BACTERIAL MENINGITIS
Bacterial meningitis is a life-threatening emergency that affects 1.38 out of 100,000 people, with a case fatality rate of 14.3%.1 Although the incidence of bacterial meningitis has declined significantly since the initiation of vaccination programs, the disease is still prevalent and associated with significant morbidity and mortality.2,3,4 In the United States, the most common causes of bacterial meningitis are Streptococcus pneumoniae (58.0%), group B Streptococcus (18.1%), Neisseria meningitidis (13.9%), Haemophilus influenzae (6.7%), and Listeria monocytogenes (3.4%).1 Escherichia coli in the neonatal population and Mycobacterium tuberculosis in immunocompromised hosts are also important considerations.5
Organisms enter the cerebrospinal fluid either through hematogenous or direct contiguous spread. In hematogenous spread, bacteria colonize the upper airway and invade the bloodstream, gradually making their way to the subarachnoid space. The subcapsular components of S. pneumoniae, H. influenzae type b, and N. meningitides induce an inflammatory cascade, and leukocyte toxins cause cellular swelling and inflammation of the brain and meninges.6 Blood–brain barrier permeability increases, allowing protein and water to enter and leading to vasogenic edema. Cerebrospinal fluid drainage is inhibited by reduced absorption of the arachnoid granules with resultant obstruction and hydrocephalus, and cerebrospinal fluid is forced into the periventricular parenchyma causing interstitial edema. Disruption of cell membrane homeostasis causes cytotoxic edema. As the brain and meninges rest in a fixed-volume skull, this leads to an elevation in intracranial pressure. Vasculitis decreases cerebral blood flow and can cause ischemia and thrombosis. Additionally, neurons are directly injured by free radicals from granulocytes and endothelial cells.7
In direct contiguous spread, organisms gain entry into the cerebrospinal fluid from adjacent infections such as sinusitis, brain abscess, or otitis media. Organisms can also enter directly with penetrating traumatic injury, through congenital defects, or during neurosurgical procedures. In these cases, the organisms and their pathophysiologic effects vary.
Important risk factors for bacterial meningitis are listed in Table 174-1.
Acute or chronic otitis media Sinusitis Immunosuppression/splenectomy Alcoholism Pneumonia Diabetes mellitus Cerebrospinal fluid leak Pneumonia Endocarditis Neurosurgical procedure/head injury Indwelling neurosurgical device/cochlear implant Advanced age Malignancies Liver disease Unvaccinated to Haemophilus influenzae type b, Neisseria meningitidis, or Streptococcus pneumoniae |
The presentation of fever, headache, stiff neck, and altered mental status is commonly seen in patients with bacterial meningitis. Although most patients have at least two of four of these symptoms, their absence does not exclude meningitis. Headache is the most common symptom and is seen in more than 85% of patients. Fever is the second most common symptom.7 Seizures and focal neurologic deficits are seen in 25% to 30% of patients.
Assess historical data in order to elicit risk factors suggestive of certain pathogens. N. meningitidis is associated with close living quarters, such as in military barracks and college dormitories. Unvaccinated patients are at risk for H. influenzae. Consider L. monocytogenes in older adults and alcoholics.8 Penetrating head trauma makes S. pneumoniae more likely. Staphylococcus aureus, coagulase-negative staphylococci, and streptococci are the most commonly implicated organisms after craniotomy, whereas coagulase-negative staphylococci are commonly seen after ventriculoperitoneal shunt and spinal surgery.4 Immunocompromised patients, such as those with human immunodeficiency virus, on chronic steroids, or with a history of splenectomy, are susceptible to meningitis with encapsulated organisms.
Evaluate for focal neurologic dysfunction such as hemiparesis, facial asymmetry, visual field deficits, or disordered eye movements. Increased intracranial pressure can cause papilledema, decreased venous pulsations, or cranial nerve palsy especially involving cranial nerves 3, 4, 6, and 7. Assess for meningeal irritation with Brudzinski sign (flexion of hips and knees in response to passive neck flexion) and Kernig sign (contraction of the hamstrings in response to knee extension while the hip is flexed). Examine the skin for cutaneous stigmata such as petechiae, splinter hemorrhages, and pustules, and consider aspirating to send for culture.9 Percuss the sinuses and examine the ears for signs of primary infection.
The diagnosis of meningitis is based on cerebrospinal fluid results obtained by lumbar puncture (LP). Withhold LP if there is coagulopathy, as evidenced by thrombocytopenia or anticoagulant or antithrombotic use, until coagulopathy is corrected. As a general rule, a platelet count ≤20,000/μL (and some prefer ≤50,000/μL) or INR ≥1.5 is a contraindication to performing an LP on an emergent basis.10 The risk of bleeding complications such as epidural hematoma resulting from LP in the presence of aspirin, antiplatelet agents, and nonsteroidal anti-inflammatory drugs is not known, and risks and benefits of LP must be considered in such circumstances.11,12 Send cerebrospinal fluid for studies including Gram stain and culture, cell count with differential, glucose, and protein.7 Typical cerebrospinal fluid findings for bacterial, viral, fungal, and neoplastic meningitides are listed in Table 174-2,13,15,16 but there is considerable overlap in findings.
| Opening Pressure (<170 mm H2O)* | Color (clear) | Gram Stain (negative) | Cell Count (<5 WBC, 0 PMN) | Glucose (>40 mg/dL) | Protein (<50 mg/dL) | Cytology (negative) | |
|---|---|---|---|---|---|---|---|
| Bacterial | Elevated | Cloudy, turbid | Positive (60%–80% before antibiotic, 7%–41% after antibiotic) | >1000–2000/mm3 WBC, neutrophilic predominance, >80% PMN | <40 mg/dL, CSF/blood glucose ratio <0.3–0.4 | >200 mg/dL | Negative |
| Viral | Normal | Clear or bloody | Negative | <300/mm3 WBC, lymphocytic predominance, <20% PMN | Normal | <200 mg/dL | Negative |
| Fungal | Normal to elevated | Clear or cloudy | Negative | <500/mm3 | Normal to slightly low | >200 mg/dL | Negative |
| Neoplastic | Normal | Clear or cloudy | Negative | <300/mm3 | Normal to slightly low | >200 mg/dL | Positive |
Bacterial meningitis is associated with an elevated opening pressure >170 mm H2O, and WBCs are elevated greater than 1000/mm3 with a neutrophilic predominance. Gram stain is positive in 60% to 80% of patients before antibiotics are initiated, with a significant decline once antibiotics have been started. Cerebrospinal fluid protein is often elevated above 200 milligrams/dL, and glucose is often decreased below 40 milligrams/dL or the glucose serum–to–cerebrospinal fluid ratio is <0.4.13,14,15 Although it is not specific for bacterial meningitis, cerebrospinal fluid lactate is a promising indicator to assist with differentiation between aseptic and bacterial meningitis.16
Sterilization of the cerebrospinal fluid is possible within 2 hours of initiating parenteral antibiotics in meningococcal and 6 hours in pneumococcal meningitis, highlighting the importance of timely LP.17 Without antibiotics, Gram stain is positive in 60% to 80% of cases, but in patients treated with antibiotics, the Gram stain is positive in 7% to 41%.15 Cerebrospinal fluid culture is positive in 80% to 90% of cases if cerebrospinal fluid analysis is preformed before antibiotics are initiated, although results are not available during the course of the ED stay. However, when bacterial meningitis is considered, never withhold empiric antibiotic therapy in order to collect the cerebrospinal fluid sample.18
Rapid latex agglutination tests can be used to detect bacterial antigens and improve bacterial identification. These tests are available for S. pneumoniae, group B streptococci, H. influenzae, E. coli, and N. meningitides, but are associated with false-positive and false-negative results and limited sensitivity and specificity. Polymerase chain reaction testing is highly sensitive for organisms such as S. pneumoniae, N. meningitides, group B streptococci, H. influenzae, L. monocytogenes, and M. tuberculosis but does not provide information on antimicrobial susceptibility.7 Serum procalcitonin, C-reactive protein, and cerebrospinal fluid lactate concentrations have been studied as adjuncts to diagnosis of bacterial meningitis with negative cerebrospinal fluid examinations, but are not a substitute for decision making in the treatment of an individual patient.19 If suspicion is great despite negative initial cerebrospinal fluid results, admit for empiric antibiotic treatment and consider repeat LP.13
Perform the LP as soon as possible to secure the diagnosis of meningitis. Concern about the complication of cerebral herniation from LP has led to controversy regarding whether patients require a CT scan of the brain prior to the procedure.15
Risk factors for brain herniation are listed in Table 174-3. Order a head CT prior to LP in patients exhibiting any of these high-risk criteria. Although a CT scan can help identify contraindications for an LP, a normal CT scan does imply that there is no risk of herniation with LP if a patient exhibits clinical predictors of impending herniation such as deteriorating mental status, posturing, irregular respirations and pupillary changes, or seizures.20
Altered mental status or deteriorating level of consciousness Focal neurologic deficit New-onset seizure Papilledema Immunocompromised state Malignancy History of focal CNS disease (stroke, focal infection, tumor) Concern for mass CNS lesion Age >60 y |
After addressing airway, breathing, and circulation status, immediately initiate empiric antibiotic therapy if bacterial meningitis is clinically suspected. Never delay administration of empiric antibiotic therapy for neuroimaging or to perform LP, because antibiotic treatment takes precedence over definitive diagnosis.6 Obtain blood cultures to assist in identification of the organism and to help guide inpatient therapy if it will not delay time to antibiotics. Base antibiotic selection on the clinical scenario including age, immunization status, living conditions, and past medical history.
The empiric antibiotic regimen for adults between 18 and 49 years of age is a third-generation cephalosporin, such as ceftriaxone, 2 grams IV, plus vancomycin, 15 milligrams/kg IV, to cover the common pathogens S. pneumoniae and N. meningitides. For adults over the age of 50 years who are immunocompromised, add ampicillin, 2 grams IV, to cover L. monocytogenes.6 If patients have a severe allergy to penicillin, options include replacing ceftriaxone with chloramphenicol and substituting ampicillin with trimethoprim-sulfamethoxazole. Consider adding acyclovir if herpes simplex virus (HSV) encephalitis is suspected.13 Use a fourth-generation cephalosporin, such as cefepime, plus vancomycin for patients who have recently undergone neurosurgery.14 Initiate antibiotics as soon as possible in order to increase survival and reduce morbidity.3,7
The second priority is administration of steroids to patients with presumptive pneumococcal meningitis. Administration of dexamethasone before or with the first dose of antibiotics has been shown to reduce cerebrospinal fluid inflammation, reduce the risk of morbidity and mortality in adults, and reduce hearing loss and other neurologic sequelae in children, especially with S. pneumoniae infection.8,21 The recommended dosage of dexamethasone is 10 milligrams IV for adults.21
Current guidelines provide no recommendation for the most common ED situation, in which the first dose of empiric antibiotics is given before LP is performed or before results of LP are received. Common sense suggests that dexamethasone could be administered just before, or concurrently with, empiric antibiotics to patients with strong suspicion for bacterial meningitis or to patients in whom grossly purulent cerebrospinal fluid is obtained at the time of LP. Infectious Disease Society of America guidelines state that dexamethasone should not be given to adults who have already received antibiotics.
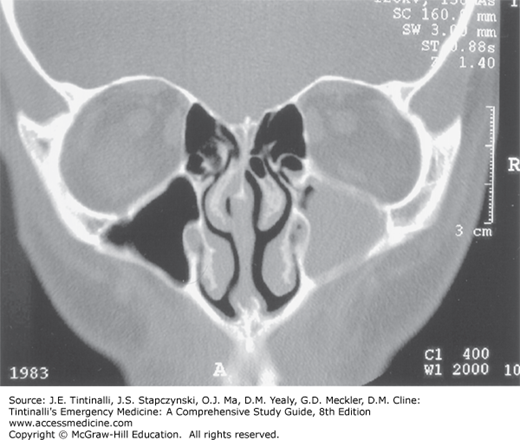
The prevalent use of antibiotics has decreased the frequency of suppurative intracranial complications from sinusitis and otitis, but bacterial meningitis resulting from these diseases still occurs. The virulence of the affecting organism and host factors, such as immunocompromised state, influence spread to the CNS. In the ear, bacteria can spread through endolymphatic channels, bony erosions, or osteothrombophlebitis of small vessels. Thrombophlebitis of veins is a common mechanism by which bacteria disseminate from the sinuses; this may result in cavernous sinus thrombosis or empyema.22 CT imaging is very sensitive for sinusitis and permits earlier diagnosis with demonstration of air-fluid levels in the involved sinuses. CT is nonspecific, however, and should be interpreted with the clinical background in mind (Figure 174-1). Infections are often polymicrobial. Initiate empiric antibiotic therapy with fluoroquinolones, such as levofloxacin or moxifloxacin, or with a third-generation cephalosporin, such as ceftriaxone, plus metronidazole.23 Invasive infections and those with intracranial spread require emergency consultation for surgical drainage.
Monitor patients with meningitis closely for complications or signs of clinical deterioration, especially evaluating their respiratory and neurologic status.8 Treat hyperpyrexia and manage seizures with anticonvulsants. Avoid hypotonic fluids, and monitor serum sodium level serially to detect syndrome of inappropriate antidiuretic hormone or cerebral salt wasting.7,21 Closely evaluate for signs of increased intracranial pressure and vasculopathy that may lead to brain ischemia. If signs of elevated intracranial pressure are detected, elevate the bed to 30 degrees, use 25% mannitol or hypertonic 3% saline for diuresis, and consider a trial of mild hyperventilation.7 Measurement of intracranial and systemic arterial pressure may be useful in severe cases to monitor cerebral perfusion pressure. Consider admission to the intensive care unit to ensure proper level of care.8
Bacterial meningitis is spread by droplets, and risk for developing bacterial meningitis after exposure is estimated to be 500 to 800 times higher than the general population.14 Chemoprophylaxis has been shown to decrease transmission of N. meningitidis by 89% in close contacts. Chemoprophylaxis is recommended for individuals who have been exposed to patients diagnosed with N. meningitidis and H. influenzae.9 It is not recommended for patients diagnosed with pneumococcal meningitis.14 Close contacts include housemates, individuals exposed to secretions (shared utensils or toothbrushes, kissing, mouth-to-mouth resuscitation), and individuals who intubated the patient without a facemask. To be most effective, initiate chemoprophylaxis within 24 hours of contact. Risk of infection after a period of 2 weeks from exposure is considered rare, and prophylaxis is not recommended after this time period. Treatment options for high-risk contacts include rifampin 10 milligrams/kg to a maximum of 600 milligrams per dose every 12 hours for four doses, ciprofloxacin 500 milligrams orally once, or ceftriaxone 250 milligrams IM once.9 Instruct all patients who receive chemoprophylaxis to seek medical attention immediately if they develop any symptoms of illness or meningitis.
Admit all patients diagnosed with bacterial meningitis and those highly suspected of having meningitis to the hospital on droplet isolation.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree