Clinical Vignette
You return to your office from lunch to find your office staff around the TV. A nurse states that CNN is reporting a confirmed case of smallpox in the Chechnyen Republic. You realize immediately that your office will be flooded with calls from anxious patients worried about smallpox, concerned about rashes they’ve just noticed, and demanding immediate vaccination. You go to the CDC website and confirm indeed that the first case of Variola major in over thirty years has been diagnosed and that a worldwide public health emergency looms. From the CDC website you download their fever rash algorithm and plan to meet with your staff to review the protocol. Within two hours you receive calls from your local health department and the hospital where you have admitting privileges asking you to report immediately for a planning meeting for a townwide mass vaccination clinic.
Background
Variola major is a double-stranded DNA virus of the Orthopox family. There are two recognized forms of smallpox: Variola major and Variola minor. Variola major is the more virulent strain with mortality rates 30% or higher in vaccine-naïve populations. Variola major has historically been more prevalent. Variola minor is considered rather mild with mortality rates less than 1%. Like its close relative, chickenpox, smallpox historically followed seasonal patterns of outbreaks, peaking in the late winter and early spring. Such a pattern is likely secondary to the sensitivity of the aerosol droplets to higher temperatures and humidity. It is not known what sensitivities (or lack thereof) weaponized forms might have. All Category A, B, and C biological weapons occur sporadically in nature with the exception of smallpox. Therefore, barring an extraordinary occupational history (i.e., laboratorian working in a Biosafety Level-4 (BSL-4) facility, diagnosing smallpox equates with diagnosing bioterrorism and constitutes an international medical emergency of the first order.
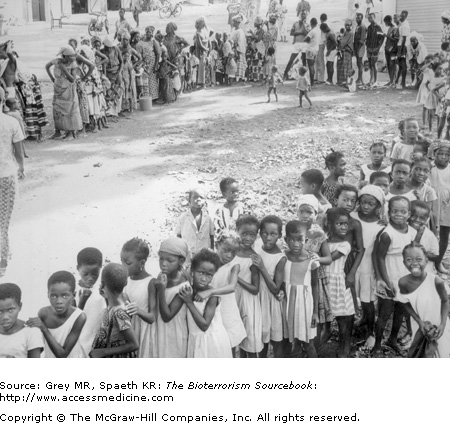
In what is one of the finest public health achievements of the 20th century, the virus that had killed more people than any other pathogen in the history of humanity was declared eradicated in 1980 thanks to a global vaccination program spearheaded by the WHO (Fig. 12–1). At that time, it was held that nations need not continue vaccination programs. It was not entirely accurate to claim the virus was eradicated as the WHO approved two sites to maintain smallpox: the CDC in Atlanta and the Institute for Viral Preparations in Moscow. Archives unearthed following the collapse of the U.S.S.R. demonstrated that the Soviets engaged in more than simple storage: they were actively developing large quantities and possibly vaccine-resistant strains of the virus that could be fitted to intercontinental ballistic missiles and bombs. The WHO called for both nations to destroy all stored viruses in 1999 and again in 2002; both declined. Reportedly, Russia continues to maintain smallpox research and active development of strains with greater resistance to standard vaccines amid reports of woefully lax security at these labs.
Smallpox and Bioterrorism
A number of factors make smallpox one of the most feared biological warfare agents. There are numerous considerations that make an outbreak likely to spread more quickly and with medical and public health consequences far more concerning now than would have been the case even thirty-five years ago.
- • Smallpox spreads easily from person to person and is transmissible through aerosols, droplets, or fomites.
- • Discontinuation of routine civilian smallpox vaccination in 1972 has left 85% of the U.S. population with no prior immunologic exposure to smallpox or to the vaccinia vaccine used to protect against the disease. Should smallpox be introduced into an immunologically naïve population and clinically naïve medical community, the risk for disease and its transmission would be enormous.
- • The loss of clinical familiarity with smallpox is likely to cause delay in recognition and diagnosis, implementation of isolation and vaccination efforts, thus allowing more time for the disease to become epidemic.
- • The world’s population is far more mobile than was the case in the early 1970s, and living conditions worldwide are more crowded.
- • Finally, new diseases (e.g., HIV/AIDS) and advances in medical care (e.g., cancer treatment and immunosuppressive drugs) mean there are far more immunocompromised individuals at risk for rapidly progressive variola.
In essence, the virulence of smallpox and communicability, along with expanded opportunities for rapid worldwide dissemination and changes in world demographics, culture, and medical standards, offer many advantages to terrorists should they obtain access to the virus.
Countering this more pessimistic view are several considerations. First, many veterans of the smallpox eradication effort, infectious disease specialists, and public health officials believe that an aggressive ring vaccination strategy, or ring vaccination followed by mass vaccination, would contain an epidemic provided multiple concurrent releases did not occur. Second, mortality from smallpox historically may have reflected poor nutritional status, coexisting infectious conditions, inadequate health care infrastructure, slower communications, and the absence of antivirals. Each of these conditions are less prevalent now than in the past and could work in favor of epidemic control.
Smallpox virus is usually inhaled and enters the mucosal lining of the oropharynx. It is then taken up by macrophages and transported to regional lymph glands where the virus multiplies, activates cytotoxic T cells and B cells, and provokes a host antibody response. On about the fourth day a subclinical viremia seeds the spleen, bone marrow, and distant lymph nodes. Day 8 signals the start of the clinical phase, heralded by a viremia-associated prodrome of fever and malaise. During this period, the virus infects the dermis and oropharynx causing the classic skin manifestations of smallpox (Fig. 12–2). As the immune response occurs, the virus is taken up by white blood cells and it is transported through the small vessels of the dermis and pharyngeal mucosa where it infects the perivascular tissues (day 14). The classic pitted scarring that is left when the scabs form are secondary to destruction of the sebaceous glands, which shrink and are replaced with granulation tissue and soon thereafter with scar tissue. The lesions in the oropharynx ulcerate the quickest because the tissue there, unlike the dermis, lacks a stratum corneum. As a result of ulcerating, oropharyngeal lesions, the saliva contains an enormous amount of virus.
Smallpox stimulates cytotoxic T-cell responses, neutralizing B-cell antibodies, and the production of interferons. These lost responses restrict viral replication and induce prolonged immunity in the patients who recover. Smallpox is more virulent in infants, the elderly, and immunologically impaired hosts, particularly those with T-cell deficits (see Vulnerable Groups).
Patients are most infective from the onset of the rash (days 8–14) until the first scab forms. At this point of infectivity drops precipitously. Infected individuals spread smallpox through aerosolized droplets from the oropharynx. Although saliva may be positive for virus up to six days prior to the onset of skin lesions, patients do not transmit the virus until visible lesions form and salivary viral content begins to peak. Infection also occurs through contact with contaminated objects, such as clothes, bedding, and surfaces, or through bodily fluids such as urine, sweat, or sputum. These facts dictate the infection control strategies outlined below. Infectivity among those in contact with a primary case is estimated to be between 40% and 80%.
According to some epidemic models, fifty people initially infected from a bioterrorist attack with smallpox would infect secondarily somewhere between 2,500 to 5,000 individuals. Each successive generation would increase the number of infected individuals 50- to 100-fold. In large part, this exponential expansion is due to the delay between exposure and onset of transmissibility, which occurs when skin lesions erupt.
Unlike other Category A agents, no naturally occurring smallpox exists. The United States and Russia are known to have smallpox stores. Given the security issues in the former Soviet Union, the possibility exists that the virus has been sold on the black market. It is also possible that heretofore unidentified sources of the virus exist elsewhere in the world, secretly contained in countries such as North Korea, France, and Iran. Other than deliberate release, for which everyone who is not vaccinated would be at risk, laboratorians and research scientists probably represent the only reasonable occupational risk groups. The last known case of smallpox in the West occurred in a lab worker in England, resulting in her death and the suicide of the research scientist whose lapse in technique was responsible for the exposure.
It is important to bear in mind that there has been no clinical or public health experience with Variola major since the mid-1970s. What is known about the clinical presentation and complications of smallpox draws necessarily on historical experience and that largely from developing nations, which may or may not be generalizable to the United States or other Western nations.
Symptoms generally begin at the end of an incubation period of between one and two weeks. At the end of this period, the patient experiences high fever sometimes with mental status changes, malaise, exhaustion, headaches, backache, and occasionally abdominal pain. A maculopapular rash will appear within three days of prodromal onset, and fever will be noted (though not as high as the prodromal fever). The rash occurs simultaneously on the oropharyngeal mucosa and the face and then spreads outward to the forearms and the legs, relatively sparing the trunk.
The synchronous development of a centrifugally spreading viral exanthum is one of the classic diagnostic clues to smallpox. This is in contrast to another orthopox virus, chickenpox or vaccinia, which begins on the trunk and face and characteristically has lesions in different stages of development. Once the rash appears, it vesiculates and then assumes firm papular pustules over a period of one week. Approximately one week after the rash begins, the lesions umbilicate and then encrustate, leaving smallpox’s signature pitted scar. Scabs are not highly infectious, although virus can be recovered from them. Patients are potentially infectious until the last scab falls off with infectivity peaking from rash onset until scab formation. The progression of a symmetric centrifugal homogeneous rash through the four stages of vesiculation, pustulation, umbilication, and encrustation is characteristic of smallpox and nothing else (Figs. 12–3 and 12–4, Table 12–1). Death from smallpox occurs usually around the second week. Encephalitis occurs infrequently, and secondary infection is surprisingly rare. Milder infections are seen in previously immunized patients.
| Pattern of Presentation | Multiple, concurrent acute cases of a febrile prodrome followed by generalized vesicular or pustular rash. |
| Features | Fever ± headache, abdominal pain, nausea/vomiting, prostration. Must have well-demarcated vesicular or pustular poxlike rash in same stage of development. Rash begins in mouth and face and moves outward to arms and legs. |
| Findings | Clinical presentation and epidemiology determine diagnosis. Must differentiate from chickenpox. Rapid PCR testing for definitive diagnosis. |
Two significant clinical variants of smallpox occur in approximately 10% of all cases and may result in delayed diagnosis. In both instances, the dermal manifestations differ while the incubation period and prodromal symptoms are unchanged from the classic presentation summarized above. In the hemorrhagic form of Variola major—for which pregnancy appears to be a risk factor—the skin becomes dull and darkly erythematous, but vesiculation and pustulation do not occur. Petechiae and frank mucosal and dermal bleeding are followed by death in virtually 100% of cases, often within 6 days of the onset of clinical symptoms. In the second variation of Variola major, known as the “flat” type, vesicles never form into the characteristically firm deep dermal papules. Instead, vesicles become confluent, flattened, and soft to the touch. Skin hemorrhages may also be seen. Presuming the patient survives, the lesions of flat smallpox leave no scar after they eventually peel away.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree