Case Vignette
It’s mid-February when an otherwise healthy 42-year-old stockbroker presents to your office with fever, chills, and malaise. He reports no sick contacts, no exotic travel but mentions having spent the previous weekend on a fruitful hunting trip that included shooting and trapping rabbits. CXR reveals hilar adenopathy. Your differential includes influenza, tuberculosis, sarcoidosis, histoplasmosis, and tularemia. What should you do?
Background
A gram-negative coccobacillus, tularemia was first identified in 1911 by a scientist investigating an outbreak of what was initially thought to be bubonic plague in Tulare County, California. The disease has multiple means of transmission, and waterborne epidemics were seen in Europe and the Soviet Union in and around World War II (WWII). It has been suggested that the Soviet outbreak, which occurred at the Eastern front during WWII, was a result of a deliberate biological attack by the Russians. In fact, tularemia has been a favorite agent for bioweapons research since the 1930s. In 1969, the World Health Organization (WHO) estimated that 10 kg (20 lb) of aerosolized F. tularensis could infect 50,000 people, killing approximately 4,000. These numbers may be outdated because antibiotic and vaccine-resistant strains of weaponized tularemia—reported to have been developed at Biopreparat—would be far more deadly.
Francisella
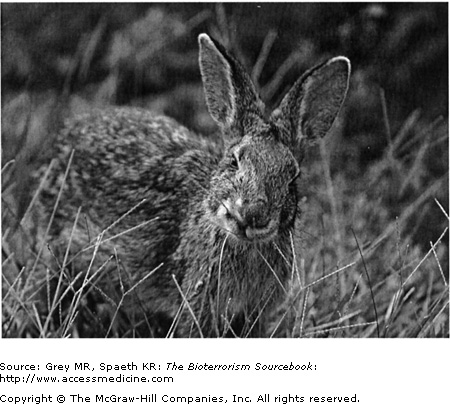
Francisella tularensis, the causative agent of tularemia, is a small, nonmotile, facultative aerobic, intracellular gram-negative coccobacilli. Tularemia grows in aerobic environments. Despite its inability to form spores, it is nonetheless quite hardy and able to persist for several weeks in water, soil, vegetation, or in animal products. F. tularensis has three different species of which biovar tularensis is the most virulent form, and it is the one most commonly seen in the United States. The organism is considered to be one of the most communicable bacterial pathogens known. Disease hosts include rabbits, rats, and other small mammals that attain the infection through direct contact or by insect vectors, such as ticks and mosquitoes.
F. tularensis is found worldwide, though global disease incidence has not been determined. Tularemia occurs sporadically throughout the continental United States, but predominantly in the rural areas of the South, Southwest, or Midwest. Since the 1990s, fewer than 200 cases are reported annually and occur in a bimodal seasonal pattern. The majority of cases are diagnosed in the summer/fall and are thought to be secondary to arthropod (tick) transmission. A smaller fall/winter peak coincides with hunting seasons. Most cases are secondary to direct contact of some kind, although there are infrequent cases of infection from inhalation. No significant differences in infection patterns are seen by age or by gender. Overall mortality rates prior to the advent of antibiotics ran between 5% and 15%, and for pneumonic forms between 30% and 60%. In the antibiotic era, overall mortality is less than 2%.
Naturally occurring tularemia is a zoonosis that traditionally infects outdoorsmen, trappers, hunters, and those handling the infected carcasses of small mammals. Veterinarians, animal control workers, butchers, and farmers are occupations at risk. Laboratory workers may inadvertently infect themselves as well. Rural dwellers, particularly Native Americans, are at increased risk as well.
Most human tularemia is tick-borne. Because infection can occur through bacterial contact with skin, mucosal linings, gastrointestinal epithelium, and the respiratory tract, humans can become infected by being bitten by infected ticks, by handling contaminated animals or animal products, by ingesting contaminated food or water, or by inhaling aerosolized bacteria. Person-to-person transmission with F. tularensis does not occur. The greatest public health threat from weaponized tularemia is as an aerosol, although other means are possible. Aerosol dispersion in a densely populated area would likely result in widespread reports of fevers and nonspecific symptoms (see following clinical description) within five days. A large percentage of these people would develop pleuritis or pneumonitis. The abrupt onset of this constellation of symptoms in large numbers or in otherwise healthy subpopulations should alert physicians and public health officials to a possible bioweapons attack.
The factors responsible for F. tularensis’s virulence are not well known. Once inoculation occurs, regardless of the site, an intense focal inflammatory response occurs. Immigration of neutrophils and other leukocytes results in a suppurative necrosis followed by granuloma formation. Pathology of the site shows a noncaseating, centrally necrotic region enclosed by epitheliod cells and multinucleated giant cells as well as fibroblasts in an array consistent with granulomatous pathology. F. tularensis survives neutrophil oxidation and is phagocytized and transported to regional lymph nodes by macrophages. Once there, the bacterium multiplies and spreads via lymphatics and blood to the kidneys, spleen, liver, and lungs. Bacteremia is detectable early in the infection. In primate studies of inhalational tularemia, peribronchial inflammation and alveolar septal inflammation occured within 72 hours of infection; later, pneumonic consolidations, granulomas, and ultimately chronic interstitial fibrosis developed. Inhalational tularemia is the bioweapon of choice and may present in the pneumonic, typhoidal, or ulceroglandular form.
Following an incubation period of anywhere between 2 to 20 days (mean 3–5 days), the abrupt onset of the following nonspecific constellation of symptoms herald the beginning of tularemia: fevers, chills, runny nose, myalgias, dry cough, headache, and prostration; hemoptysis, pleuritic pain, or dyspnea is noted. Symptoms such as nausea, vomiting, and diarrhea may be seen. As the illness progresses, anorexia, weight loss, and sweats ensue. If left untreated, these symptoms may continue for up to 4 weeks or possibly longer.
Tularemia’s clinical presentation reflects both the mode of transmission and the route of infection. The form of tularemia influences mortality, but it has little effect on treatment decisions. Regardless of the initial syndrome, infection may spread hematogenously resulting in pleuropneumonia, septicemia, and even meningitis. Tularemia sepsis is of particular concern because of its high fatality rate if untreated. Clues to septicemic tularemia include fever, diarrhea, vomiting, and abdominal pain. Further progression results in mental status changes, coma, and finally shock, DIC, ARDS, and multisystem organ failure.
Six distinct clinical syndromes have been described; however, these can exist as a continuum, and substantial syndromic overlap may present in the same individual. The six clinical syndromes are:
- 1. Ulceroglandular (80% of cases). This is the dominant naturally occurring form of tularemia and is seen when the means of transmission is from the bite of infected ticks or animals, or through direct contact with infected carcasses. Symptoms begin with fever and a solitary papular lesion—typically at the site of contact—that becomes centrally necrotic and tender within a few days and may be covered with an eschar; reminiscent of anthrax. Regional lymphadenopathy is noted several days after the papule appears (Figs. 16–2 and 16–3). Despite initiation of antibiotic therapy, lymph nodes may become progressively more fluctuant and may rupture. Pneumonia develops in 10% to 15% of patients (see discussion of pneumonic tularemia).
- 2. Glandular (10% of cases). This form (considered by some to be a subset of ulceroglandular) presents with one or more enlarged regional lymph nodes but without any cutaneous lesions or ulcerations (see Fig. 16–4).
- 3. Typhoidal (10% of cases). Generally occurring after an inhalational exposure (though it can occur from skin or mucosal contact), patients present with fever and chills but without any clear focus of infection. Patients may develop rhabdomyolysis and subsequent renal failure, sepsis, and DIC (even with apparently negative blood cultures). Pneumonia may develop, as well, and can be quite severe. Pneumonia can occur in all the forms but is most commonly seen as part of typhoidal tularemia (see later for discussion of pneumonic tularemia). The typhoidal form is distinctive in that, unlike the other forms, lymphadenopathy is absent. In the event of a deliberate attack using aerosolized F. tularensis, typhoidal tularemia would likely be a dominant form. Untreated, typhoidal tularemia has a mortality rate of roughly 35%.
- 4.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree