Chapter 42 Burns
Deaths from fires and burns are the fifth most common cause of unintentional injury deaths in the United States and the third leading cause of fatal home injury.1,2 In 2008 someone in the United States died in a fire approximately every 158 minutes and was injured in a fire every 31 minutes.3 Burn injuries account for an estimated 700,000 visits to the emergency department (ED) annually; of these, 45,000 require hospitalization in a burn center.4 The high-risk, low-frequency exposure to burn-injured patients continues to be anxiety provoking to many emergency personnel. However, proper management in the ED is an essential first step in appropriately managing burn care and can have a significant impact on patient outcomes.
Etiology
Flame is the predominant cause of burns in patients admitted to burn centers, particularly in the adult age group.5 Thirty percent of all burns requiring admission to the hospital are caused by scalding resulting from hot liquids.5 Burn injury is caused by more than fire and scald, however. A burn can also occur from thermal exposure, chemicals, electric current, and radiation, as well as from inhalation of heat or smoke. Table 42-1 lists various types of burns and their possible etiologies.
TABLE 42-1 TYPES OF BURN INJURIES
| TYPE OF BURN | EXAMPLES |
|---|---|
| Thermal | |
| Scald | Hot liquids (water, oil, beverages, bath water) |
| Flame | Flammable fabrics, campfire |
| Flash | Furnace blast, gasoline explosion |
| Contact | Hot burner, clothes iron |
| Tar | Work-related injuries |
| Steam | Radiator, steam pipes, hot water with cooking |
| Electrical | |
| Alternating current | Commercial appliances |
| Direct current | Car batteries, lightning |
| Chemical | |
| Alkaline | Cleaning supplies, household plumbing agents |
| Acid | Sulfuric acid, hydrofluoric acid |
| Radiation | Exposure to ultraviolet light (sun, tanning booths), radiation therapy, radioactive fallout, radiographs |
| Friction | |
| Tissue abrasion | “Road rash,” as a result of motorcycle/bicycle crash |
Pathophysiology
The body’s response to burn injury varies with the degree of tissue damage, cellular impairment, and fluid shifts. Damage to burned tissue causes the release of mediators that initiate an inflammatory response. The release of these mediators is associated with vasodilation and increased capillary permeability, resulting in intravascular fluid loss and tissue edema.6
Burn shock is the most significant component of burn pathophysiology. Direct thermal injury can result in dramatic changes in the microcirculation, particularly the increase in capillary permeability throughout the body. Burn shock is both hypovolemic shock and cellular shock.5 Table 42-2 summarizes the pathophysiology of hypovolemic burn shock. Table 42-3 describes the extensive effects of burn injury on the body.
TABLE 42-2 PATHOPHYSIOLOGY OF BURNS
TABLE 42-3 IMPACT OF BURN INJURY ON BODY SYSTEMS
Triage Assessment
• Remove all clothing from any burned area, including shoes and jewelry that may retain heat.
• Flush all areas of the body that came in contact with chemicals with copious amounts of water.
• Tar that is part of burned, blistered tissue should be removed. Applying ointments, such as polymicrobial antibiotic ointment or petroleum jelly, or common household agents such as mayonnaise promotes tar removal.4
Primary Assessment
Airway and Breathing
Inhalation Injury
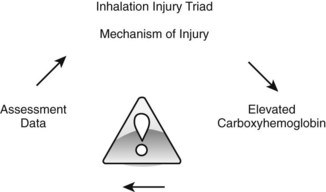
Assessment for inhalation injury should be completed on every burn patient on arrival at the ED. An inhalation injury cannot be ruled out until the components of the Inhalation Injury Triad have been considered (Fig. 42-1).
Mechanism of Injury
• Assess for burns that occurred in an enclosed space with heat or smoke exposure for an extended period of time. The likelihood of airway injury is greater in an enclosed space than it is outdoors.
• Consideration should be given to the toxins that can be produced when objects are burning in an enclosed space.
• Damaged cilia in the airway result in an inability to clear secretions and bacteria manifested by a tracheal bronchitis.7
Elevated Carboxyhemoglobin.
Carboxyhemoglobin level may be as high as 50% to 70%. See Table 42-4 for signs and symptoms of elevated carboxyhemoglobin level.
TABLE 42-4 SIGNS AND SYMPTOMS OF ELEVATED CARBOXYHEMOGLOBIN
| Carboxyhemoglobin Saturation Percentage and Symptoms | |
| 5–10 | Mild headache and confusion |
| 11–20 | Severe headache, flushing, dilation of skin vessels |
| 21–30 | Disorientation, nausea |
| 31–40 | Irritability, dizziness, vomiting, prostration |
| 41–50 | Tachypnea, tachycardia, prostration |
| 51–69 | Coma, seizures, convulsions, Cheyne-Stokes respiration. Death is possible |
| 70–80 | Slowing/stopping of breathing, death within hours |
| 80–90 | Death in less than 1 hour |
| 90–100 | Death within a few minutes |
Data from Essig, M. G. (2008, March 18). Carbon monoxide (CO). Retrieved from http://firstaid.webmd.com/carbon-monoxide-co
Carbon Monoxide Poisoning
• Carbon monoxide binds to hemoglobin 200 times more effectively than oxygen does; tissue hypoxia occurs if sufficient hemoglobin is bound to carbon monoxide.9
• The skin of a patient with high carbon monoxide levels may appear cherry red in color, but this has been observed in only 50% of patients with severe carbon monoxide poisoning.
• Although the oxygen content of the blood is diminished, the amount of oxygen dissolved in the plasma (PaO2) is unaffected by carbon monoxide poisoning; the arterial blood gas will appear normal.
• Pulse oximetry detects saturated hemoglobin and does not measure carbon monoxide, so the oxygen saturation usually appears normal.
• A serum carboxyhemoglobin level must be determined in any patient with potential exposure to carbon monoxide during a fire.
Management of Carbon Monoxide Poisoning or Inhalation Injury
• Immediately administer 100% oxygen if this has not been accomplished by EMS personnel prior to arrival at the ED.
• If the airway is compromised in any way, endotracheal intubation should be performed and difficult airway supplies should be available. See Table 42-5 for considerations for early intubation.
• Intubation can often be difficult in this patient population because of swelling of the face and hypopharynx.9
TABLE 42-5 CONSIDERATIONS FOR EARLY INTUBATION