Brachial Plexus Blocks
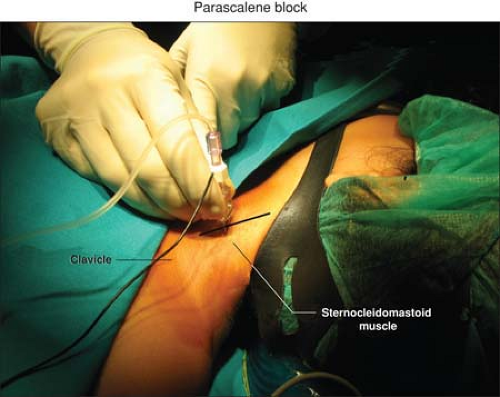
A. Parascalene Block
Giorgio Ivani
Valeria Mossetti
The parascalene approach is the safest supraclavicular approach to the brachial plexus, aiming at penetrating the interscalene space at a distance from the apical pleura, the great vessels and nerve of the neck, the stellate ganglion, and the spinal canal. In children the use of the parascalene block is safer and has lower incidence of complications than the other blocks (interscalene and infraclavicular block).
The brachial plexus is located at a depth of 7 to 20 mm from the skin.
This technique provides excellent analgesia to the upper part of the arm, but in 50% of patients the lower branches of the cervical plexus are also blocked.
Complications include:
Horner syndrome (ptosis of the eye, miosis, anophthalmos, hyperemia of the conjunctiva, hyperthermia, anhidrosis of the face) for the stellate ganglion block.
Because of the risk of respiratory failure linked to bilateral phrenic paralisys given by bilateral block, this block is contraindicated in cases of acute or chronic respiratory insufficiency or whenever it is necessary a bilateral block.
Vessel puncture of the large blood vessel of the neck (carotid artery and internal jugular vein) or of the vertebral artery.
Pneumothorax.
Epidural and intrathecal injections are avoided by using this technique.
If the position of the needle is too lateral, causing the stimulation of the suprascapular nerve (levator scapulae muscle), retract the needle and advance more ventral; if the position is too ventral, causing the stimulation of the phrenic nerve (unilateral singultus), retract the needle and advance more lateral.
Suggested Readings
Dalens B, Vanneuville G, Tanguy A. A new parascalene approach to the brachial plexus in children: comparison with the supraclavicular approach. Anesth Analg 1987;66:1264–1271.
McNeely JK, Hoffman GM, Eckert JE. Postoperative pain relief in children from the parascalene injection technique. Reg Anaesth 1991;16:20.
Vongvises P, Beokhaimook N. Computed tomographic study of parascalene block. Anaesth Analg 1997;84:379.
B. Axillary Block
Giorgio Ivani
Valeria Mossetti
In infants and children, it is enough to block one of the components of the plexus to obtain a complete anesthesia of the hand.
The complication rate of the axillary block is virtually nil, whatever the technique used. The single described complication is hematoma if the axillary artery is injured from the puncture being too deep.
There are no specific contraindications except severe lymphadenopathy.
Suggested Readings
Carre P, Joly A, Cluzel Field B. Axillary block in children: single or multiple injection? Paediatr Anaesth 2000;10(1):35–39.
Dalens B. Regional anaesthesia in infants, children and adoloscents. Baltimore: Williams & Wilkins, 1995:550.
Fisher WJ, Bingham RM, Hall R. Axillary brachial plexus block for perioperative analgesia in 250 children. Paediatr Anaesth 1999;9:435.
C. Use of Paravertebral Blockade in Children
Per-Arne Lonnqvist
Introduction
In order to map the innervation of the intrathoracic and intraabdominal organs Sellheim and Läwen in the beginning of the nineteenth century were the first to inject local anesthetics in the paravertebral space (PVS) and the technique was later used by Kappis (1919) to provide surgical analgesia for abdominal surgery. Deposition of local anaesthetics in the PVS will lead to strict unilateral anaesthesia of one or more adjacent dermatomes (Fig. 47-3) and the main indications for paravertebral nerve block (PVB) are unilateral thoracic or abdominal surgical procedures (Table 47-1).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree