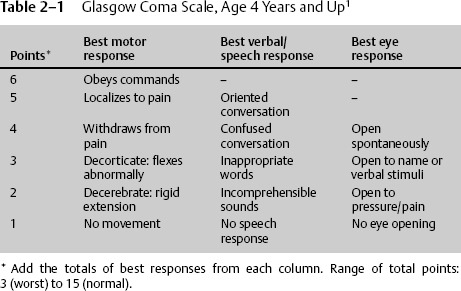
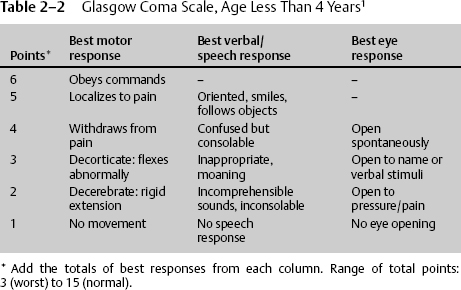
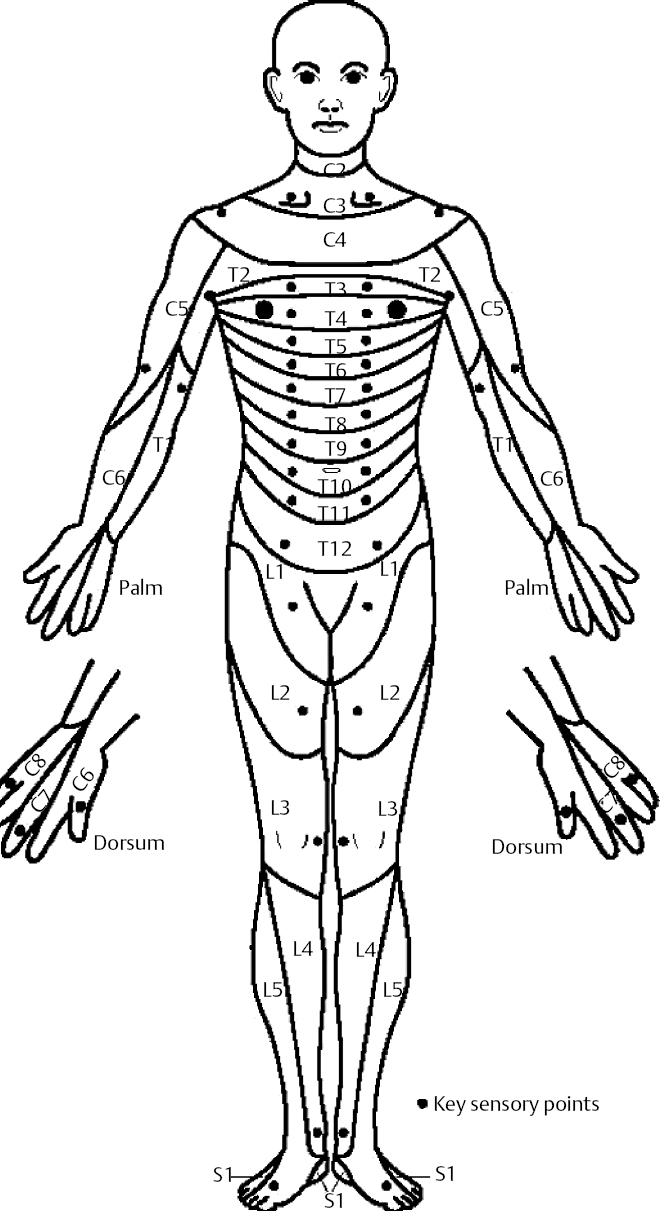
Section I John D. Cantando, Daniel Hutton, and Dan Miulli Patients admitted to the neurosurgical intensive care unit (NICU) are among the most critically ill and unstable. Many are admitted for traumatic brain injury (TBI), aneurysmal subarachnoid hemorrhage, spinal cord injury (SCI), postoperative craniotomies, and other pathologies. With the advent of advanced neuroimaging techniques, the physical examination is less emphasized in training and community settings alike. Though elegant and easily obtainable, imaging techniques sacrifice time in a potentially true surgical emergency. Physical examination should guide the appropriateness of these expensive tools. The variety of pathology in the NICU demands a consistent, reliable monitoring modality for physicians, consultants, and nurses. Numerous studies exist regarding the examination of neurologic patients. In the NICU, like elsewhere, the art of medicine should never be underestimated. While in many NICU patients, the neurologic exam is rendered more difficult by sedation, intubation, and paralytics, leaving the neurosurgeon and his or her team to rely on invasive monitoring data, serial neuroimaging, and intermittently withholding sedation to assess the patient, observation is still an important component of the patient’s examination. For example, the obtunded or comatose patient breathing rhythmically in a specific pattern offers important lesion-localizing clues to the astute neurosurgeon. Observation of asymmetric spontaneous movements of the extremities, or change in their frequency, can be another clue to evolving brain or spinal cord lesions. In the smaller number of awake patients in the NICU, the neurosurgeon has greater leeway to observe and converse with the patient. In these patients, observing whether they show any subtle localizing signs may betray early and enlarging focal lesions in the brain. For example, the patient who complains of a focal headache and who holds his hand over his head in the same area repeatedly and on request is able to point to a specific area of his head as the site of most discomfort, may be helping the neurosurgeon with localization of an existent or developing lesion (tumor, hematoma, abscess, edema, etc.). This ability of the awake patient to localize the lesion for the neurosurgeon by effectively putting a finger on where it hurts the most, or showing the “Siddiqi sign,” comprises an observation and communication component of the neurologic exam with significant inter-observer reliability (in patients without the confounding variables of recent soft-tissue bruising or incision on the head). The value of focality of the Siddiqi sign is lost when the patient complains of a global headache, or pain “all over.” A conscious attempt should be made in the NICU to not dismiss the initial observation of the patient in favor of exhaustive analyses of numerous data sets generated by an ever-increasing number of invasive monitoring techniques. Since the landmark paper by Teasdale and Jennett in 1974,1 a more standardized method to assess level of consciousness has quickly become the principle component of the neurologic exam (Table 2–1). The two components to consciousness are arousal and content. Arousal hinges on one’s ability to awaken and maintain a sustained level of alertness. Content is conferred by appropriate speech response to questioning. Anxiolytics, sedatives, and paralytics are often used in the NICU and should be noted in the exam. The physician must also consider the half-life, pharmacokinetics, pharmacodynamics, and potential medical conditions in which altered metabolism or excretion exists. The pediatric population in the NICU often presents a more difficult assessment. The modified Glasgow Coma Scale (GCS) for pediatrics is a standardized, reproducible system used to examine patients less than 4 years of age (Table 2–2). Herniation results from abnormal intracranial pressures on specific portions of the brain. Several clinical syndromes result from specific portions of brainstem compression. Uncal herniation is most common, resulting from increased supratentorial intracranial pressure, causing compression of the medial portion of the temporal lobe and the uncus through the tentorial incisura. This syndrome is typically seen with head trauma as an expanding hematoma. Accompanying this is a third nerve palsy from direct entrapment. The first sign of uncal herniation is a unilateral enlarging pupil. Other signs include Cushing’s triad—bradycardia, hypertension, and respiratory depression. These signs should be considered ominous, and further rapid investigation should ensue. The airway should be protected, intracranial pressure monitored, and mass-occupying lesions evacuated surgically. Without treatment, these patients progress to brain death in a typically rapid manner. Because of many years of discrepancy, standardizations for determination of brain death now exist.2–7 Central herniation is associated with diffusely elevated supratentorial pressure. This syndrome is more often associated with tumors and has a slower progression. Each stage corresponds to a worsening magnitude of diencephalic and brainstem compression. The diencephalic stage consists of slight lethargy, small reactive pupils, slightly disconjugate gaze, Cheyne-Stokes respirations, and possibly Parinaud’s syndrome. The upper pons stage consists of sustained regular hyperventilation, fixed midposition pupils, and internuclear ophthalmoplegia. Patients often are posturing—decorticate due to disinhibition of the corticospinal tracts, or decerebrate due to unopposed vestibulospinal tracts. The lower pontine and upper medulla stage is characterized by a more irregular (ataxic) breathing pattern and no motor response to central pain stimuli. In the terminal or medullary stage, there is slowing of irregular respirations with the pupils becoming widely fixed and dilated. Characteristics on imaging modalities have been described to correspond to physical exam and prognosis.8,9 Measures to reduce intracranial pressure should be quickly employed: the introduction of mannitol and other diuretics, corticosteroids, and surgical excision of the offending lesion. The examination of the neurosurgical patient’s cranial nerves may be done quickly at bedside. Multiple pathologies result in cranial neuropathies. Most commonly, testing is performed on comatose patients as part of a daily physical examination or for brain death. Other instances where cranial nerve function may be of particular interest include Chiari malformations with or without syringobulbia, posterior fossa surgery, cerebellopontine angle surgery, microvascular decompression of the trigeminal nerve, glomus jugulare tumors, and leptomeningeal carcinomatosis. Cranial nerve (CN) examination of the comatose patient includes the pupillary reflex. This utilizes the optic nerve (CN II) as the afferent and the oculomotor nerve (CN III) as the efferent limbs. The existence of differing pupillary diameters is termed anisocoria. Multiple etiologies may result in anisocoria (pupil diameter different by greater than 1 mm), as only the more common will be discussed. Horner’s syndrome consists of unilateral miosis, ptosis, enophthalmos, and anhidrosis. This is caused by a disruption at any point in the sympathetic innervation to the eye. Ptosis and enophthalmos are due to paralysis of Müller’s muscles of the tarsal plates. Anhidrosis is due to sympathetic chain disruption in the carotid sheath. Etiologies are numerous and include Pancoast’s tumor, lower cervical cord lesion, carotid injury/dissection, posterior inferior cerebellar artery (PICA) occlusion (as a part of Wallenberg’s syndrome), and syringobulbia. Adie’s pupil presents as a dilated pupil but responds to parasympathomimetics, such as pilocarpine. It is due to a postganglionic parasympathetic disruption. Marcus-Gunn pupil is also known as an afferent pupillary defect, where the consensual response is more significant than the direct stimulation. This is usually due to a lesion of the optic nerve anterior to the optic chiasm. Argyll-Robertson pupil is an absence of pupillary constriction to direct light stimulation but intact pupillary constriction with convergence. This is typically associated with syphilis. Direct trauma to the orbit may cause a third nerve palsy, but other etiologies should be discarded prior to diagnosis. The trochlear nerve (CN IV) supplies the superior oblique muscle and is an often-injured nerve associated with head trauma. It completely decussates in the superior medullary velum at the level of the inferior colliculus before exiting the brainstem. Its function is not easily tested at the bedside unless the patient is awake and able to follow commands. The trigeminal nerve (CN V) is the largest nerve and exits the midlateral pons to supply sensation to the face, mouth, teeth, eyes, and dura of the anterior and middle fossae (portio major). Motor function is subserved by the motor root (portio minor) supplying the muscles of mastication, tensor veli palatini, tensor tympani, and the anterior belly of the digastric and mylohyoid muscles. The abducens nerve (CN VI) supplies the lateral rectus muscle of the eye. The facial nerve (CN VII) provides innervation to the facial muscles and platysma and taste sensation to the anterior tongue. The vestibulocochlear nerve (CN VIII) provides sensation for sound and balance. Testing of these nerves in an awake patient requires detailed assessment of each testable division of each nerve. In examining the comatose patient, one can examine cranial nerves by testing certain reflexes. Having the patient follow a moving object with only the eyes quickly tests the cardinal eye movements. The pattern is typically in the pattern of a cross. The opportunity may be taken to evaluate for nystagmus or lid abnormalities. Stimulating the lateral junction of the iris and cornea with a wisp of cotton tests the corneal reflex. The afferent limb is CN V, and the efferent limb is CN VII. Patients with intact reflexes will have an associated contraction of periorbital musculature. Oculocephalic (doll’s eyes) and oculovestibular (caloric) reflexes are assessments of cranial nerves III, VI, and VIII. Rotating the patient’s head from side to side tests for doll’s eyes. Examining CN V and VII in a comatose patient involves lightly touching the surface of the cornea with a cotton wisp. Stimulation should be performed at the junction of the sclera and the iris. Care should be taken not to touch the eyelid or lashes, as this will skew the results. Examining an awake patient’s CN V function involves testing fine touch, temperature, and pinprick sensation in all three distributions, as well as motor function, by testing for masseter muscle strength (CN V). Motor function of CN VII to the face is tested by testing the platysma, smiling, pursing lips, closing eyes, and raising eyebrows. Sensation is assessed by taste to the anterior two thirds of the tongue. As with most elements of a neurologic examination, careful attention to motor or sensory loss in typical distributions or asymmetries must be correlated to the patient’s history to guide further work-up, diagnosis, and treatment. The vestibulo-ocular reflex is tested by instilling ~30 to 100 cc of ice water into the external auditory canal (with an intact tympanic membrane), with the head of bed at approximately 30 degrees. Patients with intact function will have a slow, tonic gaze toward the side of stimulation. Those without this reflex continue to stare ahead. This test evokes severe nausea and vomiting in an awake patient. This is most often performed on deeply comatose patients or those with suspected brain death. This can still be done in trauma patients in cases where the cervical spine has not been cleared. Glossopharyngeal (CN IX) and vagus (CN X) nerves can be assessed with the gag reflex. This may be performed in an awake patient by stimulating the posterior pharynx with a tongue blade. In comatose patients, deep bronchial suctioning provides adequate stimulation. Spinal accessory (CN XI) and glossopharyngeal (CN XII) nerves are testable only in awake patients. Their function should be noted for patients with glomus jugulare tumors or lesions at the foramen magnum. Examination of the motor and sensory systems requires in-depth understanding of cortical, brainstem, and spinal cord neuroanatomy and physiology. NICU patients typically have derangements in either of these systems. Patients with spinal cord injury, or postoperative fusion patients should have frequent detailed examinations. An early intervention for a patient with a developing epidural hematoma may return the patient to his or her former level of activity. Likewise, postoperative aneurysm-clipping patients with vasospasm who develop subtle weakness should have their hyperdynamic therapy amplified to ward off additional ischemia. As with peripheral nerve injury, a detailed survey of the sensorimotor systems usually will localize the lesion. The sensation exam should include several modalities to test several tracts of the cord. A proper examination should test dorsal column function (joint position, two-point discrimination, and vibratory sensation) and spinothalamic tract (pain and temperature). Sacral sparing is also of great importance to help determine the completeness or incompleteness of a spinal cord injury. The peripheral sensory nerves come off the spinal cord in precise, but irregular, distributions or dermatomes. Knowing these dermatomes is critical for localizing injury to a peripheral nerve and/or the spinal cord (Fig. 2–1). Standard documentation of motor examination is necessary for reliability between examiners. The Royal Medical Research Council of Great Britain developed a standard scale used throughout the world (Table 2–3). Motor examination should also include testing of muscle tone. Upper motor neuron lesions typically have increased tone. Increased tone may be present in patients in an unexplained coma or sudden deterioration with no clear etiology, and silent status epilepticus should be excluded (Table 2–4).
Initial Assessment
2
Bedside Exam in the Neurosurgical Intensive Care Unit
 The Power of Observation
The Power of Observation
 Level of Consciousness
Level of Consciousness
 Cranial Nerves
Cranial Nerves
 Sensorimotor
Sensorimotor
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree