PURPOSE OF PROCEDURE
Cardiac pacing serves to maintain or restore myocardial depolarization and thus ensure adequate cardiac output. In the ED, pacing is performed therapeutically to correct an ongoing rhythm disturbance or in anticipation of the onset of a conduction problem with hemodynamic impact.1
Indications for emergency pacing are listed in Table 33-1.
| Indication | Comments |
|---|---|
| Symptomatic or hemodynamically unstable bradycardia/AV block | Symptoms include hypotension, change in mental status, angina, and pulmonary edema. Pharmacologic therapy may be used to temporize while preparing to pace. |
| Severe sick sinus syndrome with prolonged asystole (generally >3 s) and syncope | — |
| Ventricular standstill due to complete heart block or Mobitz type II AV block | — |
| Torsade de pointes | Overdrive pacing. |
| Recurrent monomorphic ventricular tachycardia | Overdrive pacing. The technique is limited by: Maximum pacing rate of the pacing device (usually 180 beats/min). Potential of accelerating the ventricular tachycardia and inducing ventricular fibrillation. |
| Unstable supraventricular tachycardia | Overdrive pacing should only be used after pharmacologic intervention and cardioversion have failed. |
The indications for emergency cardiac pacing are found in chapter 18, “Cardiac Rhythm Disturbances.”
GENERAL EQUIPMENT
All cardiac pacemakers deliver an electrical stimulus to the heart by electrodes that cause depolarization and subsequent cardiac contraction.2 The modern pacemaker only stimulates the heart chamber if it does not recognize (sense) intrinsic electrical activity from that chamber after a selected time interval. Impulses are delivered to either the atria or ventricles, or to both.
Components of a cardiac pacemaker include:
Pulse generator
Electronic circuitry for sensing and pacing
Lead system that connects the pulse generator to the electrode(s) and stimulates the myocardium
Relevant clinical details of these components are listed in Table 33-2.
| Pacemaker Type | Pulse Generator Location | Electrode Location |
|---|---|---|
| Transcutaneous | External | Skin of anterior chest wall and back or Anterior chest wall below right clavicle and apex |
| Transvenous | External | Venous catheter with tip in right ventricle and/or right atrium |
| Transesophageal | External | Esophagus |
| Epicardial | External or Internal | Epicardium Electrodes are usually placed on heart’s surface during surgery |
| Permanent | Internal (subcutaneous in the prepectoral region) | Venous or epicardial |
TRANSCUTANEOUS PACING
Transcutaneous pacing is the emergency technique of choice because of its easy application. It uses externally applied electrodes to deliver an electric impulse directly across the intact chest wall to stimulate the myocardium. Transcutaneous pacers differ from standard pulse generators in several important ways. The pulse duration of the stimulating impulse is longer and the current output higher than in internal pacing. Muscle contraction (usually the chest wall or diaphragm) is notable during pacing, especially at high outputs, and may be painful. Severe twitching makes palpation of the radial, carotid, or femoral pulse difficult. Cardiac monitoring with standard ECG monitors is difficult due to interference from the large current outputs that create large-amplitude pacing spikes. Most of the newer transcutaneous pacing units have a monitor that filters pacing spikes, allowing simultaneous monitoring.
There is little risk of electrical injury to healthcare providers during transcutaneous pacing. The electrodes are insulated, and closed chest compressions can be done over pads while pacing. Inadvertent contact with the active pacing surface results only in a mild shock.
Table 33-3 lists the equipment needed to perform transcutaneous pacing.
If time and conditions allow, explain the procedure to the patient and administer IV sedation and analgesia.
Apply the external pacing pads as shown in Figure 33-1. The same pads and electrodes are used for pacing, cardioversion, and defibrillation in most of the newer defibrillator units. If separate defibrillator pads or paddles are used, place them at least 2 to 3 cm from the pacing pads.
FIGURE 33-1.
Placement of the transcutaneous pacing electrodes. A. Anterior (negative) electrode position centered over the cardiac apex. B. Anterior (negative) electrode position centered over the V3 lead position. C. Posterior (positive) electrode position. [Reproduced with permission from Doukky R, Rajanahally RS: Transcutaneous cardiac pacing, in Reichman EF, Simon RR (eds): Emergency Medicine Procedures. Figures 20-2 and 20-3. Copyright © 2004. The McGraw-Hill Companies, Inc., all rights reserved.]
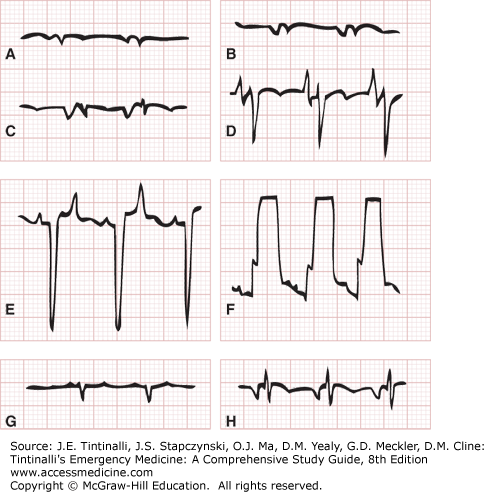
FIGURE 33-2.
Typical ECG tracings seen with a transvenous pacing catheter within the different anatomic sites. A. The subclavian or internal jugular vein. B. The superior vena cava. C. The high right atrium. D. The low right atrium. E. Free-floating in the right ventricle. F. Abutting the right ventricular wall. G. The inferior vena cava. H. The pulmonary artery. [Reproduced with permission from Wilson DD, Reichman EF: Transvenous cardiac pacing, in Reichman EF, Simon RR (eds): Emergency Medicine Procedures. Figure 22-6. Copyright © 2004. The McGraw-Hill Companies, Inc., all rights reserved.]
In bradyasystolic arrest, turn the stimulating current to maximum output and then decrease the output after capture is achieved; after restoring pulses, you may titrate energy to a level just above loss of capture. In a patient with a hemodynamically compromising bradycardia outside of cardiac arrest, slowly increase the output from the minimum setting until capture is achieved—usually between 50 and 100 mA. Continue pacing at about 1.25 times the threshold of initial electrical capture.
Transcutaneous pacing may be fixed rate (asynchronous) or demand (synchronous). Asynchronous pacing delivers an electrical impulse at a regular interval without regard to intrinsic cardiac pacemaker activity. This creates the potential risk of precipitating a dysrhythmia if the pacing stimulus occurs during the vulnerable period of ventricular repolarization. While many state a preference for synchronous pacing, there are little outcome or safety data to support that preference.
Assess capture using the ECG on the filtered monitor of the pacing unit. Look for the presence of a consistent ST segment and T wave after each pacer spike. Palpate for carotid and femoral pulses. Bedside US can be used to assess external pacer capture. If these appear favorable, assess blood pressure by cuff or arterial catheter.
Failure to capture with transcutaneous pacing may be related to faulty electrical contact, electrode placement, patient size, or underlying pathology. Recheck the lead connections, skin–electrode contact, and electrode placement. On occasion, pneumothorax, pericardial effusion or tamponade, severe myocardial ischemia, and metabolic derangements limit capture. No clinical myocardial damage results from properly performed transcutaneous pacing. Unless an easily resolved trigger exists, arrange for temporary transvenous pacing as soon as possible since ongoing pacing is likely needed.
TRANSVENOUS PACING
The indications for transvenous pacing are the same as for other methods of cardiac pacing.
Gather all equipment needed, including that to insert a central venous catheter (see chapter 31, “Vascular Access.”) Resuscitation equipment and drugs, and the pacing needs listed in Table 33-4.
Central catheter kit—introducer sheath must be one size larger than the pacer catheter Flexible transvenous cardiac pacing catheter Pacemaker generator and battery (and spare battery) Cardiac monitor Insulated connecting wire with alligator clamps at both ends |
You should know the equipment and practiced or done the procedure before starting. If conditions permit, explain the procedure to the patient and obtain informed consent. Next, identify the access site and approach and position the patient. The primary sites of catheter insertion in the ED are the right internal jugular vein (preferred) and the left subclavian vein. The right internal jugular vein allows a relatively straight line of access through the superior vena cava and right atrium into the right ventricle.
The steps for transvenous pacemaker insertion are listed in Table 33-5.
| Step | Comments |
|---|---|
| 1. Gown in standard sterile fashion. | Use sterile gloves and gown. Wear mask and hair covering. |
| 2. Identify vessel using either US guidance or landmarks. | — |
| 3. Prep and drape patient using standard sterile procedure. | Prep a wide area in case initial attempts fail and an alternate site is needed. Prep the entire ipsilateral neck and upper chest when preparing to insert an internal jugular or subclavian catheter. |