Chapter 19 Cardiovascular Emergencies
Assessment of Chest Pain
• The PQRST mnemonic (Table 19-1) is useful in assessing the characteristics of chest pain and may be used to gather comprehensive information about the nature of the pain.
• Patients often deny “pain” but complain of burning, pressure, or tightness. Describe the patient’s pain or discomfort using his or her own words in the documentation.
• Assess for “anginal equivalents,” particularly in women, diabetics, and the elderly.
• Have the patient rate the pain or discomfort on a scale of 1 to 10.
• Obtain a 12-lead electrocardiogram (ECG) within 10 minutes of patient arrival; assess for dysrhythmias and ST segment elevation or depression.
• There are many possible etiologies for chest pain (Table 19-2); therefore it is important to rule out the most serious or life-threatening causes immediately.
• Document current medications, including prescriptions, over-the-counter medications, and herbal therapies.
• Recent cocaine use is a common cause of ischemic chest pain resulting from coronary vasospasm. It is important to ask the patient about recreational drug use.
• Document positive and negative risk factors for cardiovascular disease, including those for previous cardiac disease such as prior myocardial infarction (MI), coronary interventions such as stent placement, and presence of a pacemaker or implantable cardioverter defibrillator (ICD).
| P | What things provoke or precipitate or palliate or alleviate the pain or discomfort? |
| Q | What is the quality of the pain or discomfort? Document this characteristic in the patient’s own words. |
| R | Does the pain or discomfort radiate? If so, to what locations? What is the location or region of the pain or discomfort? |
| S | Rate the severity of the pain or discomfort. Are there associated symptoms? |
| T | What are the time elements of the pain or discomfort? When did it start? How long did it last? Did the pain or discomfort begin suddenly or gradually? |
TABLE 19-2 LIFE-THREATENING AND NON–LIFE-THREATENING CAUSES OF CHEST PAIN
| LIFE-THREATENING | NON–LIFE-THREATENING |
|---|---|
| Acute coronary syndrome | Pericarditis |
| Pulmonary embolism | Esophageal reflex (GERD) |
| Aortic dissection | Pneumonia |
| Tension pneumothorax | Spontaneous pneumothorax |
| Acute myocardial infarction | Costochondritis |
| Pancreatitis | |
| Herpes zoster infection | |
| Cocaine use |
GERD, Gastroesophageal reflux disease.
Diagnostic Procedures
• Continuous bedside ST monitoring
• Serum electrolytes, complete blood count, clotting times, and cardiac biomarkers
• Cardiac catheterization with angiography
• Echocardiogram to determine left ventricular (LV) ejection fraction (EF); presence of hypertrophy, dyskinetic, or akinetic areas; structural abnormalities such as LV aneurysm or valvular dysfunction; and pericardial effusion
• Doppler studies of peripheral blood flow
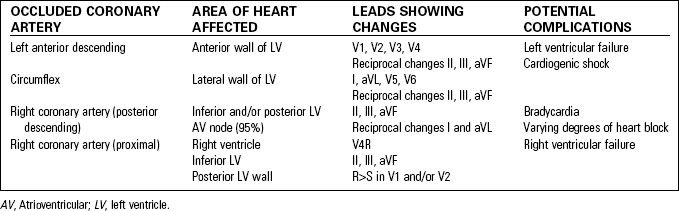
Contiguous leads are those leads that “look at” the same area of the heart.
| Anterior left ventricle (LV) | Leads V1–V4 |
| Ventricular septum | Leads V1 and V2 |
| Inferior surface of LV | Leads II, III, aVF |
| Lateral LV wall | Leads I, aVL, V5, V6 |
| Posterior LV | Leads V1 and V2 |
Specific Cardiac Emergencies
Acute Coronary Syndrome
Acute coronary syndrome (ACS) refers to the clinical presentations of acute myocardial ischemia. This continuum includes unstable angina, non–ST segment elevation myocardial infarction (non-STEMI), and ST segment elevation myocardial infarction (STEMI). These presentations represent varying degrees of myocardial oxygen supply and demand imbalance and refer to different stages of myocardial ischemia. Table 19-3 summarizes the characteristics of these three problems.
• Unstable angina—a change in the patient’s usual pattern of angina
TABLE 19-3 DIAGNOSTIC DIFFERENCES BETWEEN TYPES OF ACUTE CORONARY SYNDROME
| 12-LEAD ECG FINDINGS | CREATINE KINASE TROPONIN TEST | |
|---|---|---|
| Unstable angina | Normal or nondiagnostic changes such as ST depression and T wave inversion | Negative |
| Non-STEMI | ST depression or T wave changes | Positive |
| STEMI | ST elevation >1 mm in two contiguous leads New or presumably new LBBB | Positive |
ECG, Electrocardiogram; LBBB, left bundle branch block; STEMI, ST segment elevation myocardial infarction.
Signs and Symptoms
• Chest pain or discomfort unrelieved by rest.
• Patient may experience a sense of impending doom.
• Sign of LV failure (crackles, S3 heart sound, respiratory distress) if infarct involves a large portion of the anterior left ventricle.
• Tachycardia may be the result of sympathetic stimulation; bradycardia or varying degrees of atrioventricular (AV) block often seen with inferior MI.
Diagnostic Procedures
• If inferior wall MI is present, obtain right-sided V-leads to detect possible right ventricular infarct (Fig. 19-1A).
• If inferior MI is associated with ST depression in V2 and R wave larger than S wave in leads V1 and V2, obtain posterior ECG to detect possible posterior wall MI (Fig. 19-1B).
• Chest radiograph to detect pulmonary congestion or cardiac enlargement.
• Complete blood count, blood chemistries, and coagulation studies.
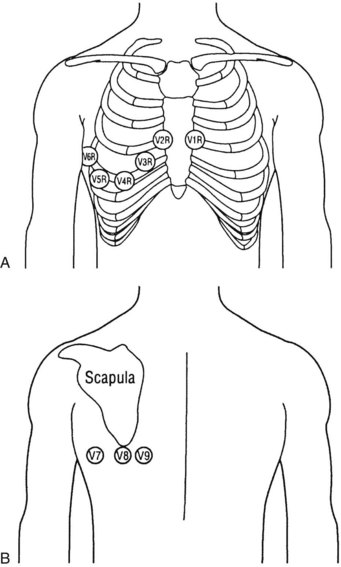
Fig. 19-1 A, Right precordial leads. B, Posterior chest leads.
(From Moser, D., & Reigel, B. [2008]. Cardiac nursing: A companion to Braunwald’s heart disease. Philadelphia, PA: W.B. Saunders.)
Therapeutic Interventions
• Administer supplemental oxygen to maintain oxygen saturation above 92%.
• Maintain intravenous (IV) access.
• Give non–enteric coated aspirin, 162 to 325 mg; have patient chew and swallow aspirin if possible. Administer aspirin as rectal suppository if necessary.
• Administer nitroglycerin sublingual tablet or spray if systolic blood pressure greater than 90 mm Hg and heart rate greater than 50 beats per minute. If the patient experiences no relief from pain, the emergency nurse may repeat nitroglycerin every 5 minutes up to three doses.
• The American Heart Association does not recommend the routine use of IV nitroglycerin in patients with STEMI.2 If it is used, monitor the patient closely for drug-induced hypotension that can decrease coronary perfusion and worsen myocardial ischemia.
• Use of morphine is indicated for STEMI when chest discomfort is unresponsive to nitrates. It should be used with caution in unstable angina and non-STEMI because of an association with increased mortality.
• Medications to limit platelet aggregation are important treatment modalities.
• In STEMI, early reperfusion of the myocardium, by pharmacologic or mechanical means, has been shown to reduce mortality.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree