential to be used as pulmonary agents. Tissue damage is driven primarily by two physicochemical properties: reactivity and solubility. Two organohalides, phosgene (COCI2) and chlorine (CL2), are considered prototypical pulmonary agents and will be detailed for illustrative purposes.
Phosgene (Fig. 23–3) is often described as having the sweet odor of freshly cut hay; however, the odor may be faint and in general is an unreliable means of identification. Phosgene is generally stored as a liquid. At temperatures above 47°F (8.2°C), phosgene is a colorless gas that is nearly four times denser than air, and so it accumulates close to the ground. When combined with water, phosgene breaks down into hydrochloric acid and carbon dioxide. If the gas is released and there is enough ambient humidity, phosgene would have a whitish color instead of being colorless.
Chlorine (Fig. 23–4) is a greenish-yellow gas that is widely used in water purification, disinfection, and the synthesis of other chemicals (plastics, rubber, and dyes). Nearly 12 million tons are produced annually for industrial, commercial, and household use. Chlorine is 2.5 times heavier than air, a property that has relevance to its clinical effects. It is also highly reactive and has the familiar pungent, irritating odor of bleach.
Sources
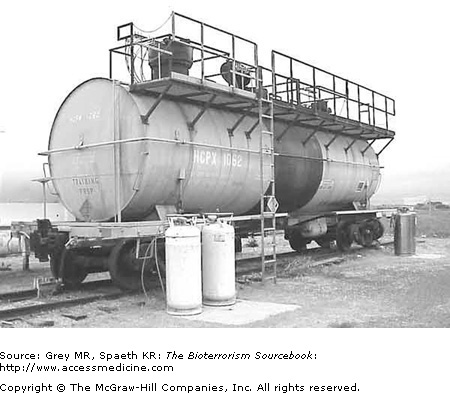
A wide range of industries produce or use pulmonary agents as chemical intermediates. For chlorine gas, these include petroleum refining, photographic processing, pulp and paper mills, sewer and waste-water treatment plants, and disinfectants (Fig. 23–5). Phosgene is a byproduct of industrial fires in which synthetic chlorinated polymers are consumed, posing a risk to firefighters and bystanders. Pesticide and pharmaceutical manufacturing are common examples in which these exposures may occur. Welders and petroleum refinery workers are also at risk. Chloropicrin is a fumigant used in agriculture, and organofluoride polymers (PFIBs such as Teflon) are used in literally dozens of industrial processes. Workers at risk include materials scientists and engineers, as well as individuals involved in plastic, polymer, resins, and elastomer manufacturing. Combustion of any of these widely used compounds may result in airborne exposures to a wide variety of pulmonary irritants, all of which may cause the characteristic pulmonary toxidrome.
Pathogenesis
For nearly all biological and chemical agents considered in this book, host and tissue factors and properties of the agents themselves provide the relevant clinical parameters that define toxicity (Table 23–1). This is certainly the case with pulmonary agents. Pulmonary agents’ toxicity is influenced by the site of action and the properties of the specific agent, in particular, water solubility and chemical reactivity. The large surface area of the lung (50–150 m2), compared to the surface area of the skin (2 m2) and eye (.0002 m2), makes the respiratory system an efficient route for chemical agent exposure. Unlike other chemical agents, however, the effects are primarily local; that is, they occur at the site of contact within the respiratory tree.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree