![]() Identifying the presence or absence of cardiac activity in cardiac arrest
Identifying the presence or absence of cardiac activity in cardiac arrest
![]() Identifying the presence or absence of pericardial effusion and differentiating from pleural effusion
Identifying the presence or absence of pericardial effusion and differentiating from pleural effusion
![]() Identifying the presence or absence of cardiac tamponade
Identifying the presence or absence of cardiac tamponade
![]() Assessing regional wall motion abnormalities in the diagnosis of myocardial infarction
Assessing regional wall motion abnormalities in the diagnosis of myocardial infarction
![]() Assessing right ventricular size and function in cases suspicious for pulmonary embolism
Assessing right ventricular size and function in cases suspicious for pulmonary embolism
CONTRAINDICATIONS
![]() None: No contrast or radiation involved
None: No contrast or radiation involved
PROBE SELECTION AND IMAGING
![]() Use a standard 2.0- to 5.0-MHz microconvex or phased-array probe
Use a standard 2.0- to 5.0-MHz microconvex or phased-array probe
![]() At least two of the four views of the heart are required for diagnosis and billing
At least two of the four views of the heart are required for diagnosis and billing
![]() Orient the probe marker to the top left of the screen
Orient the probe marker to the top left of the screen
![]() Methods of enhancing image acquisition include the following:
Methods of enhancing image acquisition include the following:
![]() Keep the complete ultrasound probe in contact with the chest wall and angle, rotate, and tilt the ultrasound probe as necessary
Keep the complete ultrasound probe in contact with the chest wall and angle, rotate, and tilt the ultrasound probe as necessary
![]() Use an adequate amount of gel during bedside echocardiography
Use an adequate amount of gel during bedside echocardiography
![]() Try alternative cardiac echocardiography views
Try alternative cardiac echocardiography views
![]() Turn the patient in the left lateral decubitus position to bring the heart closer to the anterior chest wall
Turn the patient in the left lateral decubitus position to bring the heart closer to the anterior chest wall
LANDMARKS: FOUR STANDARD VIEWS
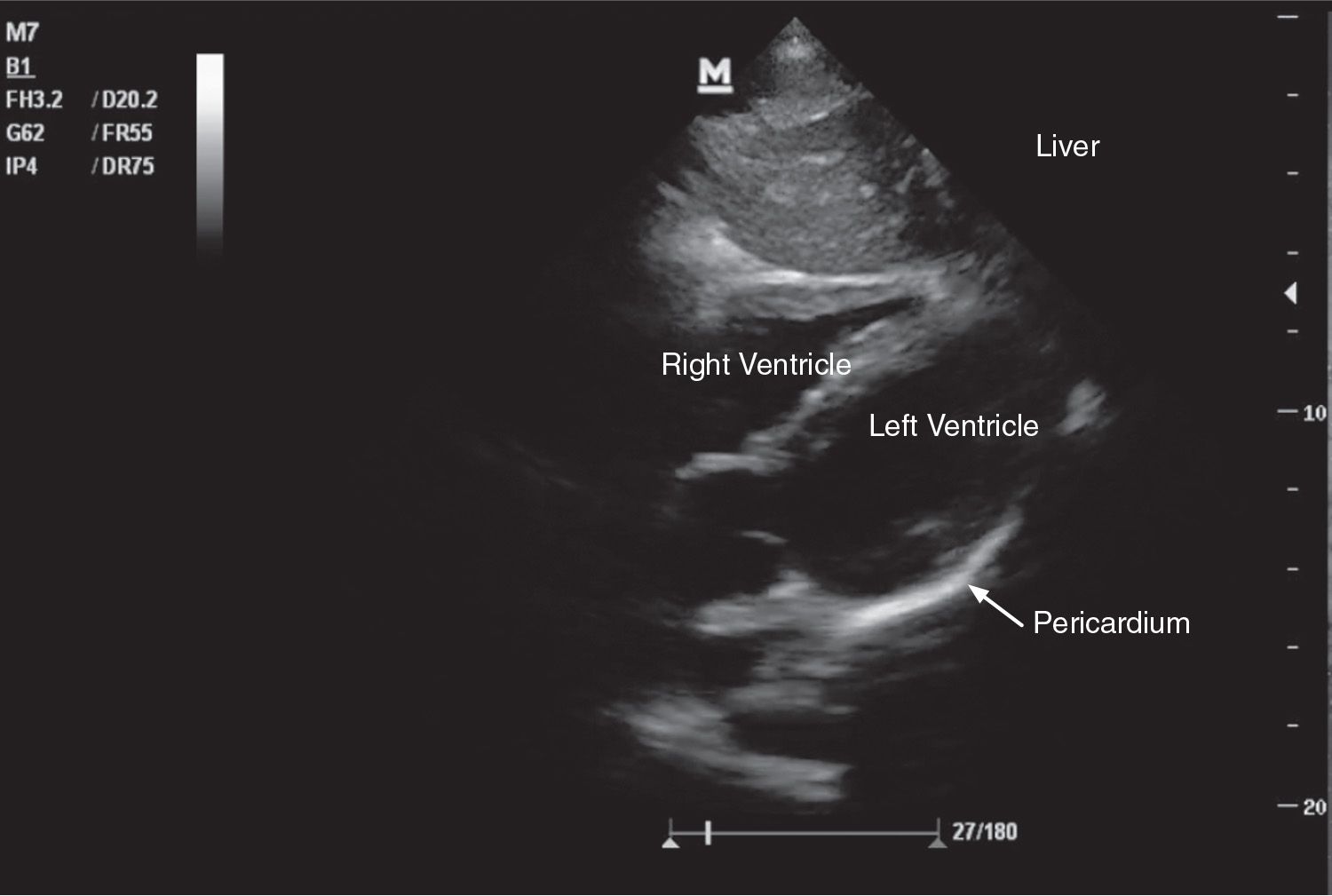
![]() Subxiphoid (Sx) View: (FIGURE 11.1)
Subxiphoid (Sx) View: (FIGURE 11.1)
![]() Place the probe in Sx position of abdomen, facing toward the patient’s left shoulder, with the probe marker toward the patient’s right
Place the probe in Sx position of abdomen, facing toward the patient’s left shoulder, with the probe marker toward the patient’s right
![]() If the heart is not adequately viewed, move the probe to the patient’s right using the liver as an acoustic window. Asking the patient to take a deep breath will push the heart inferior toward the probe
If the heart is not adequately viewed, move the probe to the patient’s right using the liver as an acoustic window. Asking the patient to take a deep breath will push the heart inferior toward the probe
![]() A moderate amount of pressure may be required for optimal viewing; however, this view is limited by body habitus and pain
A moderate amount of pressure may be required for optimal viewing; however, this view is limited by body habitus and pain
![]() This view’s utility is predominantly to assess for cardiac activity or pericardial effusion in the setting of trauma (as a part of the focused abdominal sonography for trauma [FAST] examination)
This view’s utility is predominantly to assess for cardiac activity or pericardial effusion in the setting of trauma (as a part of the focused abdominal sonography for trauma [FAST] examination)
![]() Parasternal Long (PSL) View: (FIGURE 11.2)
Parasternal Long (PSL) View: (FIGURE 11.2)
![]() Place the probe just left of the sternum in the third/fourth intercostal space and directed toward the patient’s heart, with the probe marker directed toward the patient’s left elbow
Place the probe just left of the sternum in the third/fourth intercostal space and directed toward the patient’s heart, with the probe marker directed toward the patient’s left elbow
![]() This view should be your main view—other views can be obtained by slight changes in probe positioning from here
This view should be your main view—other views can be obtained by slight changes in probe positioning from here
![]() A proper PSL view requires the apex of the left ventricle (LV), the mitral valve, and the aortic valve to be in view
A proper PSL view requires the apex of the left ventricle (LV), the mitral valve, and the aortic valve to be in view
![]() Just deep to the posterior pericardium is the descending aorta
Just deep to the posterior pericardium is the descending aorta
![]() In this view you can assess regional wall motion, valve function, septal movement, and proximal aorta size, and differentiate pericardial effusion from pleural effusion
In this view you can assess regional wall motion, valve function, septal movement, and proximal aorta size, and differentiate pericardial effusion from pleural effusion
![]() Parasternal Short-Axis (PSA) View: (FIGURE 11.3)
Parasternal Short-Axis (PSA) View: (FIGURE 11.3)
![]() From a PSL view, rotate the probe 90 degrees clockwise (toward the patient’s right hip)
From a PSL view, rotate the probe 90 degrees clockwise (toward the patient’s right hip)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree