Key Clinical Questions
Introduction
Bradyarrhythmia is a common finding in hospitalized patients. It can be of minimal prognostic significance or can indicate a serious cardiac condition that requires immediate attention. Broadly speaking, bradyarrhythmias are caused by depression of sinus node activity or conduction system blocks. Symptoms depend on the patient’s co-morbidities, the anatomical basis for the block(s), and the location of the subsidiary pacemaker which must take over to maintain cardiac output. Clinicians must analyze historical data, and examine the patient for evidence of hypoperfusion and electrocardiographic data to determine the likelihood that the rhythm will deteriorate into a worsening bradycardia or ventricular asystole.
Sinoatrial Node Dysfunction
A heart rate below 60 beats per minute defines bradycardia. Resting heart rates vary among normal individuals and depends upon age and level of conditioning. One study demonstrated that resting heart rates can range from 46 to 93 beats per minute in males and 51 to 95 beats per minute in females. Additionally, heart rate varies with time of day. Heart rate during sleep may decrease between 14 and 24 beats per minute (bpm) on average, depending upon age. Due to this variability, it is difficult to fully assess the incidence and prevalence of bradycardia in the general population. Asymptomatic bradycardia portends no adverse prognostic significance in healthy individuals, including those over 40 years old.
|
Sick sinus syndrome, or sinus-node dysfunction, however, does impact morbidity and mortality. The prevalence of sick sinus syndrome is estimated at 1 in 600 patients over 65 years old. Many patients with sick sinus syndrome have an elevated risk of cardiovascular events, including syncope, heart failure, and atrial fibrillation. Mortality for untreated patients with sick sinus syndrome ranges from 5 to 10% at 1 year to 25 to 30% at 5 years.
Even a significant sinus bradycardia may not produce symptoms, depending on an individual’s age, physical conditioning, and co-morbidities. In these patients the bradycardia may be identified as an ECG abnormality (sinus bradycardia, sinus arrest, exit block, or alternating with a tachyarrythmia). The elderly and patients with co-existing cardiopulmonary disease are more likely to develop symptoms related to low perfusion (presyncope, fatigue, weakness, confusion) or to associated tachycardia (palpitations, angina, heart failure). See (Table 127-1).
| Asymptomatic Patient | Symptomatic Patient |
|---|---|
| The patient likely remains asymptomatic if he or she has the ability to increase stroke volume. Cardiac output equals stroke volume times heart rate (CO = SV × HR). Therefore, if an individual is able to compensate for a lower heart rate by increasing stroke volume, that person will remain asymptomatic. A good example of this is a well-trained athlete, whose resting heart rates may be profoundly bradycardic but who has no symptoms referable to the heart rate because of increased stroke volume. | If a patient does not have the ability to compensate for the decreased heart rate, blood pressure (SV x HR x systemic vascular resistance) will fall. The patient may therefore develop nonspecific symptoms often chronic in nature, consistent with the patient’s inability to compensate for a decreased heart rate. A vagal stimulus can decrease sinus node automaticity or cause decreased impulse transmission across the atrioventricular node. In this manner, an individual can develop specific symptoms—usually manifesting as syncope. |
Vascular supply and cardiac innervations help determine etiology and pathophysiology of bradyarrhythmias (Table 127-2). The sinus node, which receives flow from the sinus-node artery, spontaneously depolarizes to initiate the cardiac cycle. The sinus-node artery most often originates from the right coronary artery (RCA), but may also branch from the left circumflex (LCx) artery. Once the sinus node depolarizes, the impulse propagates through the right atrium to the atrioventricular (AV) node. The AV node, supplied by the AV nodal artery usually arises from the RCA, but as with the sinus node, may originate from the circumflex artery. Impulses then pass from the AV node to the bundle of His, which separates into the right and left bundle branches. Ischemia of the RCA or LCx can lead to SA or AV node dysfunction and subsequent bradycardia.
| Etiology | Example | |
|---|---|---|
| Intrinsic | ||
| Inflammatory |
| |
| Iatrogenic |
| |
| Aging (idiopathic conduction system fibrosis) |
| |
| Coronary artery disease |
| |
| Infiltrative diseases |
| |
| Collagen vascular diseases |
| |
| Myotonic muscular dystrophy and Friedreich’s ataxia | ||
| Familial and congenital heart disease | ||
| Infectious |
| |
| Extrinsic | ||
|
| |
| Hypothyroidism | ||
| Hypothermia | ||
| Medications |
| |
| Increased intracranial pressure | ||
The innervation of the conduction system is balanced between sympathetic and parasympathetic control. Increases in parasympathetic tone decrease sinus node automaticity and slow AV nodal conduction. Therefore, a vasovagal response to external stimuli may cause a profound bradycardia due to significant parasympathetic response (Table 127-2).
In general, patients with bradycardias require emergent treatment if
The distinction between extrinsic and intrinsic causes is important because extrinsic causes are often reversible and should be corrected before consideration of permanent pacemaker therapy. |
Atrioventricular Node Dysfunction
First-degree AV block, evidenced by PR interval prolongation greater than 200 msec is rare in younger patients. It occurs more frequently in patients with heart disease and the incidence of first-degree AV block may increase by nearly 10% in older patients with heart disease. Recent evidence suggests a slightly higher mortality risk in patients with first-degree AV block. Mobitz type I second-degree AV block (known as Wenckebach) is a normal variant in younger individuals, and has no known pathologic consequences. Mobitz type II second-degree AV block, however, does have increased risk of morbidity and mortality and may require aggressive management similar to third-degree AV block. The incidence of both Mobitz type I and type II second-degree AV block increases with the presence of heart disease. In third-degree AV block, there is no AV conduction due to block at the nodal or infra nodal levels. An escape pacemaker paces the ventricles at a slower rate than the atrial rate. Acquired third-degree heart block (ie, complete heart block) is typically seen in older patients with heart disease.
First-degree and Mobitz I AV blocks are typically asymptomatic, while higher-grade AV blocks commonly present with dizziness, presyncope, and syncope. Patients may develop signs and symptoms consistent with heart failure.
AV node dysfunction occurs when the electrical impulse moving from the atria to the ventricles is delayed or completely interrupted. This delay may be caused by an anatomic abnormality or a functional impairment and can be transient or permanent in nature. First-degree AV block occurs when conduction occurs slowly through the AV node (manifesting as a PR interval > 200 msec on ECG), while ventricular depolarization occurs without missed “beats” (Figure 127-1).
Classically first degree AV block is intranodal and associated with a prolonged AH (Atrial His) apical electrogram. The site of block is usually in the AV node, but may be located in the atria, AV node bundle of His, or in the His-Purkinje system. Beta-blockers, calcium channel blockers, and digitalis typically prolong the AH interval as does increased vagal tone.
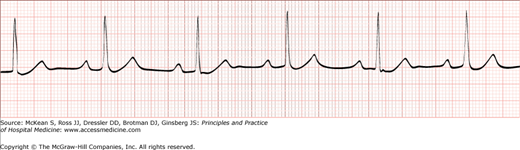
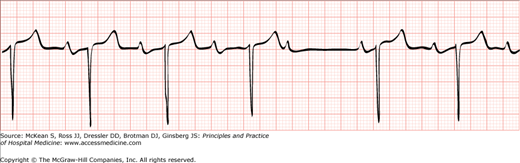
In second degree AV block conduction of electrical impulses from the atrium to ventricle intermittently fail. The ECG pattern of Type I second-degree heart block—the progressive lengthening of the PR interval, shortening of the R-R interval, and a pause less than two times the immediately preceding RR interval—likely arises because of decremental conduction of electrical impulses in the AV node (Figure 127-2). Type II second-degree AV block commonly occurs in the distal or infra-His conduction system. It is associated with bundle branch block and is more likely to progress to higher grades of heart block than Type I. The PR interval in Mobitz II pattern is constant, and while it may be slightly prolonged, it is often normal. Eventually an atrial impulse is not conducted to the ventricles, leading to a dropped beat.
Figure 127-2
Second-degree atrioventricular (AV) block, Mobitz type I. Second-degree AV blocks are characterized by inconsistent conduction of atrial impulses to the ventricles. In Mobitz type I second-degree AV blocks, the PR intervals vary, lengthening in duration until there is a nonconducted P wave (occurs following the fourth P wave in this rhythm strip).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree