CERVICAL SPINE INJURIES IN INFANTS AND CHILDREN
Cervical spine injuries occur in 1% to 2% of all pediatric trauma patients. While the incidence of cervical spine injuries in children with trauma is lower than adults, children have higher rates of mortality (~18%) compared to adults (~10%).1 In children <8 years old, almost three quarters of all spinal injuries occur in the cervical spine,2 and nearly two thirds of these children have associated neurologic deficits and head or other major organ injury.3 In addition, spinal cord injury without radiographic abnormality (SCIWORA) may occur in children and typically involves the cervical spine. The incidence of SCIWORA among pediatric trauma patients ranges from 0.15% to 0.2%, compromising 4.5% to 35% of pediatric spine injuries.4,5,6 Motor vehicle crashes are the most common mechanism of cervical spine injuries, followed by falls, and in teenagers, diving and sports injuries. Boys are affected more often than girls. Child abuse can result in cervical spine injuries in younger patients via a shaking mechanism, although this is a rare manifestation of nonaccidental trauma.7
A number of anatomic differences between the pediatric and adult cervical spine predispose children to different patterns of injury (Table 139-1). In particular, the relatively larger head-to-body ratio in young children creates a fulcrum at C2-C3 (compared to C5-C6 in adults) that accounts for higher rates of cervical spine injury above C3 in children. Weaker muscles and ligaments combined with anterior wedging and shallow facets connecting cervical vertebrae and immature growth centers together allow for easier anterior-posterior slipping of the vertebrae than in adults.
Patients younger than 8 years of age incur high ligamentous injuries more often than older children and adults. Fractures tend to occur at the weak points in the bones—synchondroses and ossification centers. Dens fractures occur most commonly along the synchondrosis, especially in children younger than age 7 years. The mechanism of injury is usually a forward facing child in a high-speed motor vehicle crash with rapid forward flexion. Atlanto-occipital and atlantoaxial dislocation injuries are devastating vertical distraction injuries that occur in the very young child, most commonly from a motor vehicle crash, and usually result in rapid death (Figure 139-1).
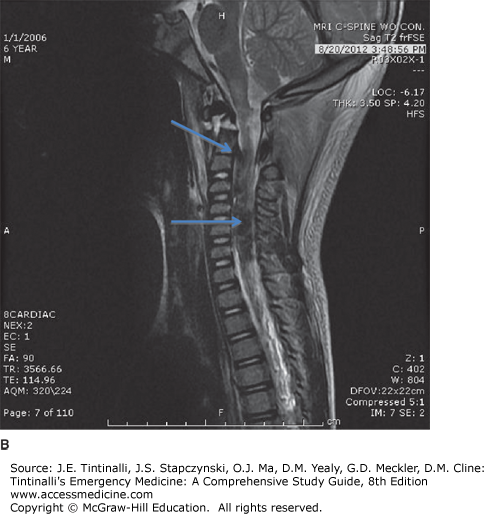
FIGURE 139-1.
Atlantoaxial dislocation in a 6-year-old boy involved in a motor vehicle crash. A. Lateral plain radiograph reveals atlantoaxial dislocation (blue arrow). B. MRI of the same patient reveals a near-complete transection of the brain stem at the level of the distal medulla, extensive ligamentous injury with resulting atlantoaxial dissociation, extensive intrathecal hematoma and hemorrhage, C1-C2 interspinous ligament tear, and prevertebral soft tissue swelling and edema around the nuchal ligament (blue arrows).
Proper immobilization of the cervical spine is of primary concern in the ED. Immobilization may be difficult in young children who are frightened or agitated, and placement of a cervical collar in children <7 years old while on a flat surface (e.g., spine board) may cause unwanted flexion of the cervical spine with further harm. A number of untoward effects have been associated with immobilization on a long backboard and cervical spine immobilization, including development of decubitus ulcers, flexion of the neck causing respiratory compromise, worsening of atlanto-occipital distraction injury, increased intracranial pressure, and musculoskeletal pain that may mimic injury and lead to increased radiologic investigation.8–20
For those at significant risk for cervical spine injury, neutral positioning of the neck is important; consider elevating the torso 2.5 cm (or more for children <4 years of age) from the spine board in order to alleviate neck flexion caused by the large occiput, and place padding beneath the child. Neutral position is achieved by aligning the external auditory meatus with the shoulders. Proper sizing of pediatric cervical collars is equally important and varies depending on the device used. If the proper-size collar is not available, use towel rolls or foam blocks placed on both sides of the child’s head and secured to the backboard with tape across the forehead.
Ask parents, witnesses, or prehospital personnel about the mechanism of injury: children with cervical spine injury will usually have a history of high-force acceleration/deceleration (as seen in motor vehicle crashes) or axial loading trauma (falls, diving injuries). Trivial mechanisms such as a ground-level fall usually do not lead to serious spine injury unless the patient has a condition associated with cervical spine instability (see “Special Considerations” later in the chapter). In the cooperative, verbal child, ask about symptoms such as neck pain, sensory deficits, or weakness. One large multicenter case-control study looking at 521 children with blunt trauma and cervical spine injury identified eight factors associated with cervical spine injury after blunt trauma (Table 139-2).21 Absence of these eight factors had a 98% sensitivity and 26% specificity for cervical spine injury. Prospective studies for validation of these risk factors are forthcoming.
Examine the child with a primary survey of airway, breathing, and circulation, followed by a complete head-to-toe examination to identify major and potentially distracting injuries that may complicate the specific evaluation of the cervical spine.
Pay careful attention to breathing, because damage to C3-C5 can injure the phrenic nerve, impairing innervation to the diaphragm, compromising respiratory mechanics, and leading to apnea. Injury to the high cervical spine can affect hemodynamic stability from spinal shock. Intubated or obtunded trauma patients should have a cervical collar remain in place, and imaging should be performed.
In children who are cooperative and alert, assess for midline neck tenderness, the presence of torticollis, and neurologic deficits while maintaining inline stabilization of the neck. Sensory symptoms such as numbness or tingling are the most common neurologic deficits among pediatric cervical spine injury patients, and persistent sensory deficits may help localize the level of the injury.
Test for motor function in the cooperative child: shoulder shrug is controlled by C5, elbow flexion and wrist extension by C6, elbow extension and wrist flexion by C7, and finger flexion by C8. Also check deep tendon reflexes: the biceps reflex tests C5, the brachioradialis reflex tests C6, and the triceps reflex tests C7.
Distinguishing between bony cervical spine injury, SCIWORA, and peripheral nerve injury (brachial plexus) from sports-related accidents can be challenging. Transient burning sensation of the hands and fingers has been described with hyperextension injuries among young football players and may indicate central cord contusion. Muscular torticollis causes neck pain in children but typically lacks a history of trauma. Infectious causes of neck pain in children include cervical adenitis and deep space infections such as retropharyngeal and peritonsillar abscess. These conditions are associated with fever and toxic appearance and do not include a history of injury.
Routine laboratory testing is not helpful in the general evaluation of cervical spine injury in children but may be useful in the context of multisystem trauma.