Chapter 32 Bite and Sting Emergencies
Between 2001 and 2005 approximately 94,552 instances of animal bites and stings were reported in the United States.1 Most are successfully managed medically, but death can and does occur. More than half (52%) of these deaths are from insect bites and stings, followed by 30% from snakebites and 13% from spider bites.2 Other considerations are potential infection and systemic complications.
Rabies
Rabies, one of the world’s oldest diseases, is most commonly transmitted through the saliva of an infected mammal but is also known to spread via the airborne route. There are an estimated 55,000 deaths worldwide each year from rabies.3 In the United States, however, prevention measures have resulted in only one or two actual cases developing in the 16,000 to 39,000 individuals exposed to potentially rabid carnivores and bats.4 The Centers for Disease Control and Prevention (CDC) reported in 2007 that the canine strain of rabies has been eliminated in the United States, and most human incidents of rabies are now the result of exposure to wildlife such as bats, raccoons, skunks, and foxes.4
Signs and Symptoms
• Initial stage rabies includes paresthesias, pain, or itching at the bite site. This is thought to be related to viral replication and may progress over several days to a week. The incubation period is usually 1 to 3 months but can vary from days to years.3
• Prodrome stage rabies includes nonspecific findings such as headache, fever, runny nose, sore throat, myalgias, and gastrointestinal symptoms. The virus progresses along the peripheral nervous system toward its ultimate destination: the central nervous system.
• Acute, progressive encephalitis includes:
Postexposure Prophylaxis
Postexposure prophylaxis is imperative (Table 32-1). For those who have not previously been exposed, the rabies vaccine human rabies immunoglobulin provides rapid, passive immunity. When the rabies vaccine is administered properly, detectable rabies virus neutralizing antibodies have been shown to develop in approximately 7 to 10 days.4 These antibodies persist for several years. Reactions to prophylactic therapies are rarely severe.4
TABLE 32-1 RABIES POSTEXPOSURE PROPHYLAXIS
| THOSE NOT PREVIOUSLY VACCINATED FOR RABIES (i.e., GENERAL PUBLIC) | THOSE PREVIOUSLY VACCINATED FOR RABIES (i.e., VETERINARIANS) |
|---|---|
| Immediate aggressive cleaning and scrubbing of wound with virucidal agent (rinse with water or saline and dry after). | Immediate aggressive cleaning and scrubbing of wound with virucidal agent (rinse with water or saline and dry after). |
| Administer human rabies immunoglobulin (20 IU/kg or 0.133 mL/kg). If anatomically feasible, inject as much as possible directly into proximal area of wound (virus will travel along nerve tracts toward the central nervous system). Any remaining volume is administered intramuscularly at a site distal to the vaccine site. | Do not administer rabies immunoglobulin. |
| Administer human diploid cell vaccine or purified chick embryo 1 mL dose on days 0, 3, 7, and 14.a | Administer human diploid cell vaccine or purified chick embryo 1 mL dose on days 0 and 3.a |
Note: More detailed information is available from Centers for Disease Control and Prevention.
a Mitka, M. (2010). CDC advisors suggest streamlining postexposure prophylaxis for rabies. Journal of the American Medical Association, 303(16), 1586.
Data from Centers for Disease Control and Prevention. (2010). Use of a reduced (4-dose) vaccine schedule for postexposure prophylaxis to prevent human rabies: Recommendations of the Advisory Committee on Immunization Practices. MMWR Recommendations and Reports, 59(RR-2), 1–9.
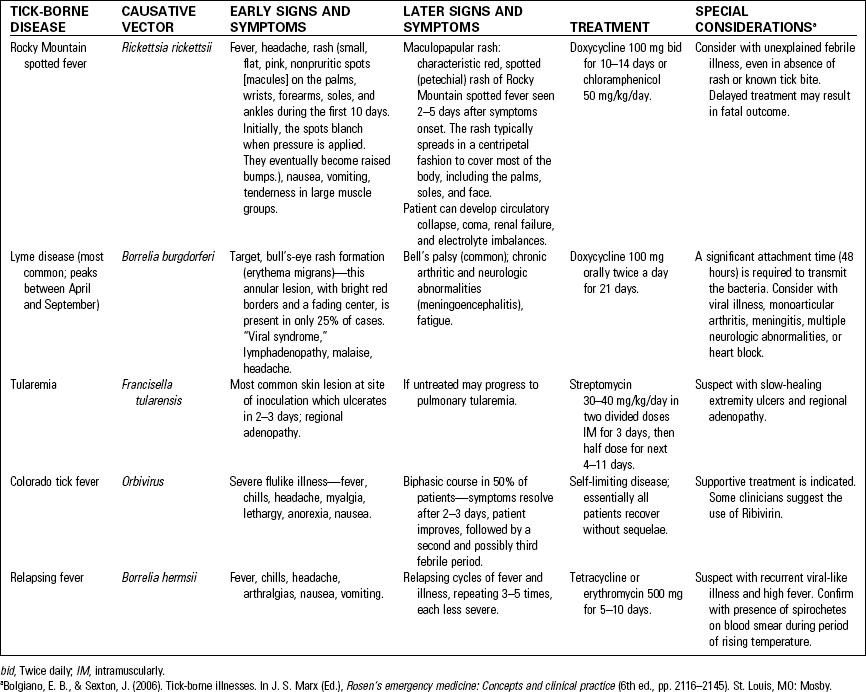
Tick-Borne Illnesses
Table 32-2 lists a sampling of common tick-borne illnesses that occur in the United States. In addition to spreading infection, certain ticks contain a neurotoxin that can induce tick paralysis. This disease is characterized by a descending paralysis that resembles Guillain-Barré syndrome. Paralysis quickly resolves when the tick is removed.
Tick Removal5,6
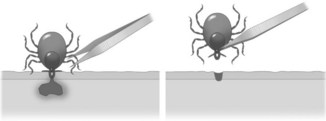
Ticks should be removed as soon as possible to decrease the amount of time for microorganisms to be transferred to the host. Guidelines for safe tick removal are included in Table 32-3 and depicted in Figure 32-1. Avoid squeezing or crushing the tick, as this may cause the inadvertent release of the tick’s internal contents. Avoid handling the tick. Occasionally, the tick may be sent to a local laboratory or health department for analysis and evaluation.
Prevention
Avoidance of tick habitats is the best prevention measure. Table 32-4 lists ways to avoid tick exposure that can be included in patient discharge instructions.
TABLE 32-4 AVOIDING TICK-BORNE ILLNESS
Snakebites
Only about 5 to 10 individuals die annually in the United States as a consequence of a snakebite.2 The actual incidence of snakebites is estimated at 45,000, with 7000 to 8000 from venomous snakes.2 Most bites occur when handling, teasing, or playing with snakes and 40% of persons bitten have a blood alcohol level greater than 0.1%.7 Around 85% of bites are on the fingers or hand and 15% involve the foot or ankle.7