Clinical Vignette
Two days after returning from a short trip to Venezuala, an otherwise healthy 48-year-old male arrives at your office complaining of fever, chills, nausea, vomiting, malaise, and arthralgias. On exam he was toxic appearing febrile, and you note abdominal tenderness, icterus, and multiple erythematous papular lesions on his lower extremities. Because of his recent tropical travel, you immediately send him by ambulance to the ER. There, staff physicians suspect a case of VHF and contact the local health department. During the course of his deteriorating clinical course in the intensive care unit, the patient developed severe coagulopathy and died. Autopsy revealed necrotic portions of the liver and histologic findings consistent with yellow fever. Yellow fever antigens were noted in blood samples, and the diagnosis was confirmed by PCR. What infection control and decontamination procedures should you have followed? In this case of a febrile individual with a rash and with recent travel abroad, what is your DDX?
Background
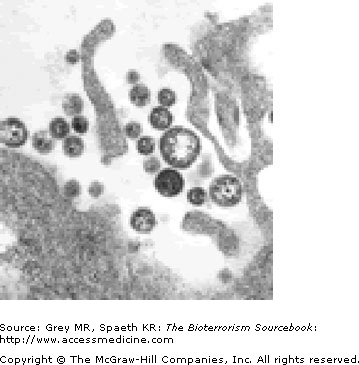
Extreme contagiousness, virulence, and mortality rates make VHFs among the most feared diseases of humankind (Fig. 13–1). Since the first documented case of a Marburg in 1967, VHFs have been identified all over the world and have observable naturally occurring outbreaks. No documented use of VHFs as bioweapons has yet occurred; however, it is commonly accepted that the United States, Russia, and probably other governments have successfully developed weaponized versions of VHFs. What is known about the epidemiology, transmission, clinical presentation, and prevention of VHFs is therefore based on naturally occurring epidemics and bioweapons research.
VHFs are caused by four distinct families of RNA viruses. Filoviridae, which includes Ebola and Marburg viruses; Arenaviridae, which include the etiologic agents of Argentine, Bolivian, and Venezuelan hemorrhagic fevers, Machupo and Lassa fever; Bunyaviridae, which includes the Congo-Crimean hemorrhagic fever virus (CCHFV) and the Rift Valley fever (RVF); and finally, Flaviviridae, which includes dengue and yellow fever viruses. With the important exception of filovirus, whose animal reservoirs are speculative, VHFs are zoonotic.
| October 2000 | The Ugandan Ministry of Health reports 176 cases of Ebola, including 64 deaths. |
| February 2001 | A Canadian physician activates the national contingency plan for viral hemorrhagic fevers (VHFs) when VHF is diagnosed in a woman returning from the Congo. |
| December 2003 | The Ministry of Health of the Republic of the Congo reported a total of 35 cases, including 29 deaths from Ebola. |
| March 2005 | CDC confirms that VHF outbreak in Angola is Marburg. A total of 124 cases, with 117 fatalities, was reported. |
September 2004: A Case of Lassa Fever in New Jersey
A businessman returning from a 4-month trip to Sierra Leone in West Africa was hospitalized in New Jersey complaining of several days of fever, chills, severe sore throat, diarrhea, and back pain. He began feeling ill just before his return to the U.S. On admission, the patient was febrile to 103.6°F (39.8°C), but alert and oriented. Due to his recent travel—which included plane rides from Africa to London to Newark, and a train ride to his home—he was placed on antimalarial and antibiotic treatments to cover the possibility of malaria or typhoid fever. Nonetheless, he developed ARDS and required mechanical ventilation. The DDx was broadened to include VHFs, specifically yellow fever and Lassa fever. Attending physicians contacted the state health department and the CDC. Under an investigational new drug protocol he was placed on IV ribavirin, but the patient died before the medication was administered. Serum antigen testing confirmed the diagnosis of Lassa fever as did additional testing, including postmortem liver immunohistochemical stains, cell culture viral isolates, and PCR testing.
Subsequent epidemiologic investigation identified 188 individuals who had contact with the patient during the period he was considered infectious. This list included family members, 139 HCWs (42 laboratorians, 32 nurses, and 11 physicians), and an additional 16 commercial laboratory workers in two additional states. Passengers on the London to Newark flight were evaluated for exposure to Lassa virus. All exposed or potentially exposed individuals were placed in an active surveillance program whereby they were checked twice daily for the development of fever >101°F (>38.3°C) for the 21-day incubation period. None contracted the disease.
MMWR/morb mortal wkly Rpt October 1, 2004; 53(38):894–897.
Epidemiology
More than twenty naturally occurring Marburg or Ebola outbreaks affecting some 2000 individuals, mainly African, have been documented since 1967 (Fig. 13–2). Infections occurred through direct contact with infected animal or human fluid or tissue, or by needle stick infection. Percutaneous exposure is associated with a higher mortality rate. Successful aerosolization and transmission of VHFs in primates has been documented. Precise information about the nature of transmission does not exist at present because outbreaks are sporadic, subside quickly, and tend to occur in areas without adequate public health involvement. Rodents and arthropods are the vectors. There are similarities and important distinctions among the various VHFs in terms of transmissibility.
Indirect transmission of Filoviridae (Ebola, Marburg) from aerosolized animal feces, infected arthropod bites, or through contact with animal carcasses occurs. Person-to-person airborne transmission cannot be ruled out, though a number of these outbreaks have ended without airborne precautions ever being taken. Ebola has been found in significant amounts in human skin and sweat glands, and there is concern that casual contact could spread the virus. Primate studies indicate that the virus can be taken up through the mucosal lining. Transmission does not appear to occur during the incubation period (determined in primate studies to be several days).
Arenaviruses (Lassa or Machupo) infect humans through aerosols from infected rodent waste products or by contact of mucus membranes or open skin with the virus. Person-to-person transmission occurs secondary to direct contact with infected body fluid; transmission through airborne droplets cannot be ruled out in the case of Arenavirus.
The Bunyaviridae (RFV, CCHFV, Hartavirus) cause human infection through the bite from infected mosquitoes, inhalation of aerosolized virions from an infected animal, carcasses, and physical contact with infected animal tissue. There is also compelling evidence that infection can occur through consumption of infected animal milk. Presently, it is felt that no person-to-person transmission can occur despite the virus being found in oropharyngeal swabs.
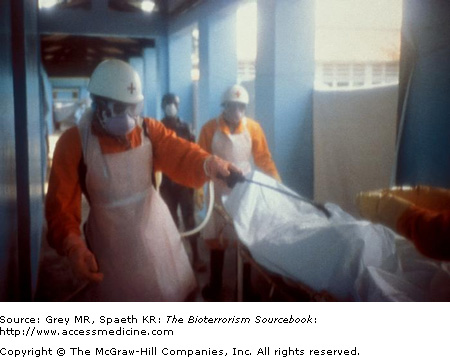
High-Risk Groups
VHFs represent a risk primarily to individuals and communities where natural reservoirs exist. Family members, HCWs, and other secondary contacts of patients with known VHF are at increased risk of acquiring the disease. Needles, syringes, and other instruments used to treat VHF patients must not be reused due to the risk of transmitting the disease to uninfected patients. Individuals involved in burial of VHF victims have acquired the disease as have those processing meat from infected livestock. HCWs, laboratorians, and individuals involved in the transport of unidentified but infected animals (especially primates) or carcasses are also at greater risk.
Pathogenesis
Basic pathophysiologic mechanisms of VHFs are not yet fully understood. As the name implies, a significant and often profound bleeding diathesis is common to all four families of VHFs. Several mechanisms, including platelet deficiency or dysfunction, direct endothelial and platelet injury, or cytokine dysregulation, have been demonstrated and vary depending on the virus family. For example, Arenaviruses cause cytokine dysregulation with resultant inhibition of platelet aggregation and thrombocytopenia, but have little or no direct cytotoxic effect. In contrast, Bunyavirus and Flavivirus are directly cytotoxic to the liver, kidney, and spleen and generate microvasculature damage.
Clinical Presentation
Naturally occurring epidemics form the basis for most knowledge of the clinical presentations of VHFs. Early clinical diagnosis is difficult due to the range and variability of signs and symptoms. The dramatic presentation of the late stages of VHFs leaves less doubt as to diagnosis. Further, distinguishing one VHF from another has less practical implication than for the other biological and chemical weapons, as treatment options are limited and infection control and public health considerations are the same. For example, ease of transmission may differ, but not to the point where the initial approach of isolation and quarantine will be affected by the form of the disease once the diagnosis of a VHF is entertained.