Cardiopulmonary Resuscitation
John A. Paraskos
Alan A. Orquiola
History
Since the introduction of cardiopulmonary resuscitation (CPR), we have been forced to rethink our definitions of life and death. Although sporadic accounts of attempted resuscitations are recorded from antiquity [1, 2 and 3], until recently no rational quarrel could be found with the sixth century BC poetic fragment of Ibycus, “You cannot find a medicine for life once a man is dead” [4]. Until 1960, successful resuscitation was largely limited to artificial ventilation for persons who had undergone respiratory arrest due to such causes as near-drowning, smoke inhalation, and aspiration. Such attempts were likely to succeed if performed before cardiac arrest had resulted from hypoxia and acidosis. Emergency thoracotomy with “open heart massage” was rarely resorted to and was occasionally successful if definitive therapy was readily available [5]. Electrical reversal of ventricular fibrillation (VF) by externally applied electrodes was described in 1956 by Zoll et al. [6]. This ability to reverse a fatal arrhythmia without opening the chest challenged the medical community to develop a method of sustaining adequate ventilation and circulation long enough to bring the electrical defibrillator to the patient’s aid. By 1958, adequate rescue ventilation became possible with the development of the mouth-to-mouth technique described by Safar et al. [7, 8] and Elam et al. [9]. In 1960, Kouwenhoven et al. [10] described “closed chest cardiac massage,” thus introducing the modern era of CPR. The simplicity of this technique—“all that is needed are two hands”—has led to its widespread dissemination. The interaction of this technique of sternal compression with mouth-to-mouth ventilation was developed as basic CPR. The first national conference on CPR was sponsored by the National Academy of Sciences in 1966 [11]. Instruction in CPR for both professionals and the public soon followed through community programs in basic life support (BLS) and advanced cardiac life support (ACLS). Standards for both BLS and ACLS were set in 1973 [12] and were updated in 1979 [13], 1985 [14], 1992 [15], 2000 [16], and 2005 [17].
For some individuals with adequately preserved cardiopulmonary and neurologic systems, the cessation of breathing and cardiac contraction may be reversed if CPR and definitive care are quickly available. If other systems are also spared, prolonged and vigorous life may ensue. The short period during which the loss of vital signs may be reversed is often referred to as clinical death. For clinical death to be reversed, however, ventilation and circulation must be restored before irreversible damage to vital structures occurs. The state of irreversible death is referred to as biologic death. In difficult circumstances, the best single criterion (medical and legal) for the ultimate death of the functioning integrated human individual (i.e., the person) is brain death [18, 19, 20, 21, 22 and 23]. By this criterion, we can make decisions as to the appropriateness of continuing “life-sustaining” techniques.
Efficacy
The value of standardized CPR continues to undergo considerable scrutiny. Unfortunately, it appears that its efficacy is limited. CPR does not seem to go beyond short-term sustaining of viability until definitive therapy can be administered. This was the stated goal of Kouwenhoven et al. [10]. The benefit of rapid initiation of CPR has been demonstrated in numerous studies [24, 25, 26, 27, 28 and 29]. Data from prehospital care systems in Seattle showed that 43% of patients found in VF were discharged from the hospital if CPR (i.e., BLS) was applied within 4 minutes and defibrillation (i.e., ACLS) within 8 minutes. If either was delayed, survival rates were much lower. Survival rates for patients in asystole or with pulseless electrical activity (PEA) were much lower [30, 31, 32 and 33]. In a Miami study, none of the patients found in bra- dyarrhythmia or asystole survived, whereas 23% of those in VF were eventually discharged [34, 35]. Perhaps one of the benefits of the early initiation of CPR is the prolongation of VF, which increases the likelihood that ACLS with attempts at defibrillation will be successful. If the onset of CPR is delayed, or if the time to defibrillation is longer than 10 minutes, the probability is greater that the patient will be in asystole or in fine VF and will convert to asystole.
Even though patients experiencing cardiac arrest in the hospital can be expected to receive CPR and definitive therapy well within the 4- and 8-minute time frames, older studies determined that their chances of being discharged alive were generally worse than for out-of-hospital patients. This was thought to be due to serious underlying medical problems [36, 37, 38, 39 and 40]. A more recent study suggests that when in-hospital cardiac arrests due to VF or ventricular tachycardia (VT) are witnessed and defibrillation is conducted rapidly, survival to discharge is excellent [41].
In 1967, Pantridge and Geddes [42] introduced the mobile intensive care unit (ICU) in Belfast, Ireland. Since then, emergency medical transport programs have spread throughout the world. In recent decades, there has been a move to further approximate the mobile ICU of Pantridge and Geddes by adding the capability of defibrillation to the emergency medical service system [43, 44, 45 and 46]. This is already in place in most metropolitan areas. Recognizing the importance of early defibrillation, it is
imperative that all first-response systems provide this necessary service, either by using emergency medical technicians capable of performing defibrillation or by equipping and training emergency personnel with automatic or semiautomatic defibrillators [47, 48, 49 and 50]. The development of inexpensive, small, lightweight, easy-to-use, voice-prompted defibrillators would allow early access to defibrillation, before the arrival of emergency medical services (EMS) [51, 52]. Where these have been made available, and where first-responders have been trained in their use, survival rates have been dramatically improved [53, 54 and 55].
imperative that all first-response systems provide this necessary service, either by using emergency medical technicians capable of performing defibrillation or by equipping and training emergency personnel with automatic or semiautomatic defibrillators [47, 48, 49 and 50]. The development of inexpensive, small, lightweight, easy-to-use, voice-prompted defibrillators would allow early access to defibrillation, before the arrival of emergency medical services (EMS) [51, 52]. Where these have been made available, and where first-responders have been trained in their use, survival rates have been dramatically improved [53, 54 and 55].
Although the current approach is modestly successful for VF, CPR techniques have most likely not yet been optimized, and further improvement is greatly needed [56]. Cardiac output has been measured at no better than 25% of normal during conventional CPR in humans [57 58, 59 and 60]. In animal models, myocardial perfusion and coronary flow have been measured at 1% to 5% of normal [61, 62 and 63]. Cerebral blood flow has been estimated to be 3% to 15% of normal when CPR is begun immediately [64, 65 and 66], but it decreases progressively as CPR continues [67, 68] and intracranial pressures rise [69, 70]. Despite these pessimistic findings, complete neurologic recovery has been reported in humans even after prolonged administration of CPR [71].
Researchers continue to evaluate new approaches and techniques, and further refinements in the delivery of CPR can be expected. Although research in this area must be enthusiastically encouraged, assiduous attention to research methods and their applicability to humans is required to prevent an overly hasty and potentially injurious change in the current guidelines. The wide variety of experimental methods and models makes evaluation of apparently contradictory research results difficult. Animal preparations for research in resuscitative techniques have limited application to humans, largely because of differences in size and configuration of the thoracic cage. Before new basic CPR techniques can be endorsed with any confidence, they must have been demonstrated to improve either survival or neurologic outcome. In addition, they must be simple to apply in an arrest and, optimally, they should be simple to teach and applicable by one rescuer without undue effort.
Mechanisms of Blood Flow During Resuscitation
Any significant improvement in CPR technique would seem to require an understanding of the mechanism by which blood flows during CPR. However, there is no unanimity among researchers in this area. It is of interest that significant advances seem to have been made by research groups holding very different ideas concerning the basic mechanism of blood flow during CPR. Indeed, it is possible that several mechanisms are operative; which of these is most important may vary according to a patient’s size and chest configuration.
Cardiac Compression Theory
In 1960, when Kouwenhoven et al. [10] reported on the efficacy of closed chest cardiac massage, most researchers accepted the theory that blood is propelled by compressing the heart trapped between the sternum and the vertebral column. According to this theory, during sternal compression the intraventricular pressures would be expected to rise higher than the pressures elsewhere in the chest. With each sternal compression, the semilunar valves would be expected to open and the atrioventricular (AV) valves to close. With sternal release, the pressure in the ventricles would be expected to fall and the AV valves to open, allowing the heart to fill from the lungs and systemic veins. Indeed, an echocardiographic study using minipigs has shown such valve motion, and a transesophageal echocardiographic study in humans also supports this theory [72,73]. Although some animal studies have demonstrated pressure changes consistent with this theory [74], most have not [75]. If the cardiac compression mechanism were operative, ventilation would best be interposed between sternal compressions so as not to interfere with cardiac compression. Also, the faster the sternal compression, the higher the volume of blood flow, assuming that the ventricles could fill adequately. The theory of cardiac compression was first brought into question in 1962, when Weale and Rothwell-Jackson [76] demonstrated that during chest compression there is a rise in venous pressure almost equal to that of the arterial pressure. The following year, Wilder et al. [77] showed that ventilating synchronously with chest compression produced higher arterial pressures than alternating ventilation and compression. It was more than a decade, however, before more data confirmed these initial findings.
Thoracic Pump Theory
In 1976, Criley et al. [78] reported that during cardiac arrest, repeated forceful coughing is capable of generating systolic pressures comparable with those of normal cardiac activity. This finding strongly suggested that high intrathoracic pressures are capable of sustaining blood flow, independent of sternal compression. Subsequently, Niemann et al. [79] proposed that the propulsion of blood during sternal compression is due to the same mechanism of increased intrathoracic pressure. Studies using pressure measurements [80, 81] and angiography [82] support this hypothesis, as do most echocardiographic studies [83, 84]. According to this theory, the heart serves only as a conduit during CPR. Forward flow is generated by a pressure gradient between intrathoracic and extrathoracic vascular structures. Flow to the arterial side is favored by functional venous valves and greater compressibility of veins, compared to arteries, at their exit points from the thorax [75, 82, 85, 86]. The thoracic pump theory provides the rationale for experimental attempts at augmenting forward flow by increasing intrathoracic pressure.
Experimental and Alternative Techniques of CPR
Several experimental and alternate techniques of CPR are presented in Table 22-1 [64, 66, 74, 87, 88, 89, 90, 91, 92, 93, 94, 95, 96, 97, 98, 99, 100, 101, 102, 103, 104, 105 and 106].
Interposed Abdominal Compression CPR
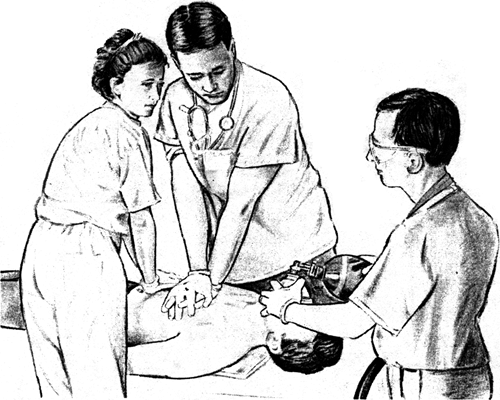
Interposed abdominal compression CPR was developed by Ralston et al. [107] and Babbs et al. [108]. This technique includes manual compression of the abdomen by an extra rescuer during the relaxation phase of chest compression (Fig. 22-1).
The mid-abdomen is compressed at a point halfway between the xiphoid process and the umbilicus with a force of approximately 100 mm Hg of external pressure. This pressure is estimated to be equivalent to that required to palpate the aortic pulse in a subject with a normal pulse. Two randomized clinical trials have demonstrated a statistically significant improvement in outcome measures for in-hospital cardiac arrest [109, 110], but no improvement has been shown for out-of-hospital arrest [111]. Based on these findings, interposed abdominal compression CPR is recommended as an option for in-hospital cardiac arrest when sufficient personnel trained in the technique are available. However, it should be emphasized that the safety and efficacy of interposed abdominal compression CPR in patients with recent abdominal surgery, pregnancy, or aortic aneurysm has not been studied.
The mid-abdomen is compressed at a point halfway between the xiphoid process and the umbilicus with a force of approximately 100 mm Hg of external pressure. This pressure is estimated to be equivalent to that required to palpate the aortic pulse in a subject with a normal pulse. Two randomized clinical trials have demonstrated a statistically significant improvement in outcome measures for in-hospital cardiac arrest [109, 110], but no improvement has been shown for out-of-hospital arrest [111]. Based on these findings, interposed abdominal compression CPR is recommended as an option for in-hospital cardiac arrest when sufficient personnel trained in the technique are available. However, it should be emphasized that the safety and efficacy of interposed abdominal compression CPR in patients with recent abdominal surgery, pregnancy, or aortic aneurysm has not been studied.
TABLE 22-1. Experimental and Alternate Techniques of Cardiopulmonary Resuscitation (CPR) | |||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Open Chest CPR
One of the first forms of successful CPR was open chest CPR. It was shown to be effective when definitive care was rapidly available and is associated with survival rates, largely in operating room arrests, ranging from 16% to 37% [5, 112, 113]. Mechanistically, open chest CPR clearly involves cardiac compression without use of a thoracic gradient. Weale and Rothwell-Jackson [76] demonstrated lower venous pressures and higher arterial pressures than with closed chest compression. There is considerable evidence that open chest CPR may be more efficacious than closed chest CPR in terms of cardiac output and cerebral and myocardial preservation [114, 115]. One study has suggested increased return of spontaneous circulation with open chest CPR [116]. Clearly, some patients with penetrating chest trauma are not likely to respond to chest compression and are candidates for open chest CPR [59, 117, 118]. Several studies suggest a benefit from thoracotomy in these patients [119, 120 and 121]. If open chest CPR is to be used, it should be used early in the sequence [122, 123]. Patients with blunt chest and abdominal trauma may also be candidates for open chest CPR. Obviously, this technique should not be attempted unless adequate facilities and trained personnel are available.
Cardiopulmonary Bypass for Unresponsive Arrest
Cardiopulmonary bypass is certainly not a form of routine life support; however, it has been considered as a possible adjunct to artificial circulation. It is an indispensable adjunct to cardiac surgery and is being used more frequently for invasive
procedures as a standby in case of sudden cardiac collapse. Cardiopulmonary bypass has been used in arrests unresponsive to standard methods of CPR [124]. In dog models, bypass has been shown capable of providing near-normal end-organ blood flow with improved “resuscibility” and neurologic status [125, 126, 127, 128 and 129]. Emergency bypass can be instituted with femoral artery and vein access, without thoracotomy [130]. Further study of its use in humans will be necessary before it can be recommended for wider use in cardiac arrest. Its potential use is restricted to centers capable of providing this technological level of treatment. The cost necessitates careful consideration of the potential to save the patient.
procedures as a standby in case of sudden cardiac collapse. Cardiopulmonary bypass has been used in arrests unresponsive to standard methods of CPR [124]. In dog models, bypass has been shown capable of providing near-normal end-organ blood flow with improved “resuscibility” and neurologic status [125, 126, 127, 128 and 129]. Emergency bypass can be instituted with femoral artery and vein access, without thoracotomy [130]. Further study of its use in humans will be necessary before it can be recommended for wider use in cardiac arrest. Its potential use is restricted to centers capable of providing this technological level of treatment. The cost necessitates careful consideration of the potential to save the patient.
Infectious Diseases and CPR
The fear provoked by the spread of human immunodeficiency virus (HIV) may lead to excessive caution when dealing with strangers; it has clearly decreased the willingness of both the lay public and health professionals to learn and perform CPR. The effect of this fear on CPR is serious and must be addressed at some length [131].
The public’s fear can be counteracted only by continued education and by stressing the facts. Health care workers have more opportunities for exposure to patients with HIV and their concerns must be adequately addressed [132].
Saliva has not been implicated in the transmission of HIV even after bites, percutaneous inoculation, or contamination of open wounds with saliva from HIV-infected patients [133, 134, 135, 136, 137 and 138]. Hepatitis B-positive saliva has also not been demonstrated to be infectious when applied to oral mucous membranes or through contamination of shared musical instruments or CPR training manikins used by hepatitis B carriers. However, it is not impossible that the mouth-to-mouth technique might result in the exchange of blood between patient and rescuer if there are open lesions or trauma to the buccal mucosa or lips. Diseases such as tuberculosis, herpes, and respiratory viral infections are potentially spread during mouth-to-mouth ventilation. Infections thought to have been transmitted by CPR include Hel-icobacter pylori [139], Mycobacterium tuberculosis [140], meningococcus [141], herpes simplex [142], Shigella [143], Streptococcus [144], Salmonella [145], and Neisseria gonorrhea [146]. There have been no cases reported of transmission of HIV, hepatitus B virus, hepatitis C virus, or cytomegalovirus [146]. The impact of these facts is different for lay people and health care professionals, and different for those carrying infection and for those at risk of infection [147].
Implications for Rescuers with Known or Potential Infection
Potential rescuers who know or highly suspect that they are infected with a serious pathogenic organism should not perform mouth-to-mouth ventilation if another rescuer is available who is less likely to be infectious or if the circumstances allow for any other immediate and effective method of ventilation, such as using mechanical ventilation devices.
Implications for Health Care Professionals
Although the probability of a rescuer becoming infected with HIV during CPR seems minimal, all those called on to provide CPR in the course of their employment should have ready access to mechanical ventilation devices. Bag-valve mask devices should be available as initial ventilation equipment, and early endotracheal intubation should be encouraged when equipment and trained professionals are available. Masks with one-way valves and plastic mouth and nose covers with filtered openings are available and provide some protection from transfer of oral fluids and aerosols. S-shaped mouthpieces, masks without one-way valves, and handkerchiefs provide little, if any, barrier protection and should not be considered for routine use. With these guidelines in mind, health care professionals are reminded that they have a special moral and ethical, and in some instances legal, obligation to provide CPR, especially in the setting of their occupational duties.
Implications for Manikin Training in Cardiopulmonary Resuscitation
The guidelines of the American Heart Association (AHA) specify that students or instructors should not actively participate in CPR training sessions with manikins if they have dermatologic lesions on their hands or in oral or circumoral areas, if they are known to be infected with hepatitis or HIV, or if they have reason to believe that they are in the active stage of any infectious process. In routine ventilation training, instructors should not allow participants to exchange saliva by performing mouth-to-mouth ventilation in sequence without barrier mouthpieces. Special plastic mouthpieces and specialized manikins protect against such interchange of mucus.
Training in CPR for People with Chronic Infections
If a potentially infectious person is to be trained in CPR, common-sense precautions should be taken to protect other participants from any risk of infection. The chronically infected individual should be given a separate manikin for practice that is adequately disinfected before anyone else uses it. The chronically infected trainee should be made aware of the preceding guidelines for potential rescuers with infections. In addition, the potential risk of infection for the immunocompromised rescuer should not be ignored.
An agency that requires successful completion of a CPR course as a prerequisite for employment must decide whether to waive its requirement for an employee who is unable to complete a CPR course for whatever reason. That agency also must determine whether a chronically infected person should continue to work in a situation in which CPR administration is a duty of employment.
Standard Procedures and Team Effort
The distinctive function of the ICU is to serve as a locus of concentrated expertise in medical and nursing care, life-sustaining technologies, and treatment of complex multiorgan system derangement. Historically, it was the development of effective treatment for otherwise rapidly fatal arrhythmias during acute myocardial infarction that impelled the medical community to establish ICUs [148]. Rapid response by medical personnel has been facilitated by constant professional attendance and the development of widely accepted guidelines for resuscitation. Each
member of the professional team is expected to respond in accordance with these guidelines.
member of the professional team is expected to respond in accordance with these guidelines.
The skills necessary to perform adequately during a cardiac or respiratory arrest and to interface smoothly with ACLS techniques cannot be learned from reading texts and manuals. CPR courses taught according to AHA guidelines allow hands-on experience that approximates the real situation and tests the psychomotor skills needed in an emergency. All those who engage in patient care should be trained in BLS. Those whose duties require a higher level of performance should be trained in ACLS as well. As these skills deteriorate with disuse, they need to be updated. It is worth noting that there is no “certification” in BLS or ACLS. Issuance of a “card” is neither a license to perform these techniques nor a guarantee of skill, but simply an acknowledgment that an individual attended a specific course and passed the required tests. If employers or government agencies require such a card of their health workers, it is by their own mandate.
The ensuing discussion of BLS and ACLS techniques follows the recommendations and guidelines established by the AHA and presented in a supplement to volume 112 of Circulation [17].
Basic Life Support for Adults With an Unobstructed Airway
BLS is meant to support the circulation and respiration of those who have experienced cardiac or respiratory arrest. After recognizing and ascertaining its need, definitive help is summoned without delay and CPR is initiated.
Respiratory Arrest
Respiratory arrest may result from airway obstruction, near-drowning, stroke, smoke inhalation, drug overdose, electrocution, or physical trauma. In the ICU, pulmonary congestion, respiratory distress syndrome, and mucous plugs are frequent causes of primary respiratory arrests. The heart usually continues to circulate blood for several minutes, and the residual oxygen in the lungs and blood may keep the brain viable. Early intervention by opening the airway and providing ventilation may prevent cardiac arrest and may be all that is required to restore spontaneous respiration. In the intubated patient, careful suctioning of the airway and attention to the ventilator settings are required.
Cardiac Arrest
Cardiac arrest results in rapid depletion of oxygen in vital organs. After 6 minutes, brain damage is expected to occur, except in cases of hypothermia (e.g., near-drowning in cold water). Therefore, early bystander CPR (within 4 minutes) and rapid ACLS with attempted defibrillation (within 8 minutes) are essential in improving survival and neurologic recovery rates [49, 149].
The sequence of steps in CPR may summarized as the ABCs of CPR: airway, breathing, and circulation. This mnemonic is useful in teaching the public, but it should be remembered that each step is preceded by assessment of the need for intervention: Before opening the airway, the rescuer determines unresponsiveness; before breathing, the rescuer determines breathlessness; before circulation, the rescuer determines pulselessness (Table 22-2).
Assessment and Determination of Unresponsiveness and Alerting of Emergency Medical Services
A person who has undergone cardiac arrest may be found in an apparently unconscious state (i.e., an unwitnessed arrest), or may be observed to suddenly lapse into apparent unconsciousness (i.e., a witnessed arrest). In either case, the rescuer must react promptly to assess the person’s responsiveness by attempting to wake and communicate with the person by tapping or gently shaking and shouting. The rescuer should summon nearby staff for help. If no other person is immediately available, the rescuer should call hospital emergency line for the resuscitation team to respond (e.g., “code blue”).
In an optimally functioning ICU, nearly all arrests should be witnessed. Early recognition of cardiac and respiratory arrests is facilitated by electronic monitoring of cardiac rhythm and often of respiratory rate and hemodynamic measurements. Video monitors often extend visual monitoring. Unfortunately, it is quite possible for a patient to become lost behind this profusion of electronic signals, the dependability of which varies widely. For several precious minutes, a heart with PEA continues to provide a comforting electronic signal, while the brain suffers hypoxic damage. A high frequency of false alarms due to loose electrodes or other artifacts may dangerously raise the threshold of awareness and prolong the response time of the ICU team. The overall efficacy of the monitoring devices, therefore, depends highly on meticulous skin preparation and care of electrodes, transducers, pressure cables, and the like.
Sudden apparent loss of consciousness, occasionally with seizures, may be the first signal of arrest and requires prompt reaction. After determining unresponsiveness, the pulse is assessed. If the carotid pulse cannot be palpated in 5 to 10 seconds, and a defibrillator is not immediately available, a precordial thump may be performed by striking the lower third of the sternum with the fist, from a height of approximately 8 inches (or the span of the stretched fingers of one hand). If the pulse does not return and a defibrillator is not immediately available, the rescuer should proceed with establishing the airway (see the next section). If a defibrillator is immediately available, it should be used instead of a precordial thump; this is expected to be the case in a monitored arrest in an ICU.
Opening the Airway and Determining Breathlessness
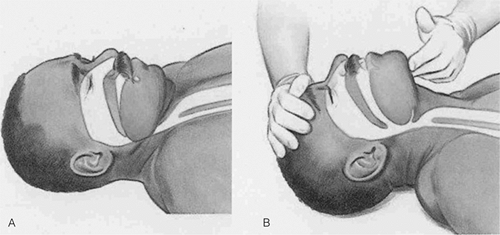
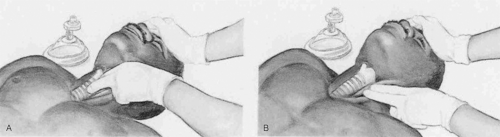
After establishing unresponsiveness and positioning the individual on his or her back (Fig. 22-2), the next step is to open the airway and check for spontaneous breathing (see Chapter 1). In a monitored arrest with VF or tachycardia, this step is taken after initial attempts to defibrillate. Meticulous attention to establishing an airway and supplying adequate ventilation is essential to any further resuscitative effort. The team leader must carefully monitor the adequacy of ventilation.
The head tilt-chin lift maneuver (Figs. 22-3 and 22-4) is usually successful in opening the airway. The head is tilted backward by a hand placed on the forehead. The fingers of the other hand are positioned under the mandible, and the chin is lifted upward. The teeth are almost approximated, but the mouth is not allowed to close. Because considerable cervical hyperextension occurs, this method should be avoided in patients with cervical injuries or suspected cervical injuries.
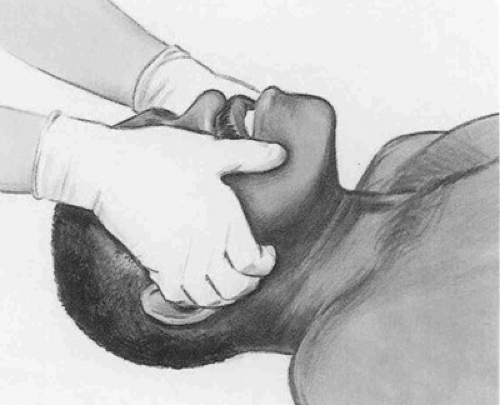
The jaw-thrust maneuver (Fig. 22-5) provides the safest initial approach to opening the airway of a patient with a cervical spine injury; it usually allows excellent airway opening with a minimum of cervical extension. The angles of the mandible are grasped using both hands and lifting upward, thus tilting the head gently backward.
The jaw-thrust maneuver (Fig. 22-5) provides the safest initial approach to opening the airway of a patient with a cervical spine injury; it usually allows excellent airway opening with a minimum of cervical extension. The angles of the mandible are grasped using both hands and lifting upward, thus tilting the head gently backward.
TABLE 22-2. Summary of Basic Life Support ABCD Maneuvers for Infants, Children, and Adults (Newborn Information Not Included)a | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
After opening the airway, the rescuer should take 3 to 5 seconds to determine whether there is spontaneous air exchange. This is accomplished by placing an ear over the patient’s mouth and nose while watching to see if the patient’s chest and abdomen rise and fall (“look, listen, and feel;” see Fig. 22-4). If the rescuer fails to see movement, hear respiration, or feel the rush of air against the ear and cheek, rescue breathing should be initiated.
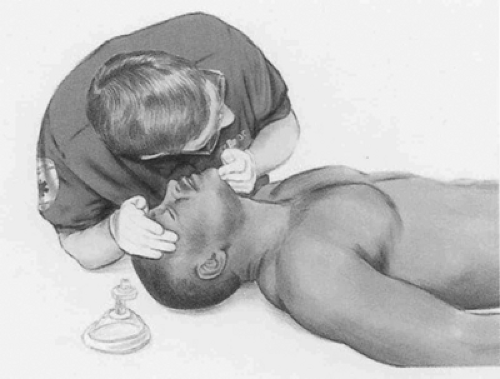
Rescue Breathing
If spontaneous breathing is absent, rescue breathing with an airway-mask-bag unit must be initiated (see Chapter 1). If
equipment is immediately available and the rescuer is trained, intubation and ventilatory adjuncts should be used initially. Each breath should be delivered during 1 second, allowing the patient’s lungs to deflate between breaths. Thereafter, the rate of ten to 12 breaths per minute is maintained for as long as is necessary, with tidal volumes of approximately 700 mL. Delivering the breath during 1 second helps to prevent gastric insufflation. Melker et al. [150, 151] demonstrated airway pressures well in excess of those required to open the lower esophageal sphincter when quick breaths are used to ventilate patients. If the patient wears dentures, they are usually best left in place to assist in forming an adequate seal.
equipment is immediately available and the rescuer is trained, intubation and ventilatory adjuncts should be used initially. Each breath should be delivered during 1 second, allowing the patient’s lungs to deflate between breaths. Thereafter, the rate of ten to 12 breaths per minute is maintained for as long as is necessary, with tidal volumes of approximately 700 mL. Delivering the breath during 1 second helps to prevent gastric insufflation. Melker et al. [150, 151] demonstrated airway pressures well in excess of those required to open the lower esophageal sphincter when quick breaths are used to ventilate patients. If the patient wears dentures, they are usually best left in place to assist in forming an adequate seal.
If air cannot be passed into the patient’s lungs, another attempt at opening the airway should be made. The jaw-thrust maneuver may be necessary. If subsequent attempts at ventilation are still unsuccessful, the patient should be considered to have an obstructed airway and attempts should be made to dislodge a potential foreign body obstruction.
Determining Pulselessness
In the adult, the absence of a central pulse is best determined by palpating the carotid artery (Fig. 22-6), although rarely the carotid pulse may be absent because of localized obstruction. If a pulse is not felt after 10 seconds of careful searching, chest compression is initiated, unless electrical countershock for ventricular arrhythmia or artificial pacing for asystole is immediately available. Although lay rescuers are no longer expected to perform a pulse check because it has been shown that checking the carotid pulse by a lay person is an inaccurate method of confirming the presence or absence of circulation [152], it is the position of the AHA that health care providers should continue
to be taught and to perform a pulse check. Therefore, rescuers should start CPR if the victim is unconscious (unresponsive), not moving and not breathing [153].
to be taught and to perform a pulse check. Therefore, rescuers should start CPR if the victim is unconscious (unresponsive), not moving and not breathing [153].
Chest Compression
Artificial circulation depends on adequate chest compression through sternal depression. Recent recommendations of CPR are “push hard at a rate of 100 compressions per minute, allow full chest recoil and minimize interruptions in chest compressions” [153]. The safest manner of depressing the sternum is with the heel of the rescuer’s hand at the nipple line, with the fingers kept off the rib cage (Fig. 22-7). It is usually most effective to cover the heel of one hand with the heel of the other, the heels being parallel to the long axis of the sternum. If the rescuer’s hands are placed either too high or too low on the sternum, or if the fingers are allowed to lie flat against the rib cage, broken ribs and organ laceration can result. Although it is important to allow the chest to recoil to its normal position after each compression, it is not advisable to lift the hands from the chest or change their position.
The rescuer’s elbows should be kept locked and the arms straight, with the shoulders directly over the patient’s sternum (Fig. 22-7). This position allows the rescuer’s upper body to provide a perpendicularly directed force for sternal depression. The sternum is depressed 1.5 to 2.0 inches (4 to 5 cm) at a rate of approximately 100 compressions per minute. In large patients, a slightly greater depth of sternal compression may be needed to generate a palpable carotid or femoral pulse. At the end of each compression, pressure is released, and the sternum is allowed to return to its normal position. Equal time should be allotted to compression and relaxation with smooth movements, avoiding jerking or bouncing the sternum. Manual and automatic chest compressors are available for fatigue-free sternal compression and are used by some EMS crews and emergency room and ICU personnel. Whether using hinged manually operated devices or compressed air-powered plungers, the rescuer must be constantly vigilant about proper placement and adequacy of sternal compression. An experimental device using a plungerlike suction device may improve flow by facilitating sternal rebound and thoracic vascular filling; this has been referred to as active compression-decompression CPR [108, 109].
Ventilation and sternal compression should not be interrupted except under special circumstances. Warranted interruptions include execution of ACLS procedures (e.g., endotracheal intubation, placement of central venous lines) or an absolute need to move the patient. Even in these limited circumstances, interruption of CPR should be minimized. In a retrospective analysis of the VF waveform, interruption of CPR was associated with the decreased probability of conversion of VF to another rhythm [154].
Two-Rescuer CPR
The combination of artificial ventilation and circulation can be delivered more efficiently and with less fatigue by two rescuers. One rescuer, positioned at the patient’s side, performs sternal compressions while the other, positioned at the patient’s head, maintains an open airway and performs ventilation. This technique should be mastered by all health care workers called on to perform CPR. Lay people have not been routinely taught this method, in the interest of improving retention of basic skills. The compression rate for two-rescuer CPR, as for one-rescuer CPR, is approximately 100 compressions per minute. The new recommendation of the compression to ventilation ratio is 30 to 2.
In an animal model of cardiac arrest, a compression-ventilation ratio of 30 to 2 was associated with significantly shorter time to return of spontaneous circulation [155]. The only exception to this recommendation is when two health care workers are providing CPR to a child or infant (except newborns); in this instance, a 15 to 2 compression to ventilation ratio should be used [153]. When the rescuer performing compressions is tired, the two rescuers should switch responsibilities with the minimum possible delay.
In an animal model of cardiac arrest, a compression-ventilation ratio of 30 to 2 was associated with significantly shorter time to return of spontaneous circulation [155]. The only exception to this recommendation is when two health care workers are providing CPR to a child or infant (except newborns); in this instance, a 15 to 2 compression to ventilation ratio should be used [153]. When the rescuer performing compressions is tired, the two rescuers should switch responsibilities with the minimum possible delay.
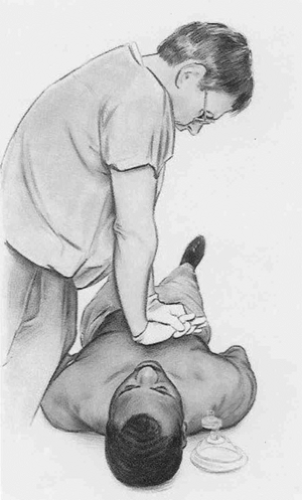 FIGURE 22-7. External chest compression. Proper position of the rescuer: place heel of hand on the breast bone at the nipple line with shoulders directly over the patient’s sternum and elbows locked. [From BLS for Healthcare Providers, American Heart Association, 2006, with permission. Copyright 2006, American Heart Association.]
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|